Abstract
Purpose
To describe a case of unilateral corneal keloid and present the clinical and histopathological findings and the management.
Methods
A 23-year-old Asian male patient was examined for a white spot on the left cornea that had been present since birth. On biomicroscopic examination, a well-demarcated vascularized corneal mass was found located nasal to the center. The pupil was displaced superiorly, and gonioscopic examination showed peripheral iridocorneal adhesion at 12 o'clock. The patient underwent penetrating keratoplasty.
Results
Histopathologic study showed a variously thickened epithelial layer, an absence of Bowman's layer, subepithelial fibrovascular hyperplasia, and an absence of dermal elements. These histopathologic findings suggested a congenital corneal keloid. The central graft cornea remained clear at 18 months after surgery and the patient was satisfied with the result.
Clinically corneal keloids appear as gray-white elevated masses diffusely involving the entire stroma or as localized solitary nodules.1-3 Such masses are usually avascular,3,4 but some of them were reported as vascularized and white.5,6 These lesions often develop after penetrating or non-penetrating corneal traumas, surgeries, or corneal inflammations.7-9 However, some cases of corneal keloids were not associated with any ocular trauma,4,10 but were rather present from birth.3,5,11
Surgical results of congenital corneal keloids have been very poor thus far. One case of congenital keloids occurred bilaterally in a child with Rubinstein-Taybi syndrome. In spite of repeated penetrating keratoplasties, the reconstruction of the anterior segment was unsuccessful.5 In other congenital cases, the eyes were eventually enucleated due to spontaneous corneal perforation or buphthalmos.3,11
We describe a case of unilateral congenital corneal keloid and present the clinical and histopathologic findings and the management.
A 23-year-old Asian man was examined for a white spot on the left cornea. He had been delivered by vaginal birth at full-term after an uncomplicated pregnancy. According to his mother, he had had the white spot on his left cornea since birth. He had no history of traumatic or inflammatory events. He had no keloids on his skin. His medical and family histories were unremarkable. His uncorrected visual acuity was 20/1000 in the left eye and 20/20 in the right eye; the left eye could not be corrected.
Biomicroscopic examination revealed a well-demarcated round corneal mass located nasal to the center (Fig. 1A). The diameter of the real mass was 4 mm and the cornea surrounding the mass was severely edematous. The total diameter of the corneal lesion was about 5.2 mm, and the lesion occupied about 90 percent of the stromal thickness. The mass was highly vascularized and had a white glistening appearance. The pupil was displaced superiorly, and gonioscopic examination showed peripheral iridocorneal adhesion at 12 o'clock (Fig. 1B). Goldman tonometry showed an intraocular pressure of 12 mmHg in the left eye. The remainder of the ophthalmologic examination was within normal limits. Anterior segment fluorescein angiography showed a single large vessel supplying the mass lesion in the early period (Fig. 2A) and profuse leakage from the vascular network within the mass in the late period (Fig. 2B). Based on the clinical appearance of the lesions, a presumptive diagnosis of corneal dermoid was made. Since the corneal mass had existed since birth, the possibility of vision improvement was deemed to be rare. Nevertheless, the patient and his mother were eager to have surgery for cosmetic reasons.
The patient underwent a penetrating keratoplasty on his left eye. In order to excise the entire corneal mass, a slightly eccentric trephination was performed. After trephination of a 7.5 mm corneal button, a 7.75 mm donor corneal graft was secured with interrupted and single continuous sutures.
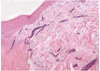
The corneal button obtained during surgery was fixed in 3% formalin solution for light microscopy. Examination of the paraffin sections stained with hematoxylin and eosin showed a variously thickened epithelial layer and localized subepithelial fibrovascular proliferation. Slight pigmentation was present in the basal epithelial layer and the Bowman's layer was absent. The stroma was thickened with a disruption of normal lamellar pattern (Fig. 3). Other special staining with periodic acid-Schiff, Masson's trichrome and congo red showed no abnormal deposition. No dermal appendage was evident. The pathologic diagnosis of a corneal keloid was made.
