Abstract
A 45-year-old man with retinitis pigmentosa (RP), who had undergone uneventful extracapsular cataract extraction (ECCE) in his right eye eight years previously, and phacoemulsification in his left eye six years previously, had spontaneously dislocated intraocular lenses (IOL) within the capsular bag in both eyes one month apart. We removed the dislocated IOLs, and performed anterior vitrectomy and scleral fixation of the new IOLs. Mild contraction of the capsular bags and uneven distribution of the zonular remnants' clumps along the equator of the capsules were found by scanning electron microscopic (SEM) examination. In this study, we propose the correlation between RP and zonular weakness. To our knowledge, this is the first case report of bilateral spontaneous dislocation of IOLs within the capsular bag of an RP patient.
A typical form of retinitis pigmentosa (RP) is frequently associated with posterior cortical and posterior subcapsular cataracts, which may cause significant visual disturbance when combined with restricted central visual field. RP patients with cataracts tend to undergo early cataract surgery, and postoperative results are known to be successful.1-3
The post-operative complications of cataract surgery in RP patients are cystoid macular edema, high incidence of posterior capsular opacification, capsulorhexis phimosis, and intraocular lens (IOL) decentration.1,4-6 We experienced a case of an RP patient who had bilateral spontaneous dislocation of IOLs within the bag 6 and 8 years after successful cataract surgery in the left and right eyes, respectively. We describe the mechanism of the zonular weakness of dislocated IOL and capsule by scanning electron microscopy (SEM).
A 37-year-old man was diagnosed at our clinic with RP and posterior subcapsular and mild nucleosclerosis cataract in his right eye, and anterior capsular cataract in his left eye in September, 1994. The fundus examination showed bone-spicule pigmentation sparing macula and pale optic disc in both eyes (Fig. 1). The visual field was restricted to central 10° and electroretinogram finding showed reduced amplitude. The best corrected visual acuity (BCVA) was 20/20 in both eyes, and other ocular findings were unremarkable. The patient had no family history of RP.
He underwent uneventful, planned, extracapsular cataract extraction (ECCE) after can-opener capsulotomy and continuous curvilinear capsulorhexis (CCC) capsulotomy, and followed by one-piece polymethyl methacrylate (PMMA) posterior chamber IOL (Rayner, 272U, England) implantation in his left eye in February, 1995. In addition, he underwent uneventful phacoemulsification following CCC and one-piece PMMA posterior chamber IOL (Rayner, 272U, England) implantation in his right eye in July, 1997. Zonular weakness was not found during cataract surgery in either eye. The post-operative BCVA was 20/20, and other findings were unremarkable in both eyes. The patient had Nd:YAG laser posterior capsulotomy because of posterior capsular opacity in his right eye in 1998.
In April, 2003, the patient revisited our clinic due to fluctuation of visual acuity in his right eye. His general health status was good, and no episode of ocular disease or trauma was found. On pupil dilation examination of his right eye, slight inferior deviation of IOL within the capsular bag was found, and capsulorhexis phimosis was not prominent. Two months later, the patient returned with further visual disturbance in his right eye. A significant downward progression of IOL was noted, and a superior zonulysis between the positions of 8 to 4 o'clock and partially prolapsed vitreous into the anterior chamber at 12 o'clock were also observed (Fig. 2). IOL removal, anterior vitrectomy and secondary IOL (Alcon, CZ70BD, USA) scleral fixation were performed in the right eye. Immediate post-operative BCVA was 20/20, and no other complication was found.
The removed IOL was fixed in 2% glutaraldehyde, postfixed in 1% osmium tetroxide for 1 hour, and subjected to dehydration in ethanol. It was critical-point dried, sputter coated with gold palladium and examined by SEM (Philips 515 SEM). IOL was encapsulated within the bag with marked contracture of the capsular bag, and the haptics were deformed inward due to capsular contracture. The anterior and posterior capsule were adherent firmly due to fibrosis in the space between the optic and haptic. The capsulorhexis phimosis was not severe, and the CCC margin was sharply maintained. Uneven distribution of the zonular remnants' clumps along the equator of the capsular bag was found (Fig. 3).
