1. Beaugerie L, Seksik P, Nion-Larmurier I, Gendre JP, Cosnes J. Predictors of Crohn's disease. Gastroenterology. 2006; 130:650–656.
2. D’Haens G, Baert F, van Assche G, Caenepeel P, Vergauwe P, Tuynman H, De Vos M, van Deventer S, Stitt L, Donner A, et al. Early combined immunosuppression or conventional management in patients with newly diagnosed Crohn's disease: an open randomised trial. Lancet. 2008; 371:660–667.
3. Colombel JF, Sandborn WJ, Rutgeerts P, Enns R, Hanauer SB, Panaccione R, Schreiber S, Byczkowski D, Li J, Kent JD, et al. Adalimumab for maintenance of clinical response and remission in patients with Crohn's disease: the CHARM trial. Gastroenterology. 2007; 132:52–65.
4. Feagan BG, Panaccione R, Sandborn WJ, D’Haens GR, Schreiber S, Rutgeerts PJ, Loftus EV Jr, Lomax KG, Yu AP, Wu EQ, et al. Effects of adalimumab therapy on incidence of hospitalization and surgery in Crohn's disease: results from the CHARM study. Gastroenterology. 2008; 135:1493–1499.
5. Dassopoulos T, Sultan S, Falck-Ytter YT, Inadomi JM, Hanauer SB. American Gastroenterological Association Institute technical review on the use of thiopurines, methotrexate, and anti-TNF-α biologic drugs for the induction and maintenance of remission in inflammatory Crohn's disease. Gastroenterology. 2013; 145:1464–1478.e1-5.
6. D’Haens GR, Panaccione R, Higgins PD, Vermeire S, Gassull M, Chowers Y, Hanauer SB, Herfarth H, Hommes DW, Kamm M, et al. The London position statement of the World Congress of Gastroenterology on Biological Therapy for IBD with the European Crohn's and Colitis Organization: when to start, when to stop, which drug to choose, and how to predict response? Am J Gastroenterol. 2011; 106:199–212.
7. Coulter A. Partnerships with patients: the pros and cons of shared clinical decision-making. J Health Serv Res Policy. 1997; 2:112–121.
8. Coulter A, Entwistle V, Gilbert D. Sharing decisions with patients: is the information good enough? BMJ. 1999; 318:318–322.
9. Peake ST, Landy J, Hussein M, Tee CT, O’Connor M, Tyrrell T, Akbar A, Hart AL. Patient preference in choosing biological therapy in Crohn's disease. Inflamm Bowel Dis. 2011; 17:E79.
10. Allen PB, Lindsay H, Tham TC. How do patients with inflammatory bowel disease want their biological therapy administered? BMC Gastroenterol. 2010; 10:1–6.
11. Kim ES, Kim KO, Jang BI, Lee CK, Kim HJ, Lee KM, Kim YS, Eun CS, Jung SA, Yang SK, et al. Factors contributing to the preference of Korean patients with Crohn's disease when selecting an anti-tumor necrosis factor agent (CHOICE study). Gut Liver. 2016; 10:391–398.
12. Ye BD, Yang SK, Cho YK, Park SH, Yang DH, Yoon SM, Kim KJ, Byeon JS, Myung SJ, Yu CS, et al. Clinical features and long-term prognosis of Crohn's disease in Korea. Scand J Gastroenterol. 2010; 45:1178–1185.
13. Ooi CJ, Fock KM, Makharia GK, Goh KL, Ling KL, Hilmi I, Lim WC, Kelvin T, Gibson PR, Gearry RB, et al. The Asia-Pacific consensus on ulcerative colitis. J Gastroenterol Hepatol. 2010; 25:453–468.
14. Say R, Murtagh M, Thomson R. Patient’s preference for involvement in medical decision making: a narrative review. Patient Educ Couns. 2006; 60:102–114.
