Abstract
Methods
We retrospectively analyzed the 78 DRS cases that presented to our department between 1995 and 2004. The clinical features investigated included sex distribution, laterality, type of presentation, deviation in primary position, anomalous vertical movements, face turn, amblyopia and anisometropia.
Results
There were 38 (48.7%) affected males and 40 (51.3%) females. Left eye predominance (83.3%) was observed, as was type I presentation (85.9%). Orthotropia was found to be the most common primary position in 46 cases (59.0%). Face turn in unilateral DRS was noted in 13 patients (17.1%). There were 6 cases (7.7%) with anisometropia and 4 (5.1%) with amblyopia.
Duane's retraction syndrome (DRS) is a congenital ocular motility disorder characterized by marked limitation or absence of abduction, restriction of adduction, retraction of the globe, narrowing of the palpebral fissure on adduction, and frequent association with elevation or depression on adduction. This characteristic retraction of the globe is thought to be caused by a branch of the oculomotor nerve innervating the lateral rectus muscle and subsequent co-contraction of the ipsilateral lateral rectus muscle upon oculomotor nerve firing. Three types of DRS have been described by Huber.1 Type I is characterized by a severe limitation of abduction with normal or slight limitation of adduction and is mostly esotropia in the primary position if strabismus is present. In type II, this is a less marked limitation of abduction and significant limitation of adduction and exotropia is more frequent in the primary position if strabismus is present. Type III is characterized by orthotropia in the primary position and marked limitation of abduction and adduction.
Only few reports have investigated DRS patients in Korean patients until now.2-3 However, various studies have described clinical features and distributions of DRS in different ethnic groups and countries.4-10
This report describes the clinical features of DRS in Korean patients and compares how closely these cases conform to the classic concepts and descriptions.
In this retrospective study, we reviewed the records of 78 consecutive DRS cases presenting to Kim's Eye Hospital between 1995 and 2004. The clinical features analyzed included age at diagnosis, sexual distribution, laterality, type of presentation, deviation at primary position, anomalous vertical movements, face turn, refractive error, amblyopia and anisometropia. Age at first visit, gender, chief complaints, and past medical history were recorded in all cases. All patients underwent a detailed eye examination, including visual acuity determination, manifest and cycloplegic refraction, alternative cover test, duction and version testing, intraocular pressure (IOP) measurement by noncontact tonometry, slit-lamp biomicroscopy and fundus examination.
The clinical type of DRS according to Huber's classification was recorded. The ocular deviation in the primary position of gaze was determined by Hirschberg or Krimsky prism test. Amblyopia was defined as best corrected visual acuity of 20/30 or less in either eye and anisometropia was defined as a difference in cycloplegic spherical equivalent greater than 2.0 diopters (D) between the two eyes. Patients with other non-ocular anomalies or a history of previous ocular surgery, including strabismus correction, were excluded.
Among the 78 cases, the average age at first visit was 9.0 years (2-25 years).
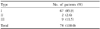
There were 38 (48.7%) affected males and 40 (51.3%) females. The left eye was involved in 65 patients (83.3%) and the right in 11 (14.1%) of the unilateral cases. Two patients (2.6%) showed bilateral involvement (Table 1). There was no significant sex predilection found among the DRS cases in this study; however, laterality showed a left predominance.
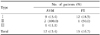
Based on the Huber's classification, of the 78 affected patients (80 eyes), 67 (85.9%) were classified as type I DRS, 2 (2.6%) as type II, and 9 (11.5%) as type III (Table 2). Both bilateral cases were type I.
Horizontal alignment in the primary position was determined in all patients. Orthotropia occurred in the majority with 46 patients (59.0%), followed by exotropia in 18 patients (23.1%), and esotropia in 14 (17.9%). Vertical strabismus of hypertropia was associated with exotropia in 3 patients (3.8%), and with esotropia in 2 (2.6%). More than half of those classified as type I were orthotropic and orthotropia was the predominating alignment among type III patients. Both individuals with bilateral DRS were esotropic. Those with type I and III (57.7%) tended to be orthotropic (Table 3).
Anomalous vertical movements, including upshoots and downshoots which are a prominent feature of DRS, were found in 12 cases (15.4%): 9 (13.4%) of 67 type I patients, both (100.0%) of 2 type II patients and 1 (11.1%) of 9 type III patients (Table 4).