One month later, the patient returned to the clinic because of sudden loss of visual acuity in his left eye. On slit lamp examination of his left eye, a haptic was prolapsed into the anterior chamber, and the optic was captured by the temporal iris (Fig. 4). Zonular dehiscence was seen between the positions of 1 to 6 o'clock, while IOL was in the capsular bag by pupil dilation examination. IOL removal, anterior vitrectomy and IOL scleral fixation (Alcon, Z70BD, USA) were performed. On SEM examination of the extracted IOL within the bag, zonular remnants were found evenly distributed on most of the equator (Fig. 5), and other findings were identical with those of the right eye.
Three months after surgery, the IOLs were well positioned, and BCVA of both eyes were 20/20. Other ocular examinations were within normal limits.
The complications in cataract surgery in RP patients have been known as IOL decentration, tilting, posterior capsular opacity, and in several reports, zonular weakness during surgery.1-6,8
Rachipalli et al.5 reported a case of an RP patient who presented with a dense nucleosclerosis, iridodonesis and phacodonesis. They observed scattered zonular loss and laxity on ultrasound biomicroscopic examination preoperatively, performed ECCE and IOL implantation without intraoperative complications and found decentered IOL four months later. Hayashi et al.6 suggested the possible existence of zonular weakness in RP patients with severe anterior capsule contraction and IOL dislocation after cataract surgery.
In this study, we report the first case of bilateral spontaneous IOL dislocation within the capsular bag with minimal capsulorhexis phimosis in an RP patient a few years following successful cataract surgery. The normal structure had been maintained immediately after surgery, but accumulation of damage to the zonules from degenerative aging process and minor trauma may cause gradual progression of zonular weakness.
Firstly, one of the possible multifactorial processes of IOL dislocation is that the RP patients might experience zonular weakness.5-8 Namiki et al.7 showed unilateral dehiscence of the zonules in an RP patient, but they were not able to provide a satisfactory explanation. In our case, bilateral zonular weakness was found by SEM. We can infer the original status of the zonular insertion from the zonular remnants' clumps along the equator. Uneven distribution is composed of a preexisting, degenerative bare region and a newly developed, weak remnant region upon IOL removal. We found that zonules were distributed unevenly, capsulorhexis phimosis was not severe, and the CCC margin was sharply maintained in his right eye. On the contrary, zonular remnants were seen evenly distributed on most of the equator in his left eye. Weak zonules may allow progression of the anterior capsular contracture easily, which may introduced further zonular weakenss.9 In the right eye, marked capsular contracture, which leads to deformation of the haptic, may have been induced by preexisting zonular weakness. Therefore IOL dislocation may occur mainly due to degenerative zonular weakness rather than capsular contracture.
Secondly, intraoperative stress might damage the zonules. Modern cataract surgery often uses high vacuum, irrigation, and aspiration pressure. Such manipulations may harm the zonules.9,10 In this case, the IOL dislocation occurred 8 years later in the eye with ECCE, but 6 years later in the eye with phacoemulsification, and the dislocated was most severe in the upper part of the zonules around 12 o'clock. This suggests that phacoemulsification may have put more stress on the zonules than planned ECCE.
Thirdly, zonular weakness was more severe in the right eye which underwent Nd:YAG laser posterior capsulotomy. We postulate that YAG capsulotomy may contribute to zonular weakness. Framme et al.11 reported a case of zonulysis and PMMA IOL dislocation within the intact capsular bag six months after Nd:YAG laser capsulotomy. They explained that zonulysis was triggered by contraction of the capsular bag after the YAG capsulotomy. The possible factors are anterior capsular contraction and shrinkage.5,6,11
Further studies are needed to prove the validity of these possibilities, and to examine the mechanism.
In conclusion, RP patients may have a preexisting zonular weakness which can be aggravated by cataract surgery. Therefore, a careful preoperative evaluation of the zonules is needed, and intraoperative stress on the zonules should be minimized. In addition, the surgeon should be aware of the possibility of delayed IOL dislocation which may occur several years after the operation. RP patients should be informed about the possibility of delayed postoperative complications before cataract surgery.
