1. Jung KW, Won YJ, Kong HJ, Oh CM, Lee DH, Lee JS. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2011. Cancer Res Treat. 2014; 46:109–123.
2. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015; 136:E359–86.
3. Shin DW, Cho B, Kim SY, Jung JH, Park JH. Management of cancer survivors in clinical and public health perspectives: current status and future challenges in Korea. J Korean Med Sci. 2013; 28:651–657.
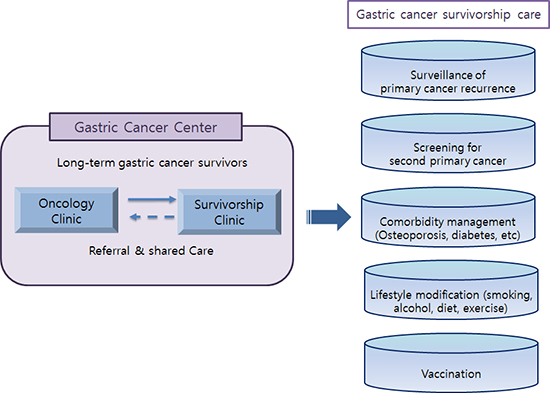
4. Oeffinger KC, McCabe MS. Models for delivering survivorship care. J Clin Oncol. 2006; 24:5117–5124.
5. Earle CC, Burstein HJ, Winer EP, Weeks JC. Quality of non-breast cancer health maintenance among elderly breast cancer survivors. J Clin Oncol. 2003; 21:1447–1451.
6. Nielsen JD, Palshof T, Mainz J, Jensen AB, Olesen F. Randomised controlled trial of a shared care programme for newly referred cancer patients: bridging the gap between general practice and hospital. Qual Saf Health Care. 2003; 12:263–272.
7. Shin DW, Park JH. Long-term survivorship clinics led by primary care physicians within the cancer center may be a good option for coordinated survivorship care. Cancer. 2014; 120:3752–3753.
8. National Institute on Alcohol Abuse and Alcoholism. The Physicians' Guide to Helping Patients with Alcohol Problems. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism;1995.
9. World Health Organization (CH). Global Recommendations on Physical Activity for Health. Geneva: World Health Organization;2010.
10. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2013; 36:S67–74.
11. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002; 106:3143–3421.
12. World Health Organization (CH). Guidelines for Preclinical Evaluation and Clinical Trials in Osteoporosis. Geneva: World Health Organization;1998.
13. Ministry of Health and Welfare. Korea Centers for Disease Control and Prevention. Korea Health Statistics 2013: Korea National Health and Nutrition Examination Survey (KNHANES VI-1). Cheongju: Korea Centers for Disease Control and Prevention;2014.
14. Humpel N, Magee C, Jones SC. The impact of a cancer diagnosis on the health behaviors of cancer survivors and their family and friends. Support Care Cancer. 2007; 15:621–630.
15. Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011; 35:303–308.
16. Lee MH, Kim HC, Ahn SV, Hur NW, Choi DP, Park CG, Suh I. Prevalence of dyslipidemia among Korean adults: Korea National Health and Nutrition Survey 1998-2005. Diabetes Metab J. 2012; 36:43–55.
17. Lee YH, Han SJ, Kim HC, Hyung WJ, Lim JS, Lee K, Lee HJ, Lee EY, Kang ES, Ahn CW, et al. Gastrectomy for early gastric cancer is associated with decreased cardiovascular mortality in association with postsurgical metabolic changes. Ann Surg Oncol. 2013; 20:1250–1257.
18. Yang J, Li C, Liu H, Gu H, Chen P, Liu B. Effects of subtotal gastrectomy and Roux-en-Y gastrojejunostomy on the clinical outcome of type 2 diabetes mellitus. J Surg Res. 2010; 164:e67–71.
19. Lim JS, Lee JI. Prevalence, pathophysiology, screening and management of osteoporosis in gastric cancer patients. J Gastric Cancer. 2011; 11:7–15.
20. Mariotto AB, Rowland JH, Ries LA, Scoppa S, Feuer EJ. Multiple cancer prevalence: a growing challenge in long-term survivorship. Cancer Epidemiol Biomarkers Prev. 2007; 16:566–571.
21. Tabuchi T, Ito Y, Ioka A, Miyashiro I, Tsukuma H. Incidence of metachronous second primary cancers in Osaka, Japan: update of analyses using population-based cancer registry data. Cancer Sci. 2012; 103:1111–1120.
22. Shin DW, Baik YJ, Kim YW, Oh JH, Chung KW, Kim SW, Lee WC, Yun YH, Cho J. Knowledge, attitudes, and practice on second primary cancer screening among cancer survivors: a qualitative study. Patient Educ Couns. 2011; 85:74–78.
23. Shin DW, Kim Y, Baek YJ, Mo HN, Choi JY, Cho J. Oncologists experience with second primary cancer screening: current practices and barriers and potential solutions. Asian Pac J Cancer Prev. 2012; 13:671–676.
24. Shih YC, Pan IW. Influenza vaccination among individuals with cancer and their family members. Am J Prev Med. 2010; 38:61–69.
25. Yoo S. Recent update in adult immunization. Korean J Fam Med. 2010; 31:345–354.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download