Abstract
The purpose of this study is to assess the efficacy of the multi-zone cross-cylinder method as compared with the single method for astigmatism correction using LASIK. This prospective study enrolled 40 patients (52 eyes) who underwent the cross-cylinder method using LASIK, and 52 patients (60 eyes) who underwent the single method using LASIK: all patients were given a diagnosis of complex myopic astigmatism from the department of ophthalmology of this hospital between January 2002 and July 2003. Preoperatively, the mean spherical equivalent refraction was -3.85 ± 1.13 D in the cross-cylinder group and -4.05 ± 1.20 D in the single method group (p = 0.23). The mean cylinder was -2.05 ± 1.58 D in the cross-cylinder group and -1.95 ± 1.12 D in the single method group (p = 0.31). 6 months after treatment the results were a mean spherical equivalent refraction of -0.26 ± 0.30 D in the cross-cylinder group and -0.34 ± 0.35 D in the single method group (p = 0.13). The mean cylinder was -0.38 ± 0.29 D in the cross-cylinder group and -0.45 ± 0.30 D in the single method group (p = 0.096). There were no statistically significant differences between the two groups. The mean BCVA was not different from mean preoperative BCVA in both groups (i.e., 0.98 ± 0.10, 0.96 ± 0.25, p = 0.86). Postoperatively, patient complications that included night halo, glare and corneal haze were not noted in either group. In conclusion, the results of cross-cylinder method are no different from the single method for the correction of a complex astigmatism. In the future, studies will have to be conducted to assess the efficacy of the cross-cylinder method in consideration of those factors that can affect the postoperative outcome.
LASIK has been widely used as a surgical technique for myopia correction.
LASIK has also been reported to be effective for the treatment of complex myopic astigmatism as well as for simple myopia.1-3 However, various functional disorders such as myopic regression and corneal haze may occur after the myopia was corrected with an excimer laser.4 Vinciguerra et al4 proposed this new correction method for myopia on the grounds that these functional disorders were mainly due to the presence of junctions between the operated and non-operated sites. These junctions were caused by a conventional keratomileusis that managed only the steepest meridian. Based on the above reasons, we conducted this study to evaluate the clinical efficacy of the correction method proposed by Vinciguerra et al for the management of astigmatism.
This study enrolled 92 patients (112 eyes) who underwent a LASIK treatment: the patients were given a diagnosis of complex myopic astigmatism at department of ophthalmology of this hospital between January 1, 2002 and July 31, 2003. The cross-cylinder method group enrolled 40 patients (52 eyes) and the single method group enrolled 52 patients (60 eyes). The present study included patients with a stable complex myopic astigmatism of the refractive status showing a variation of less than 0.5 D within a year; it excluded those patients with other concomitant ophthalmic diseases or those patients with a past history of ophthalmic surgery. The preoperative use of contact lens was prohibited for 10 days (soft lens) and 3 weeks (hard lens). Preoperatively, all the patients underwent the following tests for uncorrected/corrected visual acuities and subjective refraction: an anterior segment examination including IOP and slit lamp examinations, fundoscopy, the test for corneal refraction, and a corneal pachymetry. For the surgical treatment, an EC-5000 excimer laser (Nidek Co. Ltd.,Gamagori, Japan) was used. The laser had a wavelength of 193 nm, an ablation rate of 0.6 µm/scan, a laser repetition rate of 40 Hz and an energy of 108-120 mJ/mm.2 The cross-cylinder surgery was done according to the following 3 steps: The hyperopic astigmatism was first corrected along the most steep meridian (OZ:5.5mm, TZ:8.0mm) and then the myopic astigmatism was corrected along the most flat meridian (OZ:6.0mm, TZ:8.0mm). After that, a residual amount of myopia (spherical equivalent refraction) was corrected (OZ:6mm, TZ:8.0mm). The ratio of myopic to hyperopic astigmatism was set at 50% each. For anesthesia, proparacaine (Alacaine, Alcon) 0.5% was dropped on patients' eyes 5-6 times at a 5 minute interval and then the patients' peri-ophthalmic regions were disinfected. After the patients eyes were opened with a speculum, a corneal section of 130 µm in thickness was prepared with automated microkeratome (MK-2000, NIDEK). The diameter of the suction ring we used was 8.5 mm, and the corneal section was turned over using a spatula and then the excimer laser was irradiated according to the degree of refraction. We did not use a specific eyeball fixator; the patients were instructed to fix their eyeballs by viewing the target themselves. After excimer laser irradiation, the residual corneal section was determined to be at a minimum of 300 µm in thickness. The corneal section was returned to patients' eye it was then dried so as to attach itself to the corneal parenchyma. On postoperative day 1 and thereafter, Ofloxacin (Tarivid, Santen Pharmaceutical Corp.) and 0.1% of Flumetholon (Santen Pharmaceutical Corp.) were dropped on patients' eyes 4 times a day at 6-hour intervals. After 2 weeks, the frequency of eyedrop application was determined on the basis of the individual patients' profile of myopic regression.
