Abstract
Purpose
To evaluate the change of axial length (AL), intraocular pressure (IOP), and corneal astigmatism after scleral shortening with scleral invagination in the rabbit eye.
Methods
The authors performed scleral shortening (3 mm) with scleral invagination in two groups of 6 eyes each: 180 degrees (group 1) and 360 degrees (group 2).
Results
Average AL shortening was more prominent in group 2 (0.5±0.17 mm) than in group 1 (0.37±0.29 mm), but the difference was not statistically significant. IOP increased immediately after the procedure and was maintained at a high level through 2 months postoperatively. Induced corneal astigmatism was more prominent in group 1 than in group 2. The difference was statistically significant in group 1 (p<0.05) but not in group 2.
Conclusions
In the scleral shortening with scleral invagination procedure, a large amount of scleral invagination resulted in more shortening of axial length, but there was more corneal astigmatism in 180-degree invagination of the sclera than in 360-degree. Further research is required to determine the effect of the extent of scleral invagination on the change of these values.
The scleral shortening technique was introduced in 1893 by Alaimo and 1903 by Muller1 as a surgical treatment technique for patients with retinal detachment. At that time, full thickness scleral resection was performed, so, it was not widely used because of choroidal injury and severe complications such as vitreous hemorrhage, retinal hemorrhage, and vitreous prolapse. Subsequently, Blaskowics2 developed safer lamellar scleral resection to reduce the complication during full thickness scleral resection. Lamellar scleral resection was applied to cases of macular hole with central retinal detachment in high myopia with posterior staphyloma, and good surgical results were reported.3-7 Recently, lamellar scleral resection has been performed as part of macular translocation surgery in age-related macular degeneration patients.8-12 In these cases, lamellar scleral resection is substituted by scleral invagination to minimize the complication accompanying scleral resection as a sclera shortening technique.10-13 However, in scleral invagination, problems of corneal astigmatism and elevated intraocular pressure (IOP) have been reported, and the amount of the macular translocation is diverse. Hence, it is difficult to predict the change of axial length after surgery as well as the development of corneal astigmatism, and in comparison with the degree of scleral invagination, the width of macular translocation is narrow.11,14,15 Recently, Deramo et al16 introduced a macular translocation technique with temporary scleral invagination using 6-0 polyglactin absorbable suture, which maintains a stable position of the translocated macula and reduces corneal astigmatism after surgery. In our study, we performed 180-degree and 360-degree scleral shortening by scleral invagination method on 12 rabbit eyes to examine the change of axial length, IOP and corneal astigmatism according to the amount of scleral invagination.
To evaluate the change of axial length, corneal astigmatism, and IOP caused by scleral shortening, 360-degree scleral shortening with a width of 3 mm, 4 mm, and 5 mm was performed. The results showed that in the cases with scleral shortening over 4 mm, the increase of IOP was so severe as to induce corneal edema during surgery and that such experiments were not feasible. Hence, scleral invagination with a width of 3mm was performed. Our experiments were performed on 12 right eyes of pigmented rabbits.
The axial length of the rabbit eyes was measured with A-scan (A/B-Scan system 835, Humphrey Instruments). And automated keratomerty (KR-8100, Topcon), corneal topography with Orbscan (Orbtek, Bausch & Lomb), IOP measurement with Tonopen (Mentor Co., USA), and fundus examination were performed before scleral shortening procedure. After that, 0.3 cc sulfur hexafluoride (SF6) gas was injected into the vitreous cavity using a 26-gauge needle through a point 3 mm posterior from the limbus and artificial vitreous liquefaction was induced. Two weeks after the injection of SF6 gas, and after confirming that the artificial vitreous liquefaction was sufficient, scleral shortening procedure was performed. Among the rabbits, 6 were classified as group 1, and the other 6 as group 2. Inferior 180-degree scleral shortening was performed by scleral invagination method in group 1, and 360-degree in group 2. For scleral invagination, rabbits were anesthetized with xylazine hydrochloride (2 mg/kg) and ketamine hydrochloride (5 mg/kg) intramuscularly, and 360-degree limbal peritomy was performed. The bridle suture was performed below the 4 rectus muscles, and the point 7 mm posterior from the limbus was marked with a marker, and an anterior and a posterior point, each at 1.5 mm, were also marked. The scleral shortening procedure with an antero-posterior width of 3 mm was performed. Scleral shortening was performed with 3 mattress sutures per quadrant by using non-absorbable 6 - 0 prolene suture. If IOP was high during or immediately after surgery, aspiration of the aqueous humor or vitreous was performed. After conjunctival suture with 8 - 0 vicryl, fundus examination was performed.