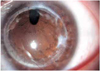
The postoperative course was uneventful. Two months after surgery, his best corrected visual acuity (BCVA) was slightly improved to 20/400. Some superficial corneal scars appeared along with corneal sutures and a moderately sized leukoma occurred at the 3 o'clock position 3 months after the surgery. However, the scars did not progress further (Fig. 4). The patient was satisfied with the surgical results. The graft cornea remained clear centrally at the time of writing at 18 months after surgery.
The pathogenesis of corneal keloid is not yet fully understood. Although most cases of corneal keloid have been associated with a previous corneal injury, some reported cases had no previous history of trauma as seen in congenital corneal keloid.3-5,10,11
The pathogenesis of dermal keloids suggested by Murray was that a mechanical stimulus triggers a cellular response with an inflammatory reaction, including vasodilation, edema and immature fibroblast recruit. This reaction is followed by a biochemical stimulus that induces blood vessel regression, myofibroblast proliferation and subsequent scar retraction. At some point, a stimulus induces excessive growth that leads to an exaggerated increase in cellularity and metabolic activity which favors the invasion of the surrounding tissue's healthy borders by the scar.12
In corneal keloids, however, various theories have been suggested. Some authors considered the stromal cells of an incarcerated iris after corneal perforation as a cause of corneal keloid formation.11 Conversely, others suggested that the corneal keloid originates from the corneal stroma itself and its defect of corneal reparative process.13 One theory is that subclinical corneal infections stimulate an excessive repair process by leaving intrastromal antigens and form a corneal keloid.10 Cibis et al1 suggested that amino acid or other noxious substances from the new leaky corneal vessels induce excess fibrous tissue proliferation and keloid formation. In the case of congenital corneal keloid with no history of corneal trauma, the failure of normal differentiation of corneal tissue during embryogenesis has been proposed as the mechanism of keloid formation.14 Rao et al5 reported that congenital corneal keloid was associated with anterior segment dysgenesis in Rubinstein-Taybi syndrome. Our patient showed a distorted pupil and iridocorneal adhesion at 12 o'clock but no cataract or angle structure abnormality. This observation may support the hypothesis that congenital corneal keloids are caused by failure of normal differentiation of the anterior segment.
Histopathologic study of our patient showed a variously thickened epithelial layer subepithelial fibrovascular hyperplasia, an absence of Bowman's layer, irregularly arranged stromal collagen fibers, and an absence of dermal elements. In previous reports these have been considered pathognomonic of a corneal keloid.8,14-16 Although we did not observe activated fibroblasts on electron microscopy, the postoperative occurrence of superficial leukoma might support the diagnosis of corneal keloid.
Most of the earlier reports about the vascularization of corneal keloid described the vessels to be located in the anterior part of the keloid mass, or to be diffusely spread but with more vessels located anteriorly.1,13,16,17 In this case, the major feeding vessel and the branches were also located in the anterior portions of the keloid stroma. Anterior segment fluorescein angiography showed profuse leakage from the vascular network. Shoukrey et al7 observed the thickened basal lamina of the vessels in the keloid and this was thought to reflect a high turnover of the vascular endothelium, leading to a degenerative event and enhancing edema. The anterior segment angiographic findings of our patient were consistent with the tendency for leakage and edema of the corneal keloids.
