Abstract
Purpose
To present a case of a unilateral diffuse retinal hemorrhage in a 15-year-old girl, who underwent bilateral trabeculectomy for steroid induced glaucoma.
Methods
Despite the maximally tolerable medical treatment, IOP in the right eye remained above 50 mmHg for four months, and was simultaneously elevated in the left eye. So we performed bilateral trabeculectomy.
Results
On the first postoperative day, diffuse retinal hemorrhages were observed in the right eye; however, no retinal hemorrhage was found in the left eye. The hemorrhages resolved completely without consequences two months later.
Conclusions
In the case of high IOP for a long period, sudden lowering of IOP may acutely increase the blood flow and consequently rupture multiple retinal capillaries because of altered autoregulatory function. Special care is therefore needed to prevent an abrupt fall in IOP before, during, and after surgery, especially when IOP has been highly elevated for an extended period.
Several cases of choroidal hemorrhage after glaucoma iltration surgery have been reported in the literature,1-7 but retinal hemorrhage as a complication of glaucoma surgery is relatively rare. We describe a case of diffuse retinal hemorrhages that occurred in only one eye after bilateral glaucoma filtration surgery and the possible mechanism of the hemorrhages is also discussed.
A 15-year-old Korean girl was transferred to our department in February 2003. She had a history of systemic and topical steroid treatment for uveitis in both eyes since August 2002 but had shown a poor clinical response. Initial visual acuity on presentation was 20/25 (with -8.00 diopters), and the intraocular pressure (IOP) was 19 mmHg in both eyes. Inflammatory cells were found in the anterior chamber, and 'snowball and snow bank' was observed in the vitreous cavity. No remarkable findings were noted on her general systemic evaluation, and she did not have a history of taking aspirin or any other medication that might promote bleeding. Topical and subtenon steroids were used to control the ocular inflammation in both eyes, but only after repeating temporary stabilization followed by recurrence of the inflammation. Anterior chamber inflammation and the snowball and snow bank of the vitreous cavity were controlled during August 2003. However, in the following month IOP began to increase to over 30 mmHg in the right eye (OD), and also in the left eye (OS) two months later. IOP remained above 50 mmHg for four months in the right eye and above 40 mm Hg for one month in the left eye despite maximally tolerated medical therapy. How-ever in November 2003 a glaucomatous visual field defect began to develop and cup-disc ratios 0.6 in both eyes. Patient complained side effects of medication such as tingling sensation and general weakness.
Trabeculectomy was performed OD on January 15, 2004 and OS on January 22, 2004. Preoperative visual acuity was 20/20 in both eyes, and IOP was 56 mmHg OD and 48 mmHg OS. The trabeculectomies with mitomycin-C were performed under general anesthesia. After a fornix-based, conjunctival incision with a partial-thickness, scleral flap dissection, a cellulose sponge soaked with mitomycin-C (0.2 mg/mL) was applied twice to the wound bed for 30 seconds each time. Sclerostomy was performed and a peripheral iridectomy created. Two releasable sutures were made to secure the scleral flap with 9-0 prolene. The tenon and conjunctiva were then also sutured with 9-0 prolene. The surgery including intubation and extubation of the endotracheal tube was uneventful.
On the first postoperative day, IOP was 16 mmHg and the corrected visual acuity was 20/50. Slit lamp biomicroscopic examination showed a diffusely raised, functioning, filtering bleb (Fig. 1) and a deep and well-formed anterior chamber, but fundus examination revealed diffuse, superficial and deep retinal hemorrhages on the posterior pole and peripheral fundus (Fig. 2A). Some of the hemorrhages showed whitish spots in the center. Fluorescein angiography was performed and showed multiple, blocked fluorescence due to the retinal hemorrhages, but normal blood circulation without any obstruction of the blood flow (Fig. 2B). The left eye underwent the same surgical procedure one week later. On the first postoperative day, IOP was 9 mmHg and the corrected visual acuity was 20/25 for the left eye. No remarkable retinal abnormality was found in the left eye. One month postoperatively, IOP was stable in the range of 8 to 12 mm Hg in both eyes, and visual acuity improved to 20/20 in the right eye with further resolution of the retinal hemorrhages. About two months later the retinal hemorrhages in the right eye disappeared completely (Fig. 2C).