The change of axial length using A-scan ultrasonography, keratometry, and corneal topography were examined at 2, 4, 6, and 8 weeks after surgery and IOP was measured 1 hour, 1 day, and 1, 2, 4, 6, and 8 weeks after surgery. Statistical analysis methods included Mann-Whitney Rank Sum test, Wilcoxon Signed-Rank test and repeated measures ANOVA.
Almost all rabbit eyes showed mild posterior subcapsular opacity at 2 weeks after the injection of SF6 gas. However, there was no abnormality in fundus examination and inflammation was not detected in the anterior chamber.
In pre-operative examination, the average axial length of the rabbits in group 1 was 14.92±0.33 mm (14.5-15.4 mm), compared to 14.83±0.25 mm (14.5-15.2 mm) in group 2. There was no significant difference between the two groups (p=0.699). IOP was 7.67±2.80 mmHg (5-12 mmHg) in group 1 and 8.50±1.87 mmHg (6-11 mmHg) in group 2.
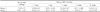
In group 1, which underwent 180-degree scleral shortening surgery, the change of axial length was 14.67±0.29 mm, 14.60±0.30 mm, 14.62±0.25 mm, and 14.60±0.25 mm at 2, 4, 6 and 8 weeks after surgery, respectively. In group 2, which underwent 360-degree scleral shortening surgery, the change of axial length was 14.43±0.15 mm, 14.45±0.14 mm, 14.42±0.13 mm, and 14.33±0.08 mm, respectively. Comparing the axial length 2 months after surgery with the preoperative value, it was shortened by an average of 0.37±0.29 mm in group 1 and 0.50±0.17 mm in group 2, and although it was smaller than the axial length calculated geometrically, this difference in shortening of axial length was statistically significant (p<0.05). In the comparison of the two groups, the degree of axial length shortening was larger in group 2 at all time points; however, a significant difference between the two groups was not detected (p>0.05) (Table 1).
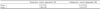
In group 1, the average IOP after surgery was 14.50±3.67 mmHg at 1 hour, 14.17±2.86 mmHg at 4 weeks, and 13.33±3.72 mmHg at 8 weeks after surgery, and it was increased almost 2-fold compared with pre-operative IOP. In group 2, IOP was 14.83±3.37 mmHg at 1 hour, 15.83±1.17 mmHg at 4 weeks, and 14.33±1.86 mmHg at 8 weeks after surgery, and the increase was equivalent to that of group 1 (Table 2).
Corneal topography, measured with Orbscan, varied widely and it was difficult to obtain reliable data before surgery, and also up to 8 weeks after surgery. In automated refraction and keratometry before surgery, various patterns of corneal astigmatism were detected in rabbit eyes. After surgery, the exacerbation of the degree of astigmatism was detected, with a diverse pattern. Corneal astigmatism was significantly increased from 4.38±1.81 D before surgery to 6.14±1.35 D at 8 weeks after surgery in group 1 (p=0.028) and it was increased primarily along the meridian where scleral invagination surgery was performed. In group 2, it was increased from 3.9±4.09 D to 4.83±2.05 D at 8 weeks after surgery, but the increase was not statistically significant (p=0.6) (Table 3).
In the past, scleral shortening procedure was performed to facilitate the reattachment of the retina in patients with macular hole and retinal detachment due to posterior staphyloma in high myopia.5-7 Recently, scleral shortening procedure has been performed in age-related macular degeneration patients as part of macular translocation surgery. Macular translocation surgery was first introduced by Machemer and Steinhorst,8,9 and they performed 360-degree retinotomy and total retinal detachment. The complications of 360-degree retinotomy and macular translocation surgery, such as retinal detachment, severe proliferative vitreoretinopathy, intraocular hemorrhage, diplopia and recurrence of choroidal neovascularization, have been reported.17,18 To reduce such complications, de Juan18 developed macular translocation technique with partial scleral resection. Nevertheless, even in macular translocation surgery with scleral shortening technique, complications such as corneal astigmatism and refractive error have been reported.15
The methods of scleral shortening are full thickness scleral resection, lamellar scleral resection that removes approximately 2/3 of the scleral thickness, and scleral invagination which had fewer complications and was relatively safer. Recently, scleral outfolding using titanium clips has been proposed.19 In the cases of scleral invagination used in limited macular translocation, corneal astigmatism and the excessive elevation of IOP have been reported. Another problem is that the degree of macular translocation by scleral invagination is not constant and a small range of macular translocation, approximately 1mm, can be induced by 5 mm scleral invagination.12-15,20 If the subfoveal neovascular membrane is too large, a large amount of macular translocation is required. Consequently, a large amount of scleral shortening may be required, and in such cases it is essential to have a good understanding of the change of the eyeballs such as axial length, IOP, and corneal astigmatism.