Face turn in unilateral DRS occurred in 13 eyes (17.1%): 12 (18.5%) type I cases, one (50.0%) type II case and zero (0%) type III cases (Table 4). The esotropic patients with DRS turned their face toward the affected eye while the exotropic patients with DRS turned theirs away from the affected eye, except in 1 case (Table 5). The direction of the face turn was toward the affected eye in 9 cases and away from the affected eye in 4 cases (Table 5). To determine possible etiologies for face turns in primary orthotropia, the association of face turn with upshoots and downshoots in unilateral DRS was examined (Table 6).
Among 78 patients who underwent cycloplegic refraction, 14 cases (18.0%) were emmetropic, 33 (42.3%) were hypermetropic and 31 (39.7%) were myopic. Six cases (7.7%) were anisometropic and 4 (5.1%) amblyopic.
DRS reported among the white population is usually a sporadic syndrome with a unilateral predominance for the left side and with a slight female predominance. In most cases the abducens nucleus and nerve are absent or hypoplastic, and the lateral rectus muscle is innervated by a branch of the oculomotor nerve. However, there may also be contributing mechanical abnormalities.11
In our study, most of the 78 patients complained of limitation of ocular movement, ocular deviation and abnormal head position. The average age of first visit was 9 years old.
The proportion of males (48.7%) and females (51.3%) was similar in our study, which is in contrast to the female predominance of previous reports by Duane,12 Kirkham13 and Raab,14 but similar to that by Zhang15 who also reported no definite sex predilection. Considering Zhang's study of 201 Chinese DRS patients, it is suggested that DRS patients of Korean decent might share similar characteristics with those of Chinese decent.
Also, our findings corroborate Lee and Chang's study3 which reported 46 Koreans with DRS. In the literature the predilection for left eye affliction is three to one.16 In this study, the left eye predominance was even greater at 65 of 78 cases (83.3%). The 2 cases (2.6%) of bilateral DRS in our study presented a lower occurrence rate than that previously reported for Koreans (4.0%) or Caucasians (10-23%), which suggests that bilateral involvement in DRS is rarely found in Koreans.
According to Huber's classification, Raab14 reported 70 DRS cases, among which there were 73% type I, 1% type II, and 26% type III. Lee and Chang3 also reported that type I was the most common type (96%) among Korean DRS, with the incidence of types II and III being only 2% each. In our series, 67 (85.9%) of 78 patients were type I, 2 (2.6%) were type II, and 9 (11.5%) were type III. These results are similar to previous Caucasian studies but different from a previous Korean study.2,3 As the extent of adduction recorded could be dependent on the subjective judgement of the examiner, we cannot clearly exclude the possibility of misdiagnosis in this case.
Many patients with DRS appeared to have strabismus in the primary position. Patients might adopt a small, unnoticed, head position movement which could obscure a small angle strabismus in the primary position in order to achieve binocular single vision. Among the 85 patients with unilateral DRS reported by Isenberg and Urist,4 24 (28.0%) were esotropic, 25 (29.0%) were exotropic, and 36 (43.0%) were orthotropic. All type I patients with strabismus were esotropic. Zhang15 reported that exotropia was the most common deviation in the primary position (35.8%), followed by orthotropia (32.3%) and esotropia (25.4%), in 201 Chinese patients. Among 46 Korean patients reported by Lee and Chang,3 27 (59.0%) were esotropic, 9 (20.0%) were exotropic, and 10 (21.0%) were orthotropic. In our study, orthotropia was the most common (46 patients, 59.0%) in the primary position, followed by 18 exotropic patients (23.1%), and 14 esotropic patients (17.9%). This result most closely corresponds with Isenberg and Urist's report with Caucasian subjects that orthotropia is most common, with the ratio between esotropia and exotropia being similar. Moreover, our findings were different from Lee and Chang's and Zhang's studies of Asians, which suggests that there might be regional, as opposed to merely racial, differences. More research is needed to examine these differences.
The occurrence of face turn, a major characteristic of this entity, is usually attributed to maintenance of straight eyes and fusion. For face turn and anomalous vertical movements of DRS eyes, Raab14 reported 35% and 25%, Zhang15 40% and 20%, and Lee and Chang3 77% and 48%, respectively. In our study, face turn in unilateral DRS were found in 13 cases (16.7%) and anomalous vertical movements, including upshoots and downshoots in the adduction position, in 12 cases (15.4%). The fact that orthotropia was the most common primary position in Korean DRS patients could explain this different occurrence rate.