White-centered, retinal hemorrhages have since been described in patients with hemorrhage retinopathy caused by several systemic and ocular conditions, including leukemia, intracranial hemorrhage, anoxia, profound anemia, hypertensive and diabetic retinopathy, neonatal birth trauma, and shaken-baby syndrome.8-13 Usually retinal capillaries are impermeable14 but certain conditions such as those listed above can result in anoxic insult or sudden elevation of venous pressure, thereby rupturing the thin capillary wall in multiple foci and resulting in multiple, white-centered hemorrhages.15
Retinal hemorrhages after glaucoma surgery are relatively rare.16-20 Fechtner et al indicated that a sudden lowering of IOP can increase retinal and choroidal blood flow, thereby overwhelming the capacitance of the capillary bed and causing multiple focal endothelial leaks. Fechtner et al also indicated that the presence of a fibrin center in the deep hemorrhages would be consistent with this. In contrast to the choroidal vascular bed, the retinal vasculature has been assumed to have autoregulation.21-23 Autoregulation has also been defined as the tendency of blood flow to remain constant in the face of changes in perfusion pressure.24 Using this definition, Riva et al21 concluded that autoregulation was still effective at a perfusion pressure (P) as low as 10 mmHg with IOP of about 42 mmHg. At P=10 mmHg, the regulatory response is only one third as efficient as that at P=30 mmHg with IOP of about 22 mmHg. Glaucomatous eyes are known to have abnormal retinal blood flow autoregulation,25,26 which may contribute to the development of retinal hemorrhage because a sudden lowering of IOP can induce an abrupt increase in blood flow in the retinal artery, resulting in rupture of the thin retinal capillary wall.
Our patient was a young woman who developed diffuse retinal hemorrhages in only one eye following bilateral trabeculectomy performed after a longstanding period of increased IOP.
Bleeding was not observed in the other eye which had not undergone such extended or substantial IOP elevation. We therefore concluded that the cause of the retinal hemorrhages was the sudden lowering of IOP which acutely increased the blood flow and then ruptured multiple, retinal capillaries of the altered autoregulatory function due to the extended period of elevated IOP, as was reported by Fechtner et al for cases of ocular decompression retinopathy.17
Suzuki et al reported several cases of retinal bleeding after glaucoma surgery and classified them into three categories: a small hemorrhage sometimes seen in the peripheral fundus that may be overlooked by ophthalmologists if the pupil is not dilated; massive but benign bleeding or decompression retinopathy; and finally central retinal vein occlusion (CRVO) or hemorrhagic retinopathy.18 Retinal hemorrhage following filtration surgery could also be associated with CRVO or Valsalva retinopathy. Wu et al reported a case of retinal hemorrhage due to CRVO after trabeculectomy with mitomycin C. They explained the anterior shift of the lamina cribrosa after a sudden decrease in IOP, especially in the advanced cupping of the optic disc, as the cause of the hemorrhage.27 Mandal et al reported another case of retinal hemorrhage after trabeculectomy in a patient with developmental glaucoma where extreme physical exertion and concomitant valsalva maneuvers occurring during general anesthesia were thought to have played a role.28 However, our patient did not show any vascular obstruction in the fluorescein angiography performed after the onset of retinal hemorrhage, and the entire surgical procedure was uneventful with no hypertensive episode or wide fluctuations of blood pressure during operation. Therefore, we do not think these hemorrhages were caused by CRVO or Valsalva's retinopathy.