In previous reports on the change of axial length after scleral shortening, Matsumura and Ogino7 have reported that there was no statistically significant correlation between the amount of sclera resected and the shortening of axial length in patients with retinal detachment accompanying posterior staphyloma. However, this result was considered to be due to all subjects having high myopia with posterior staphyloma with caused difficulty in the accurate measurement of axial length. Nakagawa21 performed 4 different methods of sclera shortening procedure using human eyes stored in an eye bank: three groups of 10 eyes each underwent lamellar scleral resection with dissection of 6, 8, and 10 mm in height, and the other group of 10 eyes underwent a 10-mm invagination. They reported that average axial length shortening following lamellar resections for 6, 8, and 10 mm groups were 1.50±0.24 mm, 2.10±0.13 mm, and 2.65±0.24 mm, respectively, and 2.50±0.23 mm for the 10 mm invagination group. In their report, axial length was shortened by 25% of the width of scleral shortening and the amount of scleral shortening significantly correlated to the shortening of axial length. There was no significant difference of the effect of axial length shortening between lamellar scleral resection and scleral invagination.
In our study, a statistically significant shortening of axial length was noted at 2, 4, 6 and 8 weeks after surgery in both groups of rabbit eyes, compared with the axial length before scleral shortening (Table 1). In group 1, which underwent 180-degree scleral shortening with a width of 3 mm, the shortening of axial length averaged 0.37 mm, which showed a shortening of axial length by 12.33% of the 3 mm scleral shortening. In group 2, which underwent 360-degree scleral shortening with a width of 3 mm, axial length was shortened by an average of 0.50 mm, which was approximately 8.33% of the total scleral shortening of 6 mm. In the result of Nakagawa, axial length was shortened by approximately 25% of the amount of scleral shortening, compared to 12.33% in group 1 and 8.33% in group 2 in our study. In our study, scleral invagination procedure was performed on live rabbits, which is different from Nakagawa's experiment that was performed under the condition of normal IOP maintained through infusion cannula. In vivo, the effect of scleral shortening on axial length may be reduced more than the experimental value of Nakagawa, due to the continuous effect of IOP after surgery. In addition to the relaxation effect on the scleral shortening suture by the increased IOP after surgery, errors from the measurement of actual axial length may also have occurred in our experiment, and the morphological differences between rabbit and human eyes may be an additional cause of the different shortening effects.
In our study, the shortening of axial length in group 2 was larger than that in group 1, although the difference was not statistically significant. However, a smaller range of the reduction of axial length was detected in group 2. This result may have been due to the fact that the effect of lengthening of axial length was accompanied by the contraction of the sclera, similarly to scleral encircling buckle, in the cases of 360-degree scleral shortening, and that the reduction range was therefore smaller in group 2.22
IOP immediately after operation was increased substantially but decreased slightly at 2 months after operation in our study. The cause of the increased IOP was considered to be due to the structural characteristic of the rabbit eyes. In rabbits, the lens volume is relatively large in comparison to vitreous volume, and hence, even if the same amount of scleral shortening is performed, the degree of the reduction of vitreous volume is larger. In addition, it was considered that the microscopic change of the anterior segment of the eyes by scleral shortening may affect aqueous outflow. In clinical cases of scleral invagination, scleral shortening was performed under the condition with low IOP through an infusion cannula. Kim15 and de Juan18 reported performing cases of scleral shortening only in a small area of the superotemporal quadrant, which may have eliminated the problem of the increased IOP during or immediately after operation. However, in a study of patients who underwent 180-degree scleral invagination and macular translocation for 2 years, high IOP lasted for approximately one month after the operation was reported,20 and thus additional studies on the change of IOP after scleral invagination operation may be required.
Scleral shortening has been reported to change the shape of the cornea and induce substantial corneal astigmatism. Kim15 has reported that in a retrospective study on 8 cases, after the scleral invagination operation on the superotemporal quadrant using non-absorbable suture, a large amount of corneal astigmatism was developed and approximately 80% of astigmatism was eliminated in 2 cases by suture removal. In other studies, scleral shortening was performed using absorbable sutures to reduce corneal astigmatism after surgery and the corneal astigmatism disappeared gradually with time.16 In our study, corneal astigmatism of rabbits prior to surgery was so irregular that it was difficult to obtain accurate values. Nevertheless, similarly to the report by Kim,15 a statistically significant increase of corneal astigmatism at the vertical meridian was detected in automated refraction and corneal topography in group 1, which underwent 180-degree scleral invagination surgery. This is in agreement with the results showing increased corneal astigmatism in the meridian of partial scleral resection reported by Lee.23
The shortening of axial length by scleral invagination surgery may affect the refractive power in macular translocation surgery. The length of the shortened sclera and the reduction of axial length correlated somewhat, but their clear relationship cannot be explained by our experimental results alone. The corneal astigmatism showed a pattern of increase toward the meridian of partial scleral invagination; however, it was difficult to predict precisely. Nonetheless, it is believed that a certain degree of nomogram may be obtained by additional experiments, which may provide basic information for future scleral invagination operation in macular translocation surgery.