To comparatively evaluate the preoperative and postoperative myopic profiles, this study monitored corneal haze (as well as uncorrected visual acuity), corrected visual acuity, spherical equivalent refraction and astigmatic progression on postoperative week 1, month 1, month 3 and month 6.
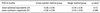
The mean age was 27.22 ± 5.85 years old in the cross-cylinder group and 29.65 ± 7.22 years old in the single method group (p = 0.65). The mean value of preoperative BCVA was 0.98 ± 0.10 in the cross-cylinder group and 0.96 ± 0.25 in the single method group (p = 0.86). In addition, as a mean refraction error, the mean spherical equivalent refraction was -3.85 ± 1.13 D in the cross-cylinder group and -4.05 ± 1.20 D in the single method group (p = 0.23). The mean cylinder was -2.05 ± 1.58 D in the cross-cylinder group and -1.95 ± 1.12 D in the single method group (p = 0.31). There were no significant differences found between the two groups (Table 1). On postoperative month 6, the mean uncorrected visual acuity was 0.89 ± 0.16 and the mean BCVA was 0.98 ± 0.10 in the cross-cylinder group, and 0.91 ± 0.35 and 0.96 ± 0.25 respectively in the single method group. The changes of postoperative spherical equivalent and the cylinderic magnitude were not significantly different between the two groups (Table 2, Fig. 1, 2). On postoperative month 6, the mean spherical equivalent refraction was -0.26 ± 0.30 D in the cross-cylinder group and -3.34 ± 0.35 D in the single method group (p = 0.13). The mean cylinder was -0.38 ± 0.29 D in the cross-cylinder group and -0.45 ± 0.30 D in the single method group (p = 0.096) (Table 3). There were no statistically significant differences found between the two groups. Postoperatively, the axis of residual myopic astigmatism was not changed, but 5 cases showed a 90° deviation because of a hypercorrection. In addition, no postoperative complications were noted, and these potential post-op complications included night halo, corneal haze and glare.
Among the various methods used in the surgical treatment of myopia, (these include clear lens extraction, PRK, LASIK and radial keratotomy), PRK has been frequently used for a moderate myopia of less than -6.0 D and LASIK has been frequently used for a higher myopia of more than -8.0 D.5,6 Although there have been only a few long term follow up studies, the previous studies suggest that LASIK is indicated in cases with a high myopia of more than -8.0 D. LASIK was formerly contraindicated for PRK due to the problems of myopic regression and corneal haze, and these cases of high myopia had shown an uncorrected visual acuity of more than 0.5 on the sixth postoperative month in 45-81% of the total patients.7,8 In addition, LASIK has been reported to show an excellent outcome in the surgical correction of complex myopic astigmatism.1-3,9
For myopia correction using LASIK, the most universal method is the single method where cornea is resected on the affected side with myopic astigmatism. However, both sides including the most steep and flat meridians are corrected in the cross-cylinder method. The purpose of this multizone cross-cylinder is to make a transitional zone with little difference in refractive power between the treated and untreated sites. Due to the discrepancy of diopter in the small optical zone, a multi-focal area was formed in the middle of a cornea; as a results, the problems of glare, night halo and decreased contrast sensitivity were noted. In areas with a great difference in refraction on the corneal surface, deranged cellular immunity and aggravated corneal haze gives rise to myopic regression and a decreased visual acuity. These problems may be solved using a corneal resection in a step-wise and sequential manner. Such corneal resection has the following advantages: (1) It is possible to prepare the physiologically prolate and symmetrical shape of cornea; (2) The rate of myopic regression is relatively low; (3) An improved visual acuity is obtained; and (4) The amount of resection is reduced through a sequential resection of the astigmatism.10
Figure 3 schematically represents the principle of multi-zone cross-cylinder excimer laser ablation.4 Fig. 3 describes a cornea in those cases with complex myopic astigmatism showing a 180° deviation. To make for than easier understanding, the order of corneal resection was described in the reverse order of surgical procedure, and the optical/transitional zones were arbitrarily set. A zone corresponded to the correction site for hyperopic astigmatism with a 90° deviation (OZ: 5.5 mm, TZ: 9.0 mm), B zone corresponded to the correction site for myopic astigmatism with a 180° deviation (OZ: 5.5 mm, TZ: 8.5 mm) and C zone corresponded to the correction site for residual astigmatism (spherical equivalent refraction) (OZ:5.5 mm). For example, -2.00 sphere -1.00 cylinder × 180° hyperopic astigmatism was first corrected to +0.5D at a 90° axis and then myopic astigmatism was corrected to -0.5D at a 180° axis. After that, the residual spherical equivalent refraction of -2.50 D was to be further corrected. The above method resected a cornea to make a steep meridian (90°) flatter and the flat meridian (180°) steeper. To summarize, a uniform corneal resection made it possible to obtain a relatively smooth corneal surface.