The surgical results of treatment for corneal keloids have differed widely. Some older patients were simply treated by superficial lamellar keratectomy. The lesions separated easily from the remaining cornea and there was no recurrence of the corneal keloid.6,7 Some other cases deteriorated after superficial lamellar keratectomy, but were successfully treated with lamellar keratoplasty or penetrating keratoplasty. 4,10 However, the surgical results of congenital corneal keloids have been unsatisfactory. Multiple penetrating keratoplasties were unsuccessful in the reconstruction of the anterior segment and some eyes were even enucleated because of spontaneous corneal perforation or buphthalmos.3,5,11 The patient in the present case report had congenital corneal keloid, but he had gone 23 years without any surgical intervention. Although his vision did not improve significantly after penetrating keratoplasty, the surgical result was cosmetically acceptable and the patient was therefore satisfied. Irrespective of the surgery performed, the most important factor related to the surgical result might be the age of the patient at surgery.
In conclusion, this case of congenital corneal keloid without any history of trauma was diagnosed by clinical and histopathologic study. The management of congenital corneal keloid by penetrating keratoplasty may be an effective surgical option in young adult patients.
Figures and Tables
Fig. 1
(A) A well-demarcated vascularized round mass is located slightly nasal to the center on the left cornea. (B) Gonioscopic examination shows peripheral iridocorneal adhesion at 12 o'clock.
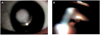
Fig. 2
Anterior segment fluorescein angiographic findings. (A) A single large vessel supplying the mass lesion appears in the early period. (B) Profuse leakage from the vascular network within the mass is shown in the late period.

References
1. Cibis GW, Tripathi RC, Tripathi BJ, Harris DJ. Corneal keloid in Lowe's syndrome. Arch Ophthalmol. 1982. 100:1795–1799.
2. Lahav M, Cadet JC, Chirambo M, et al. Corneal keloids -a histopathological study. Graefes Arch Clin Exp Ophthalmol. 1982. 218:256–261.
3. O'Grady RB, Kirk HQ. Corneal keloids. Am J Ophthalmol. 1972. 73:206–213.
4. Mejia LF, Acosta C, Santamaria JP. Clinical, surgical, and histopathologic characteristics of corneal keloid. Cornea. 2001. 20:421–424.
5. Rao SK, Fan DS, Pang CP, et al. Bilateral congenital corneal keloids and anterior segment mesenchymal dysgenesis in a case of Rubinsein-Taybi syndrome. Cornea. 2002. 21:126–130.
6. Bourcier T, Baudrimont M, Boutboul S, et al. Corneal keloid: Clinical, ultrasonographic, and ultrastructural characteristics. J Cataract Refract Surg. 2004. 30:921–924.
7. Shoukrey NM, Tabbara KF. Ultrastructural study of a corneal keloid. Eye. 1993. 7:379–387.
8. Risco MJ, Huaman A, Antonios SR. A case of corneal keloid: clinical, surgical, pathologic and ultrastructural characteristics. Br J Ophthalmol. 1994. 78:568–571.
9. Mullaney PB, Teichmann K, Huaman A, Heinz G. Corneal keloid from unusual penetrating trauma. J Pediatr Ophthalmol Strabismus. 1995. 32:331–334.
10. Holbach LM, Font RL, Shivitz IA, Jones DB. Bilateral keloid-like myofibroblastic proliferations of the cornea in children. Ophthalmology. 1990. 97:1188–1193.
11. Farkas TG, Znajda JP. Keloid of the cornea. Am J Ophthalmol. 1968. 66:319–323.
12. Murray JC. Scars and keloids. Dermatol Clin. 1993. 11:697–708.
13. Fenton RH, Tredici TJ. Hypertrophic corneal scars (keloids). Surv Ophthalmol. 1964. 9:561–566.
14. Weiner MJ, Albert DM. Congenital corneal keloid. Acta Ophthalmol (Copenh). 1989. 67:188–196.
15. Brown SI. Corneal transplantation of the infant cornea. Trans Am Acad Ophthalmol Otolaryngol. 1974. 78:461–466.
16. Smith HC. Keloid of the cornea. Trans Am Ophthalmol Soc. 1940. 38:519–538.
17. Frederique G, Howard RO, Bonuik V. Corneal ulcers in rubeola. Am J Ophthalmol. 1969. 68:996–1003.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download