Figures and Tables
References
1. Muller L. Eine neue operative Behandlung der Netzhautabhebung. Klin Monatsbl Augenheikd. 1903. 41:459–462.
2. Schepens CL. Retinal Detachment and Allied Diseases. 1983. Vol.1. Philadelphia: WB Saunders Co;8–9.
3. Everett WG. An experimental evaluation of scleral shortening operations. Arch Ophthalmol. 1956. 56:34–47.
4. Chamlin M, Rubner K. Lamellar undermining; a preliminary report on a technique of scleral buckling for retinal detachment. Am J Ophthalmol. 1956. 41:633–638.
5. Kuriyama S, Matsumura M, Harada T, et al. Surgical techniques and reattachment rates in retinal detachment due to macular hole. Arch Ophthalmol. 1990. 108:1559–1561.
6. Siam AL. Macular hole with central retinal detachment in high myopia with posterior staphyloma. Br J Ophthalmol. 1969. 53:62–63.
7. Matsumura M, Ogino N. A Surgical approach for macular hole retinal detachment associated with high myopia. Jpn J Ophthalmic Surg. 1996. 9:425–428.
8. Machemer R, Steinhorst UH. Retinal separation, retinotomy, and macular relocation: I. Experimental studies in the rabbit eye. Graefes Arch Clin Exp Ophthalmol. 1993. 231:629–634.
9. Machemer R, Steinhorst UH. Retinal separation, retinotomy, and macular relocation: II. A surgical approach for age-related macular degeneration? Graefes Arch Clin Exp Ophthalmol. 1993. 231:635–641.
10. Akduman L, Karavellas MP, MacDonald JC, et al. Macular translocation with retinotomy and retinal rotation for exudative age-related macular degeneration. Retina. 1999. 19:418–423.
11. Fujikado T, Ohji M, Hayashi A, Yano Y. Visual function after foveal translocation with scleral shortening in patients with myopic neovascular maculopathy. Am J Ophthalmol. 1998. 125:647–656.
12. Lewis H, Kaiser PK, Lewis S, Estafanous M. Macular translocation for subfoveal choroidal neovascularization in age-related macular degeneration: a prospective study. Am J Ophthalmol. 1999. 128:135–146.
13. Lin SB, Glaser BM, Gould D, et al. Scleral outfolding for macular translocation. Am J Ophthalmol. 2000. 130:76–81.
14. Weinberger D, Lichter H, Loya N, et al. Corneal topographic changes after retinal and vitreous surgery. Ophthalmology. 1999. 106:1521–1524.
15. Kim T, Krishnasamy S, Meyer CH, Toth CA. Induced corneal astigmatism after macular translocation surgery with scleral infolding. Ophthalmology. 2001. 108:1203–1208.
16. Deramo VA, Meyer CH, Toch CA. Successful macular translocation with temporary scleral infolding using absorbable suture. Retina. 2001. 21:304–311.
17. Eckardt C, Eckardt U, Conrad HG. Macular rotation with and without counter-rotation of the globe in patients with age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 1999. 237:313–325.
18. de Juan E Jr, Loewenstein A, Bressler NM, Alexander J. Translocation of the retina for management of subfoveal choroidal neovascularization II. A preliminary report in humans. Am J Ophthalmol. 1998. 125:635–646.
19. Kamei M, Roth DB, Lewis H. Macular translocation with chorioscleral outfolding: an experimental study. Am J Ophthalmol. 2001. 132:149–155.
20. Mateo C, Moreno J, Rosales G, et al. Two-year results of macular translocation with scleral infolding in myopic choroidal neovascularization. Semin Ophthalmol. 2004. 19:29–42.
21. Nakagawa N, Parel JM, Murray TG, Oshima K. Effect of scleral shortening on axial length. Arch Ophthalmol. 2000. 118:965–968.
22. Seo JM, Park KS, Yu HG, Chung H. Geometric changes of the eye with an encircling scleral buckle. J Korean Ophthalmol Soc. 2002. 43:1072–1080.
23. Lee JH, Oh SO, Hwang JM. The changes of corneal curvature after scleral resection. J Korean Ophthalmol Soc. 1988. 29:53–55.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download