1. Wanner C, Amann K, Shoji T. The heart and vascular system in dialysis. Lancet. 2016; 388:276–284.
2. Klarenbach SW, Tonelli M, Chui B, Manns BJ. Economic evaluation of dialysis therapies. Nat Rev Nephrol. 2014; 10:644–652.
3. Stack AG, Bloembergen WE. Prevalence and clinical correlates of coronary artery disease among new dialysis patients in the United States: a cross-sectional study. J Am Soc Nephrol. 2001; 12:1516–1523.
4. Stompór T. An overview of the pathophysiology of vascular calcification in chronic kidney disease. Perit Dial Int. 2007; 27:Suppl 2. S215–22.
5. London GM, Guérin AP, Marchais SJ, Métivier F, Pannier B, Adda H. Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality. Nephrol Dial Transplant. 2003; 18:1731–1740.
6. Bhan I, Thadhani R. Vascular calcification and ESRD: a hard target. Clin J Am Soc Nephrol. 2009; 4:Suppl 1. S102–5.
7. Blacher J, Guerin AP, Pannier B, Marchais SJ, London GM. Arterial calcifications, arterial stiffness, and cardiovascular risk in end-stage renal disease. Hypertension. 2001; 38:938–942.
8. Nitta K, Ogawa T. Aortic arch calcification and clinical outcome in patients with end-stage renal disease. Tohoku J Exp Med. 2011; 223:79–84.
9. Kim HS, Chung W, Kim AJ, Ro H, Chang JH, Lee HH, Jung JY. Circulating levels of soluble receptor for advanced glycation end product are inversely associated with vascular calcification in patients on haemodialysis independent of S100A12 (EN-RAGE) levels. Nephrology (Carlton). 2013; 18:777–782.
10. Fu MX, Wells-Knecht KJ, Blackledge JA, Lyons TJ, Thorpe SR, Baynes JW. Glycation, glycoxidation, and cross-linking of collagen by glucose. Kinetics, mechanisms, and inhibition of late stages of the Maillard reaction. Diabetes. 1994; 43:676–683.
11. Park S, Yoon SJ, Tae HJ, Shim CY. RAGE and cardiovascular disease. Front Biosci (Landmark Ed). 2011; 16:486–497.
12. Leurs P, Lindholm B. The AGE-RAGE pathway and its relation to cardiovascular disease in patients with chronic kidney disease. Arch Med Res. 2013; 44:601–610.
13. Cipollone F, Iezzi A, Fazia M, Zucchelli M, Pini B, Cuccurullo C, De Cesare D, De Blasis G, Muraro R, Bei R, et al. The receptor RAGE as a progression factor amplifying arachidonate-dependent inflammatory and proteolytic response in human atherosclerotic plaques: role of glycemic control. Circulation. 2003; 108:1070–1077.
14. Mori Y, Kosaki A, Kishimoto N, Kimura T, Iida K, Fukui M, Nakajima F, Nagahara M, Urakami M, Iwasaka T, et al. Increased plasma S100A12 (EN-RAGE) levels in hemodialysis patients with atherosclerosis. Am J Nephrol. 2009; 29:18–24.
15. Shiotsu Y, Mori Y, Nishimura M, Sakoda C, Tokoro T, Hatta T, Maki N, Iida K, Iwamoto N, Ono T, et al. Plasma S100A12 level is associated with cardiovascular disease in hemodialysis patients. Clin J Am Soc Nephrol. 2011; 6:718–723.
16. Yayar O, Eser B, Buyukbakkal M, Erdogan B, Ercan Z, Merhametsiz O, Haspulat A, Kali A, Yildirim T, Canbakan B, et al. Do elevated plasma S100A12 levels predict atherosclerosis in peritoneal dialysis patients? Ren Fail. 2015; 37:845–850.
17. Shiotsu Y, Mori Y, Nishimura M, Hatta T, Imada N, Maki N, Iida K, Iwamoto N, Matsuoka E, Tamagaki K, et al. Prognostic utility of plasma S100A12 levels to establish a novel scoring system for predicting mortality in maintenance hemodialysis patients: a two-year prospective observational study in Japan. BMC Nephrol. 2013; 14:16.