Most unilateral DRS patients who showed esotropia and exotropia were found to have face turn, which is a mechanism of maintaining binocular single vision whereby the face is turned toward the direction of the horizontal muscle with the greatest deficit. Our study revealed this tendency, as had many other Caucasian and Asian studies.2-4,14-15 The esotropic patients with DRS turned their face toward the affected eye while the exotropic patients with DRS turned theirs away from the affected eye, except in 1 case. Nevertheless, 13.0% of primary position orthotropic patients had face turn. Therefore, other possible explanations for face turn, as well as maintenance of fusion, cannot be excluded.
Regarding the relationship of face turn in primary orthotropia with upshoots and downshoots in unilateral DRS, 4 (66.7%) of the orthotropic DRS cases exhibited face turn toward the side of limited abduction, affected eye. However, two cases (33.3%) with severe upshoots and downshoots tended to turn their faces away from the side of vertical deviation.
In our study, we found emmetropia in 14 cases (18.0%), hypermetropia in 33 (42.3%), and myopia in 31 (39.7%). Zhang15 reported emmetropia in 50.0% of patients, hypermetropia in 35.6%, and myopia in 11.0%.
Various reports have compared the occurrence rate of amblyopia in the general population with that in DRS. In our study, there were 4 cases (5.1%) with amblyopia, compared to 4 of 46 (8.0%) for Lee and Chang,2 and 40 of 118 (33.9%) for Zhang.15 Only Zhang's criteria of amblyopia, defined as a best corrected visual acuity of 20/25 or less in either eye, was different from that of other studies. Thus, no significant difference was found in the occurrence rate of amblyopia between DRS patients and the general population.
In conclusion, although most clinical manifestations of DRS in this study corresponded with previous studies among Caucasians and Asians, the male/female distribution rate and Huber's classification were different from Caucasian studies but similar to Asian ones. Further research is necessary into the racial and regional differences found in clinical features of DRS.
Figures and Tables
References
1. Huber A. Electrophysiology of the retraction syndrome. Br J Ophthalmol. 1974. 58:293–300.
2. Shin WB, Roh YB. Analysis of abnormal head posture and surgical results in the patients with Duane's retraction syndrome. J Korean Ophthalmol Soc. 1998. 39:393–399.
3. Lee KH, Chang BL. Clinical characteristics of Duane's retraction syndrome. J Korean Ophthalmol Soc. 1996. 37:1747–1752.
4. Isenberg S, Urist MJ. Clinical observations in 101 consecutive patients with Duane's retraction syndrome. Am J Ophthalmol. 1977. 84:419–425.
5. Kirkham TH. Duane's syndrome and familial perceptive deafness. Br J Ophthalmol. 1969. 53:335–339.
6. Maruo T, Kubota N, Arimoto H, Kikuchi R. Duane's syndrome. Jpn J Clin Ophthalmol. 1980. 34:845–854.
7. Mehel E, Quere MA, Lavenant F, Pechereau A. Aspects epidemiologiques et cliniques de syndrome de Stilling-Turk-Duane. J Fr Ophthalmol. 1996. 19:533–542.
8. Pfaffenbach DD, Cross HE, Kearns TP. Congenital anomalies in Duane's retraction syndrome. Arch Ophthalmol. 1972. 88:635–639.
9. Ro A, Gummeson B, Orton RB, Cadera W. Duane's retraction syndrome. Southwestern Ontario experience. Can J Ophthalmol. 1989. 24:200–203.
10. Riordan-Eva P, Vickers SF, McCarry B, Lee JP. Cyclic strabismus without binocular function. J Pediatr Ophthalmol Strabismus. 1993. 30:106–108.
11. Alexandrakis G, Saunders RA. Duane retraction syndrome. Ophthalmol Clin North Am. 2001. 14:407–417.
12. Duane A. Congenital deficiency of abduction associated with impairment of adduction, retraction movements, contraction of the palpebral fissure and oblique movements of the eye. Arch Ophthalmol. 1905. 34:133–159.
13. Kirkham TH. Inheritance of Duane's syndrome. Br J Ophthalmol. 1970. 54:323–329.
14. Raab EL. Clinical features of Duane's syndrome. J Pediatr Ophthalmol Strabismus. 1986. 23:64–68.
15. Zhang F. Clinical features of 201 cases with Duane's retraction syndrome. Chin Med J. 1997. 110:789–791.
16. DeRespinis PA, Caputo AR, Wagner RS, Guo S. Duane's retraction syndrome. Surv Ophthalmol. 1993. 38:257–288.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download