Abstract
Strabismus fixus is very rare and the convergent form is rarely accompanied by blepharoptosis. We successfully treated one patient with high myopia whose convergent strabismus fixus, accompanied by blepharoptosis, became severe after cataract surgery. We report the case with a discussion of its pathology. We performed levator advancement operation, bilateral lateral rectus 11 mm resection, and bilateral medial rectus 8 mm recession. The suture was removed after maintaining temporary traction suture for 6 days. Blepharoptosis was completely corrected by postoperative 2 months. Esodeviation was 15PD, which was not increased compared with immediately after surgery. Satisfactory cosmetic outcome was obtained.
Strabismus fixus is a very rare form of strabismus that is characterized by severe adduction of the eye and ocular movement limitation. Although it is also considered as congenital fibrosis syndrome, it can develop after birth.1 Strabismus fixus develops after birth when severe rigidity develops in a medial rectus muscle a long time after paralysis of the lateral rectus, when inflammation is present in the extraocular muscle, or when adhesion of the extraocular muscle occurs in surrounding tissues after surgery.2
However, there has been no reported case where convergent strabismus fixus developed due to high myopia and extraocular muscle injury after cataract surgery.3,4 Furthermore, convergent strabismus fixus is rarely accompanied by blepharoptosis. The major cause of blepharoptosis in our patient was probably levator aponeurosis injury at the time of cataract surgery. However, we could not ignore the possibility that blepharoptosis had been present before cataract surgery, or that levator palpebrae muscle weakness was one clinical aspect of strabismus fixus. Although the development of strabismus is not rare after cataract surgery, the progression to strabismus fixus is. We therefore report this present case with high myopia that we successfully treated, and present a literature review.
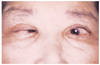
A 65-year-old female patient visited the present hospital due to progressive severe esodeviation, ocular movement limitation and blepharoptosis that had developed 20 years previously (Figs. 1, 2). She had undergone cataract surgery in both eyes 17 years previously, after which esodeviation in both eyes progressed quickly and the mild blepharoptosis, which was present before surgery became severe. After she underwent strabismus surgery 2 years later, esodeviation was improved but again deteriorated gradually. Although she underwent blepharoplasty for blepharoptosis 5 years previously, it was not corrected completely. There was no special aspect in her family history or systemic examination.
According to ocular examination, subjective uncorrected visual acuity was finger count 50cm in the right eye and 20/125 in the left eye. Both eyes were aphakic. Refractive power in the right eye was 5Dsph = -9.0Dcyl Ax 129°, and the left, +1.5Dsph = -4.5Dcyl Ax 87°. Corrected visual acuity was 20/125 in the right eye and the left eye visual acuity could not be corrected. The axial length was 33.8 mm and 34.2 mm, the interpalpebral fissure length was 3 mm and 12 mm, and MRD1 was -2 mm and 4mm, in the right and left eyes, respectively. According to levator function test, the distance was 5 mm and 7 mm, respectively. Neither eye showed Bell's phenomenon. Krimsky test showed the esodeviation to be more than 100PD. The hypofunction values were -3 in upgaze and -4 in adduction. Forced duction test was positive for supraduction and adduction in both eyes. Titmus test showed no stereopsis. Worth 4 dot test showed suppression in the right eye. The right pupil was tilted upward. According to fundus examination, both eyes showed severe myopic changes including lacquer cracks, temporal conus and staphyloma at the posterior pole.
The patient wanted surgery for cosmetic improvement. Surgery was performed with the patient under general anesthesia and levator advancement operation was done after dehiscent levator aponeurosis of the right eye was identified. Hang-back technique was used to recess the medial rectus muscle in the right eye by 8 mm. The medial rectus muscle in the left eye was recessed by 8 mm. The lateral rectus muscle in both eyes was resected by 11 mm. The left eye was abducted using a silicon tube and fixed with the traction suture onto the sclera around the lateral canthus. The silicone tube was removed at postoperative 6 days.
The patient did not complain of diplopia by postoperative 6 days and blepharoptosis in the right eye was completely corrected. Esodeviation in the primary position was 15PD. Adduction showed -1 functional decrease, which was little ocular movement limitation compared with before surgery. Cosmetically satisfactory results were obtained. Esodeviation had not increased when the patient came in for a follow-up examination at postoperative 2 months, and there was no recurrence of esodeviation (Fig. 3).