Ocular decompression retinopathy has been reported in patients with POAG15,18 or after trauma,15 uveitic glaucoma,17 juvenile glaucoma,16,19 neovascular glaucoma20 or ACG.29 Our patient had steroid-induced glaucoma. The glaucoma surgeries have varied, including trabeculecomy,17,18,20 nonperforating trabecular surgery,16 Molteno valve implantation,15 and laser iridotomy.29 Both local17,18,20 and general15,17,28 anesthesia have been used. Therefore, we think that ocular decompression retinopathy may occur regardless of the type of glaucoma, glaucoma surgery or anesthesia. In addition, this suggests that the common pathogenic link is the sudden lowering of IOP that may rupture the multiple retinal capillaries. The visual prognosis after retinal hemorrhage varies according to the cases reported, and ranges from a favorable prognosis with return to the preoperative visual acuity as the hemorrhage resolves,17,20,28 to a poor prognosis with deterioration of vision accompanying the development of preretinal membrane.15
Our patient showed complete resolution of the retinal hemorrhages and restoration of preoperative visual acuity within two months. To our knowledge, this is the first reported case of unilateral, diffuse, retinal hemorrhage following bilateral trabeculectomy in a patient with steroidinduced glaucoma. In our patient, retinal hemorrhages occurred only in one eye despite both eyes undergoing the same surgery under the same conditions. We couldn't lower preoperative IOP, despite maximally tolerated medical therapy, and the difference in the eyes was due to the duration and severity of the IOP elevation before surgery and the consequent severity of the lowered IOP after the surgery. Therefore, to prevent ocular decompression hemorrhage, the following careful measures are essential: sufficient control of IOP before the glaucoma surgery, slow drainage of aqueous humor through the paracentesis and its immediate replacement with viscoelastic material in the anterior chamber to allow gradual lowering of IOP, and tight closure of the flap with releasable sutures to prevent marked and prolonged hypotony.
Figures and Tables
Fig. 1
Bleb photograph of the right eye on the first postoperative day. Note the diffuse and well-elevated bleb (black arrow). A white steroid crystal is observed in the sub-tenon capsule (white arrow).
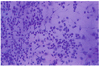
Fig. 2
(A) Fundus photograph of the right eye on the first postoperative day. Diffuse retinal hemorrhages with a white center are observed in the posterior pole and peripheral fundus. (B) Fluorescein angiogram also shows multiple, blocked fluorescence due to the retinal hemorrhages, but the vascular filling appears normal. (C) Hemorrhages are almost completely resolved two months later.

References
1. Givens K, Shields MB. Suprachoroidal hemorrhages after glaucoma filtering surgery. Am J Ophthalmol. 1987. 103:689–694.
2. Cantor LB, Katz LJ, Spaeth GL. Complications of surgery in glaucoma. Suprachoroidal expulsive hemorrhage in glaucoma patients undergoing intraocular surgery. Ophthalmology. 1985. 92:1266–1270.
3. Tuli SS, WuDunn D, Ciulla TA, et al. Delayed suprachoroidal hemorrhage after glaucoma filtration procedures. Ophthalmology. 2001. 108:1808–1811.
4. Howe LJ, Bloom P. Delayed suprachoroidal haemorrhage following trabeculectomy bleb needling. Br J Ophthalmol. 1999. 83:757.
5. The Fluorouracil Filtering Surgery Study Group. Risk factors for suprachoroidal hemorrhage after filtering surgery. Am J Ophthalmol. 1992. 113:501–507.
6. Canning CR, Lavin M, McCartney AC, et al. Delayed suprachoroidal haemorrhage after glaucoma operations. Eye. 1989. 3:327–331.
7. Ariano ML, Ball SF. Delayed nonexpulsive suprachoroidal hemorrhage after trabeculectomy. Ophthalmic Surg. 1987. 18:661–666.
8. Duane TD, Osher RH, Green WR. White centered hemorrhage: their significance. Ophthalmology. 1980. 87:66–69.
9. Kapoor S, Schiffman J, Tang R, et al. The significance of white-centered retinal hemorrhages in the shaken baby syndrome. Pediatr Emerg Care. 1997. 13:183–185.
