See the article "".
See the reply "The Author's Response: ASA Physical Status Classification in Surgical Oncology and the Importance of Improving Inter-Rater Reliability" in Volume 32 on page 1213.
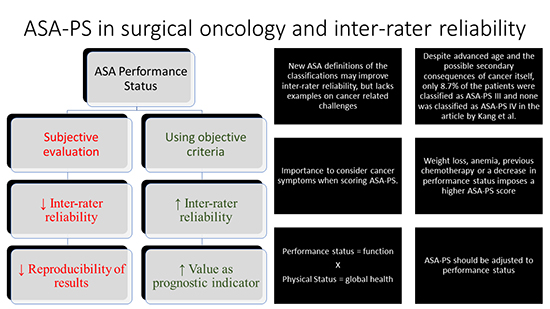
Graphical Abstract
To the Editor:
We read the article by Kang et al. (1) with great interest. The American Society of Anesthesiologists physical status (ASA-PS) classification was developed by the ASA more than 70 years ago and is still the most used tool for risk assessment of surgical patients by clinicians, surgeons, and anesthesiologists worldwide. It is very useful for preoperative stratification of surgical patients, despite being highly subjective and having moderate inter-rater reliability (2). The score has good predictive power for complications, mortality, and length of stay (23).
The subjectivity of the ASA-PS and good correlations with outcomes may be linked. The subjective nature of the score means that an immeasurable or unexpected clinical finding is translated into a worse classification and thus, a better anticipation of risk. However, more uniform application of the score seems necessary. Therefore, a few years ago, the American Society of Anesthesiologists (ASA) changed the definitions of the classifications and gave many examples of what kinds of patients should fit into each ASA-PS classification (4). According to the new ASA determination, patients who are pregnant, obese (30 kg/m2 < body mass index [BMI] < 40 kg/m2), or social alcohol drinkers are classified as ASA-PS II patients. The presence of grade III obesity, previous myocardial infarction, coronary artery disease, implanted coronary stents, stroke, or transient ischemic attack result in an ASA-PS III classification. This change may improve the inter-rater reliability for general surgical patients, but in surgical oncology, this may not be the case. Common consequences of cancer on global health are not shown as examples in the new ASA guidelines.
The high numbers of ASA-PS I and II patients in the study population deserve special attention. Only 8.7% of the patients were classified as ASA-PS III and none was classified as ASA-PS IV, despite the advanced ages in all groups. A common mistake in clinical practice is to score the ASA-PS “as if the patient did not have cancer.” Cancer is a systemic disease by definition. Weight loss, anemia, previous chemotherapy, or a decrease in performance status should impose a higher ASA-PS score. There may have been an underestimation of ASA-PS scores in the study by Kang et al. (1).
Underestimations of morbidity and mortality imply an improper choice of surgical procedure to be performed, inadequate information being provided during the patient consent process, and incorrect allocation during the postoperative period. Thus, inappropriate stratification may cause higher costs and worse outcomes.
The ASA-PS score is a measure of general physical status and thus global health. Compared with a measure of performance status, such as the Eastern Cooperative Oncology Group (ECOG) performance status classification, it may show results that are difficult to interpret. Evaluation of performance status during the preoperative anesthesia assessment is essential for postoperative planning. In cancer patients, the Karnofsky and ECOG performance status scales help to make clinical decisions together with global health scales, not in lieu of them. Performance assessment in metabolic equivalents (METS) is useful for not only cardiac assessment but also as a measurement of usual activity and for planning prehabilitation and rehabilitation protocols.
The high mortality among ASA-PS III patients with locally advanced disease probably reflects a worse physical status directly related to the cancer itself in the preoperative period. This could also result in a worse performance status. In ASA-PS III patients with a localized tumor, comorbidities may be responsible for the score. The ASA-PS cannot discriminate the cause of the inferior physical status. To conclude that the ASA-PS has an independent relationship with survival, it should be adjusted according to performance status.
References
1. Kang HW, Seo SP, Kim WT, Kim YJ, Yun SJ, Lee SC, Choi YD, Ha YS, Kim TH, Kwon TG, et al. Impact of the ASA physical status score on adjuvant chemotherapy eligibility and survival of upper tract urothelial carcinoma patients: a multicenter study. J Korean Med Sci. 2017; 32:335–342.
2. Sankar A, Johnson SR, Beattie WS, Tait G, Wijeysundera DN, Myles PS. Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br J Anaesth. 2014; 113:424–432.
3. Davenport DL, Ferraris VA, Hosokawa P, Henderson WG, Khuri SF, Mentzer RM Jr. Multivariable predictors of postoperative cardiac adverse events after general and vascular surgery: results from the patient safety in surgery study. J Am Coll Surg. 2007; 204:1199–1210.
4. American Society of Anesthesiologists. ASA physical status classification system [Internet]. accessed on 13 January 2017. Available at https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download