Convergent strabismus fixus is a type of strabismus characterized by medial rectus muscle fibrosis, contracture, and limitation of ocular horizontal movement causing severe esodeviation and the patient turning the head toward the fixating eye.1 Strabismus fixus is a congenital fibrosis of extraocular muscle along with inferior rectus fibrosis with blepharoptosis, generalized fibrosis, vertical retraction syndrome and congenital unilateral fibrosis.5 However, after Villascca6 reported that strabismus fixus developed after severe head trauma, many cases were reported on secondary strabismus fixus.3,4,6 When it is developed secondarily, strabismus fixus develops from various causes, not only medial rectus muscle contracture after lateral rectus muscle paralysis but also lateral rectus muscle weakness resulted when the lateral rectus muscle is pressed between the orbital rim and eyeball as the ocular expansion occurs in high myopia, the presence of various diseases causing extraocular muscle infection, diabetes, paralysis of the 6th nerve in both eyes in patients with head trauma or increased cerebral pressure.
Our patient developed strabismus fixus secondarily, possibly from high myopia and extraocular muscle injury during cataract surgery. Although there could be many causes for strabismus after cataract surgery, the factors directed with the extraocular muscle were toxicity by anesthetics and extraocular muscle injury during surgery resulting in extraocular muscle contracture, hyperactivity or paralysis.5 For example, the causes could be superior rectus muscle injury due to bridle suture and ischemic injury of extraocular muscle due to edema and hematoma after surgery. Many patients develop inflammatory reaction of extraocular muscle due to gentamicin subconjunctival injection and the degree of damage is especially large in elderly patients since the injured muscle does not readily regenerate.7 Although studies reported that injury to the superior rectus muscle, medial rectus muscle, lateral rectus muscle and inferior oblique muscle was also present, the extraocular muscle suffering injury most frequently is the inferior rectus muscle with Volkmann's ischemic contracture as its pathology.5,8 Guyton reported that widespread destruction and fibrosis of any extraocular muscle could happen from commonly used peribulbar or retrobulbar anesthesia.9 There has not been a report on the general degree of strabismus developed after cataract surgery or whether strabismus would progress to strabismus fixus. Thus, we could not tell whether the pathology involved in this case was only extraocular muscle contracture after cataract surgery. Furthermore, there was no record on the patient history of the preoperative and postoperative degree of deviation or the degree of ocular movement limitation. Thus, we could not ascertain the worsened degree of deviation and motion limitation after surgery. Nonetheless, we could not exclude the possibility of esodeviation due to lateral rectus muscle paralysis and fibrosis or contracture of the medial rectus muscle or upward motion limitation due to inferior rectus muscle injury as the cause of the strabismus that quickly progressed after cataract surgery.
It is well known that high myopia is the major pathology of strabismus fixus. Our patient also developed strabismus starting in her mid 40's, and the axial length was 33.8 mm in the right eye and 34.2 mm in the left eye, having relatively large eyes. The confirmation of inferior displacement and weakness of the lateral rectus muscle, that was suppressed from the globe and lateral ocular rim coming in contact on CT, probably helped in deciding whether high myopia or extraocular muscle contracture after cataract surgery would be the more important pathology. We believed that the main pathology in our patient was high myopia since we observed during surgery that the lateral rectus muscle was thinly elongated and that the lateral ocular rim and globe were situated close to each other. Although it was reported that the progression of convergent strabismus fixus caused by high myopia could be prevented through early intervention, the facts that all high myopia patients do not develop strabismus and that strabismus does not progress to strabismus fixus suggest that further studies are needed on the necessity or otherwise of screening patients by additional tests such as CT other than basic ocular exam.10,11 The findings that our patient had had poor vision since she was in her teen years and that her vision had deteriorated before esodeviation beca me severe suggest that her visual acuity did not deteriorate as a complication of strabismus fixus. The severely distorted ocular axis in strabismus fixus would cause optic nerve atrophy, ischemia, and central retinal artery occlusion, resulting in worsening of visual acuity.12
Our patient underwent second surgery for strabismus due to recurrence after the initial strabismus surgery 15 years previously. Convergent strabismus fixus is generally treated surgically by medial rectus recession and temporary traction suturing with the eye in the abducted state; however, lateral rectus resection is also performed when undercorrection is severe.1 Many surgical methods have been attempted since convergent strabismus fixus can recur easily. For example, in some cases permanent suture was done with traction suture by making holes with a microdrill due to recurrence by postoperative 8 weeks, despite the fact that traction suture was maintained for 5 days after bilateral lateral rectus muscle resection and bilateral medial rectus muscle recession. In our patient, we performed the usual surgery for convergent strabismus fixus since strabismus gradually progressed after initial surgery, complete correction was difficult, and the patient wanted cosmetic correction.13 The deviation did not increase but was fair at postoperative 2 months, at 15 PD, which was the angle observed at postoperative 6 days.