10. Capoor S, Goble RR, Wheatley T, et al. White-centered retinal hemorrhages as an early sign of preeclampsia. Am J Ophthalmol. 1995. 119:804–806.
11. Von Barsewisch B. Perinatal Retinal Hemorrhages. 1979. New York: Springer-Verlag;48–52.
12. Neitzke R, Spraul CW, Lang GE. Bilateral retinal hemorrhages with a white leukemia. Ophthalmologe. 2001. 98:1198–1199.
13. Ling R, James B. White-centered retinal haemorrhages (Roth spots). Postgrad Med J. 1998. 74:581–582.
14. Sagaties MJ, Raviola G, Schaeffer S, et al. The structural basis of the inner blood-retina barrier in the eye of Macaca mulatta. Invest Ophthalmol Vis Sci. 1987. 28:2000–2014.
15. Dudley DF, Leen MM, Kinyoun JL, et al. Retinal hemorrhages associated with ocular decompression after glaucoma surgery. Ophthalmic Surg Lasers. 1996. 27:147–150.
16. Oh CH, Kim YY, Jung HR. A Case of Decompression Retinopathy after Glaucoma Surgery. J Korean Ophthalmol Soc. 2002. 43:2059–2063.
17. Fechtner RD, Minckler D, Weinreb RN, et al. Complications of glaucoma surgery. Ocular decompression retinopathy. Arch Ophthalmol. 1992. 110:965–968.
18. Suzuki R, Nakayama M, Satoh N. Three types of retinal bleeding as a complication of hypotony after trabeculectomy. Ophthalmologica. 1999. 213:135–138.
19. Karadimas P, Papastathopoulos KI, Bouzas EA. Decompression retinopathy following filtration surgery. Ophthalmic Surg Lasers. 2002. 33:175–176.
20. Danias J, Rosenbaum J, Podos SM. Diffuse retinal hemorrhages (ocular decompression syndrome) after trabeculectomy with mitomycin C for neovascular glaucoma. Acta Ophthalmol Scand. 2000. 78:468–469.
21. Riva CE, Grunwald JE, Petring BL. Autoregulation of Human Retinal Blood Flow. Invest Ophthalmol Vis Sci. 1986. 27:1706–1712.
22. Geijer C, Bill A. Effects of raised intraocular pressure on retinal, prelaminar, laminar, and retrolaminar optic nerve blood flow in monkeys. Invest Ophthalmol Vis Sci. 1979. 18:1030–1042.
23. Sossi N, Anderson DR. Effect of elevated intraocular pressure on blood flow. Occurrence in cat optic nerve head studied with iodoantipyrine I 125. Arch Ophthalmol. 1983. 101:98–101.
24. Findl O, Strenn K, Wolzt M, et al. Effects of changes in intraocular pressure on human ocular haemodynamics. Curr Eye Res. 1997. 16:1024–1029.
25. Grunwald JE, Riva CE, Stone RA, et al. Retinal autoregulation in open-angle glaucoma. Ophthalmology. 1984. 91:1690–1694.
26. Anderson DR. Glaucoma, capillaries and pericytes. 1. Blood flow regulation. Ophthalmologica. 1996. 210:257–262.
27. Wu SC. Central retinal vein occlusion after trabeculectomy with mitomycin C. Can J Ophthalmol. 2001. 36:37–39.
28. Mandal AK, Jalali S, Rao VS, et al. Valsalva retinopathy-like hemorrhage associated with combined trabeculotomy-trabeculectomy in a patient with developmental glaucoma. Ophthalmic Surg Lasers. 2001. 32:330–332.
29. Nah G, Aung T, Yip CC. Ocular decompression retinopathy after resolution of acute primary angle closure glaucoma. Clin Experiment Ophthalmol. 2000. 28:319–320.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download