Salchow et al11 reported that the refractive error of -0.40 ± 0.98 D remained at month 6 after LASIK surgery for myopia of -6.78 ± 3.48 D, and Salah et al12 reported a myopic regression of -0.61 D on average between 3 weeks and 6 months after LASIK surgery. In Korea, Choi et al13 noted a myopic regression of -0.52 ± 0.88 D between postoperative week 1 and month 6 in patients with a refractive error of -8.56 ± 2.67 D. In this present study on patients with myopia of -3.85 ± 1.13 D, the mean spherical equivalent refractions were 0.35 ± 0.36 D and -0.26 ± 0.30 D on postoperative week 1 and month 6, respectively. The patients' mean myopic regression was -0.61 ± 0.353 D between postoperative week 1 and month 6. Although statistically insignificant, this study revealed a postoperative mild-to-moderate tendency of hypercorrection, and there was no difference in myopic regression as compared to the aforementioned studies. There are some other studies reported in the literature for the surgical correction of astigmatism performed by the single method. Fraenkel et al14 reported that the mean residual astigmatism of 0.74 D was noted in the surgical treatment of astigmatism of 1.99 D on postoperative month 6. Zaldivar et al15 reported that the mean residual astigmatism of 0.39 D was noted in the surgical treatment of astigmatism of 1.84 D on postoperative month 6. In Korea, Kim et al16 reported that the mean residual astigmatism of 0.58 ± 0.72 D was noted in the surgical treatment of astigmatism of 1.0 ± 1.75 D on postoperative month 1. In the present cross-cylinder method study, the mean residual astigmatism of -0.38 ± 0.29 D was noted in the surgical treatment of myopic astigmatism of -2.05 ± 1.58 D at postoperative month 6. This indicates that the cross-cylinder method is clinically effective for the correction of astigmatism, although it is difficult to directly compare this study with the aforementioned ones.
In the present study, we compared the cross-cylinder method group and single method group. There were no statistically significant differences of the mean spherical equivalents and the mean cylinderic magnitudes between the two groups. However, we founded that the cross-cylinder method was a bit better than single method, although the mathematical difference was statistically insignificant. We think that the cross-cylinder method is clinically more effective than the single method for the correction of astigmatism since the cross-cylinder method creates smooth transitional zone (with a low dioptric gradient) between the treated and untreated cornea.
We have noted that the present study has revealed some problems of cross-cylinder method. (1) There is a lot of possibility of decentration occurring due to patients' loss of attention and the long surgical time necessary for the corrections of hyperopic astigmatism, myopic astigmatism and myopia. (2) Due to indications for correction of the hyperopic astigmatism, the cross-cylinder method required a thicker central cornea because of the wider transitional zone as when compared to the single method. This can lead to some limitations in patient recruitment. (3) In spite of the unknown cause, the cross-cylinder method shows hypercorrection when compared to the single method at an early postoperative stage. In the present study, the mean spherical equivalent refraction was 0.35 ± 0.36 D on postoperative month 1, and this corresponded to hypercorrection at an early postoperative stage as compared with other studies.