As for blepharoptosis, it is usually accompanied in divergent strabismus fixus but rarely in convergent strabismus fixus. We therefore believe that the blepharoptosis in our patient was a complication of cataract surgery.14 The rate of blepharoptosis development after cataract surgery is very high at 21%. Levator palpebrae muscle function is relatively normal and blepharoptosis develops within several weeks after surgery due to levator aponeurosis weakness, partial rupture or dehiscence. As in the mechanism of extraocular muscle injury mentioned earlier, the cause is superior rectus muscle complex injury and the rate of blepharoptosis increases with increasing patient age or surgery time.7,15 Blepharoptosis developed again probably due to recurrence of levator aponeurosis dehiscence developed at the time of cataract surgery, although our patient had undergone blepharoplasty 5 years before. The use of speculum during cataract surgery, bridle suture of the superior rectus muscle, and retrobulbar anesthesia would result in weak or dehiscent levator aponeurosis. On the other hand, bilateral levator palpebrae muscle function was decreased significantly with the distance being 5 mm in the right eye and 7 mm in the left eye. Furthermore, we could not confirm that blepharoptosis resulted as a complication of cataract surgery because mild blepharoptosis was present even before cataract surgery and progressed after cataract surgery.15,16 In other words, blepharoptosis could be one of the clinical aspects of convergent strabismus fixus with levator palpebrae muscle fibrosis being its cause, but we did not continue on with tests.
We report a successful outcome after surgically treating a patient with the rare combination of strabismus, convergent strabismus fixus, and blepharoptosis, which had worsened after cataract surgery
Figures and Tables
References
1. Mein J, Trimble R. Diagnosis and Management of Ocular Motility Disorders. 1991. 2nd ed. Oxford: Blackwell Scientific;351–352.
2. Jin YH. Strabismology. 2001. Ulsan: UUP;380–382.
3. Sharma P, Gupta NK, Arora R, Prakash P. Strabismus fixus convergens secondary to amyloidosis. J Pediatr Ophthalmol Strabismus. 1991. 28:236–237.
4. Prakash P, Gupta NK, Menon V, Chandra M. Myopic strabismus fixus convergens. Indian J Ophthalmol. 1989. 37:24–26.
5. Rosenbaum AL, Santiago AP. Clinical Strabismus Management: Principles and Surgical Techniques. 1999. Philadelphia: W.B. Saunders;363–378.
6. Villaseca A. Strabismus fixus. Am J Ophthalmol. 1957. 48:751–762.
7. Calson BM, Emerick S, Komorowski TE. Extraocular muscle regeneration in primates: local anesthetic induced lesions. Ophthalmology. 1992. 99:582.
8. Hamed LM. Strabismus presenting after cataract surgery. Ophthalmology. 1991. 98:247–252.
9. Guyton DL. Strabismus after cataract surgery. Am Orthopt J. 2001. 51:29–32.
10. Ohta M, Iwashige H, Hayashi T, Mauro T. Computed tomography findings in convergent strabismus fixus. Nippon Ganka Gakki Zasshi. 1995. 99:980–985.
11. Hayashi T, Maruo T. Acquired progressive esotropia and acquired strabismus fixus. Nippon Ganka Gakkai Zasshi. 1999. 103:604–611.
12. Mansour AM, Wang F, Henkind P, El-Baba F. Ocular complications in strabismus fixus convergens. Ophthalmologica. 1987. 195:161–166.
13. Yoon TJ, NA KS, Choi GJ. Surgical Correction of Convergent Strabismus Fixus. J Korean Ophthalmol Soc. 2001. 42:1816–1820.
14. Von Noorden GK, Campos EC. Binocular Vision and Ocular Motility: Theory and Management of Strabismus. 2002. 6th ed. St. Louis, MO: C.V. Mosby;471–472.
15. Ann DH, Lee YG, Kim HK, Hong YJ. Postoperative ptosis after cataract and glaucoma surgery. J Korean Ophthalmol Soc. 1998. 39:598–603.
16. Singh SK, Sekhar GC, Gupta S. Etiology of ptosis after cataract surgery. J Cataract Refract Surg. 1997. 23:1409–1413.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download