18. Isoyama N, Leurs P, Qureshi AR, Bruchfeld A, Anderstam B, Heimburger O, Bárány P, Stenvinkel P, Lindholm B. Plasma S100A12 and soluble receptor of advanced glycation end product levels and mortality in chronic kidney disease stage 5 patients. Nephrol Dial Transplant. 2015; 30:84–91.
19. Kalousová M, Kuběna AA, Benáková H, Dusilová-Sulková S, Tesař V, Zima T. EN-RAGE (extracellular newly identified receptor for advanced glycation end-products binding protein) and mortality of long-term hemodialysis patients: a prospective observational cohort study. Clin Biochem. 2012; 45:556–560.
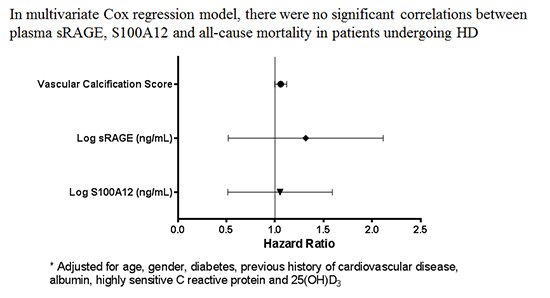
20. Nakashima A, Carrero JJ, Qureshi AR, Miyamoto T, Anderstam B, Bárány P, Heimbürger O, Stenvinkel P, Lindholm B. Effect of circulating soluble receptor for advanced glycation end products (sRAGE) and the proinflammatory RAGE ligand (EN-RAGE, S100A12) on mortality in hemodialysis patients. Clin J Am Soc Nephrol. 2010; 5:2213–2219.
21. Daugirdas JT. Simplified equations for monitoring Kt/V, PCRn, eKt/V, and ePCRn. Adv Ren Replace Ther. 1995; 2:295–304.
22. Kauppila LI, Polak JF, Cupples LA, Hannan MT, Kiel DP, Wilson PW. New indices to classify location, severity and progression of calcific lesions in the abdominal aorta: a 25-year follow-up study. Atherosclerosis. 1997; 132:245–250.
23. Pietzsch J, Hoppmann S. Human S100A12: a novel key player in inflammation? Amino Acids. 2009; 36:381–389.
24. Zakiyanov O, Kalousová M, Kříha V, Zima T, Tesař V. Serum S100A12 (EN-RAGE) levels in patients with decreased renal function and subclinical chronic inflammatory disease. Kidney Blood Press Res. 2011; 34:457–464.
25. Kalousová M, Hodková M, Kazderová M, Fialová J, Tesar V, Dusilová-Sulková S, Zima T. Soluble receptor for advanced glycation end products in patients with decreased renal function. Am J Kidney Dis. 2006; 47:406–411.
26. van de Logt F, Day AS. S100A12: a noninvasive marker of inflammation in inflammatory bowel disease. J Dig Dis. 2013; 14:62–67.
27. Meijer B, Hoskin T, Ashcroft A, Burgess L, Keenan JI, Falvey J, Gearry RB, Day AS. Total soluble and endogenous secretory receptor for advanced glycation endproducts (RAGE) in IBD. J Crohn’s Colitis. 2014; 8:513–520.
28. Baillet A. S100A8, S100A9 and S100A12 proteins in rheumatoid arthritis. Rev Med Interne. 2010; 31:458–461.
29. Pugliese G, Iacobini C, Blasetti Fantauzzi C, Menini S. The dark and bright side of atherosclerotic calcification. Atherosclerosis. 2015; 238:220–230.
30. Schmidt AM, Yan SD, Brett J, Mora R, Nowygrod R, Stern D. Regulation of human mononuclear phagocyte migration by cell surface-binding proteins for advanced glycation end products. J Clin Invest. 1993; 91:2155–2168.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download