Figures and Tables
Fig. 1
Fundus photograph of the right(A) and left(B) eyes. Bone-spicule pigmentation just anterior to the posterior pole with normal-appearing macula and slightly pale optic disc are evident.

Fig. 2
Slit lamp photograph. IOL dislocation in the right eye after pupil dilation six years after phacoemulsification can be seen.

Fig. 3
Scanning electron microscopy. A: The removed intraocular lens within the capsular bag in the right eye with phacoemulsification. B, C: The zonular remnants' clumps are unevenly distributed on the equator. D: There are some parts with no zonules. Equator and haptic, white arrows; continuous curvilinear capsulorhexis margin, asterisks; optic, black arrows; zonular remnants' clumps, arrowheads (A: original magnification ×22. B: original magnification ×44. C: original magnification ×178. D: original magnification ×356).

Fig. 4
Slit lamp photograph. A: A haptic has been prolapsed into the anterior chamber and the optic has been captured by the temporal iris in the left eye, but they are still in the bag. B: After pupil dilation, zonular dehiscence can be seen between the positions of 1 to 6 o'clock (white arrows).
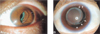
Fig. 5
Scanning electron microscopy. The zonular remnants (arrowheads) are found more evenly distributed and densely on most of the equator (white arrows) of the capsular bag in the left eye which underwent ECCE than the right eye. (A: original magnification ×44. B: original magnification ×178. C: original magnification ×356).

References
1. Jackson H, Garway-Heath D, Rosen P, Bird AC, Tuft SJ. Outcome of cataract surgery in patients with retinitis pigmentosa. Br J Ophthalmol. 2001. 85:936–938.
2. Reccia R, Scala A, Bosone G. Posterior chamber intraocular lens implantation in patients with retinitis pigmentosa. Doc Ophthalmol. 1989. 72:115–118.
3. Newsome DA, Stark WJ Jr, Maumenee IH. Cataract extraction and intraocular lens implantation in patient with retinitis pigmentosa or Usher's syndrome. Arch Ophthalmol. 1986. 104:852–854.
4. Nishi O, Nishi K, Fusisawa T. Effects of cytokines on the proliferation of and collagen synthesis by human cataract lens epithelial cells. Br J Ophthalmol. 1996. 80:63–68.
5. Rachipalli R, Srinivas K. Capsulorhexis phimosis in retinitis pigmentosa despite capsular tension ring implantation. J Cataract Refract Surg. 2001. 27:1691–1964.
6. Hayashi K, Hayashi H, Matsuo K, Nakao F, Hayashi F. Anterior capsule contraction and intraocular lens dislocation after implant surgery in eyes with retinitis pigmentosa. Ophthalmology. 1998. 105:1239–1243.
7. Namiki M, Tagami Y, Morino I. Findings from slit lamp and histological examination of the anterior capsule in patients with severe anterior capsule shrinkage and opacities after implantation of intraocular lens. J Jpn Ophthalmol Soc. 1993. 97:716–720.
8. Lee DH, Yoon BJ, Kim HJ. Intraocular lens implantation in retinitis pigmentosa patients. J Korean Ophthalmol Soc. 1990. 31:1520–1522.
9. Nishi O, Nishi K. Intraocular lens encapsulation by shrinkage of the capsulorhexis opening. J Cataract Refract Surg. 1993. 19:544–545.
10. Shigeeda T, Nagahara M, Kato S, Kunimatsu S, Kaji Y, Tanaka S, Amano S, Oshika T. Spontaneous posterior dislocation of intraocular lenses fixated in the capsular bag. J Cataract Refract Surg. 2002. 28:1689–1693.
11. Framme C, Hoerauf H, Laqua H. Delayed intraocular lens dislocation after neodymium: YAG capsulotomy. J Cataract Refract Surg. 1998. 24:1541–1543.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download