15. Thia KT, Loftus EV Jr, Sandborn WJ, Yang SK. An update on the epidemiology of inflammatory bowel disease in Asia. Am J Gastroenterol. 2008; 103:3167–3182.
16. Hou JK, El-Serag H, Thirumurthi S. Distribution and manifestations of inflammatory bowel disease in Asians, Hispanics, and African Americans: a systematic review. Am J Gastroenterol. 2009; 104:2100–2109.
17. Yang SK, Yun S, Kim JH, Park JY, Kim HY, Kim YH, Chang DK, Kim JS, Song IS, Park JB, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008; 14:542–549.
18. Ng SC, Tang W, Ching JY, Wong M, Chow CM, Hui AJ, Wong TC, Leung VK, Tsang SW, Yu HH, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-Pacific Crohn's and colitis epidemiology study. Gastroenterology. 2013; 145:158–165.e2.
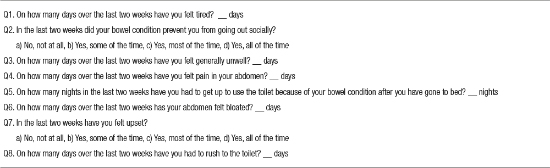
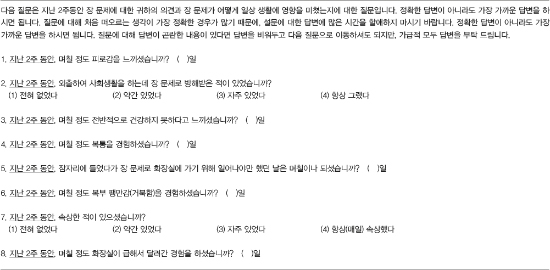
19. Alrubaiy L, Cheung WY, Dodds P, Hutchings HA, Russell IT, Watkins A, Williams JG. Development of a short questionnaire to assess the quality of life in Crohn's disease and ulcerative colitis. J Crohn's Colitis. 2015; 9:66–76.
20. Charnock D. The DISCERN Handbook. Abingdon: Radcliffe Medical Press;1998.
21. Chilton F, Collett RA. Treatment choices, preferences and decision-making by patients with rheumatoid arthritis. Musculoskelet Care. 2008; 6:1–14.
22. Williams EL, Edwards CJ. Patient preferences in choosing anti-TNF therapies-R1. Rheumatology (Oxford). 2006; 45:1575–1576.
23. Conrad S, Hüppe A, Raspe H. Preference of patients with inflammatory bowel disease regarding information and shared decision-making: results from a cross-sectional survey in Germany. Z Gastroenterol. 2012; 50:364–372.
24. Baars JE, Markus T, Kuipers EJ, van der Woude CJ. Patients’ preferences regarding shared decision-making in the treatment of inflammatory bowel disease: results from a patient-empowerment study. Digestion. 2010; 81:113–119.
25. Siegel CA, Lofland JH, Naim A, Gollins J, Walls DM, Rudder LE, Reynolds C. Gastroenterologists’ views of shared decision making for patients with inflammatory bowel disease. Dig Dis Sci. 2015; 60:2636–2645.
26. Siegel CA, Lofland JH, Naim A, Gollins J, Walls DM, Rudder LE, Reynolds C. Novel statistical approach to determine inflammatory bowel disease: patients’ perspectives on shared decision making. Patient. 2016; 9:79–89.
27. Sylwestrzak G, Liu J, Stephenson JJ, Ruggieri AP, DeVries A. Considering patient preferences when selecting anti-tumor necrosis factor therapeutic options. Am Health Drug Benefits. 2014; 7:71–81.
28. Kim NH, Jung YS, Moon CM, Lee SY, Kim ER, Kim YH, Lee CK, Lee SH, Kim JH, Huh KC, et al. Long-term clinical outcomes of Korean patient with Crohn's disease following early use of infliximab. Intest Res. 2014; 12:281–286.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download