There are various factors affecting the postoperative outcomes and these include the preoperative amount of astigmatism, discordance of astigmatic axis between patients and the laser, errors of axis determination, decentration and the deposition of foreign body in the transitional zone.17 The present study posed some limitations because it was conducted on a small-sized patient population and it did not consider visual quality and other factors quantitatively. In the future, Further studies will be needed to assess the efficacy of cross-cylinder method and to take into consideration such factors as postoperative myopic regression, contrast sensitivity, corneal haze, glare and night halo that can affect the postoperative outcome.
Figures and Tables
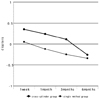 | Fig. 1The graph of postoperative mean spherical equivalent changes (D) in 6 months after cross-cylinder ablation. |
 | Fig. 2The graph of postoperative mean cylinderic changes (D) in 6 months after cross-cylinder ablation. |
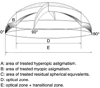 | Fig. 3Myopic with-the-rule astigmatism corrected with a cross-cylinder method. The surgical strategy involved ablating half the amount of the cylinder along steepest meridian, the other half in a subsequent step along the flattest meridian; thereafter, the spherical equivalent was corrected. |
Table 1
Preoperative characteristics of patients. There are no statistically significant differences between the two groups.

References
1. Pallikaris IG, Papatzanaki ME, Stathi EZ. Laser in situ keratomileusis. Lasers Surg Med. 1990. 10:463–468.
2. Hersh PS, Abbassi R. Summit PRK-LASIK Study Group. Surgically induced astigmatism after photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg. 1999. 25:389–398.
3. Dulaney DD, Barnet RW, Perkins SA, Kezirian GM. Laser in situ keratomileusis for myopia and astigmatism: 6 month results. J Cataract Refract Surg. 1998. 24:758–764.
4. Vinciguerra P, Sborgia M, Epstein D, Azzolini M, MacRae S. Photorefractive keratectomy to correct myopic or hyperopic astigmatism with a cross-cylinder ablation. J Refract Surg. 1999. 15:S183–S185.
5. Sohn JH, Cha HW, Kim YJ. Excimer laser photorefractive keratectomy-multicenter study. J Korean Ophthalmol Soc. 1993. 34:1208–1212.
6. Jun SG, Cha HW, Kim YJ. Excimer laser photorefractive keratectomy: two-year follow-up. J Korean Ophthalmol Soc. 1997. 38:17–26.
7. Pallikaris IG, Siganos DS. Excimer laser in situ keratomileusis and photorefractive keratectomy for correction of high myopia. J Refract Corneal Surg. 1994. 10:498–510.
8. Guell JL, Muller A. Laser in situ keratomileusis (LASIK) for myopia from -7 to -18 diopters. J Refract Surg. 1996. 12:222–228.
9. Huang D, Stulting RD, Carr JD, Thompson KP. Multiple regression and vector analyses of laser in situ keratomileusis for myopia and astigmatism. J Refract Surg. 1999. 15:538–549.
10. Vinciguerra P, Camesasca FI. Cross-cylinder ablation. Customized Corneal Ablation. The Quest for SuperVision. 2001. 28. SLACK Incorporated;325–326.
11. Salchow DJ, Zirm ME, Stieldorf C, Parisi A. Laser in situ keratomileusis for myopia and myopic astigmatism. J Cataract Refract Surg. 1998. 24:175–182.
12. Salah T, Waring GO III, Magharby AE, Moadel K, Grimm SB. Excimer Laser in situ Keratomileusis under a corneal flap for myopia of 2 to 20 diopters. Am J Ophthalmol. 1996. 121:143–155.
13. Choi YK, Suh Y, Joo CK. Myopic regression and its mechanism after LASIK surgery. J Korean Ophthalmol Soc. 2000. 41:620–626.
14. Fraenkel GE, Webber SK, Sutton GL. Toric laser in situ keratomileusis for myopic astigmatism using an ablatable mask. J Refract Surg. 1999. 15:111–117.
15. Zaldivar R, Davidorf JM, Oscherow S. Laser in situ keratomileusis for myopia from -5.50 to -11.50 diopters with astigmatism. J Refract Surg. 1998. 14:19–25.
16. Kim SJ, Lee YJ, Cha HW. Astigmatic correction of LASIK. J Korean Ophthalmol Soc. 2001. 42:967–971.
17. Hersh PS, Shah SI, Geiger D, Holladay JT. Corneal optical irregularity after excimer laser photorefractive keratectomy. The Summit Photorefractive Keratectomy Topography Study Group. J Cataract Refract Surg. 1996. 22:197–204.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download