1. Mavragani CP, Moutsopoulos NM, Moutsopoulos HM. The management of Sjögren’s syndrome. Nat Clin Pract Rheumatol. 2006; 2:252–261.
2. Patel R, Shahane A. The epidemiology of Sjögren’s syndrome. Clin Epidemiol. 2014; 6:247–255.
3. Kim JY, Park SH, Kim SK, Hyun DS, Kum YS, Jung KJ, Choe JY. Lymphocytic interstitial pneumonia in primary Sjögren’s syndrome: a case report. Korean J Intern Med. 2011; 26:108–111.
4. Kim SM, Waters P, Vincent A, Kim SY, Kim HJ, Hong YH, Park KS, Min JH, Sung JJ, Lee KW. Sjogren’s syndrome myelopathy: spinal cord involvement in Sjogren’s syndrome might be a manifestation of neuromyelitis optica. Mult Scler. 2009; 15:1062–1068.
5. Kim YK, Song HC, Kim WY, Yoon HE, Choi YJ, Ki CS, Park CW, Yang CW, Kim J, Kim YS, et al. Acquired Gitelman syndrome in a patient with primary Sjögren syndrome. Am J Kidney Dis. 2008; 52:1163–1167.
6. Cho SG, Yi JH, Han SW, Kim HJ. Electrolyte imbalances and nephrocalcinosis in acute phosphate poisoning on chronic type 1 renal tubular acidosis due to Sjögren’s syndrome. J Korean Med Sci. 2013; 28:336–339.
7. Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, Daniels TE, Fox PC, Fox RI, Kassan SS, et al. Classification criteria for Sjögren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis. 2002; 61:554–558.
8. Shiboski SC, Shiboski CH, Criswell L, Baer A, Challacombe S, Lanfranchi H, Schiødt M, Umehara H, Vivino F, Zhao Y, et al. American College of Rheumatology classification criteria for Sjögren’s syndrome: a data-driven, expert consensus approach in the Sjögren’s International Collaborative Clinical Alliance cohort. Arthritis Care Res (Hoboken). 2012; 64:475–487.
9. Hay EM, Thomas E, Pal B, Hajeer A, Chambers H, Silman AJ. Weak association between subjective symptoms or and objective testing for dry eyes and dry mouth: results from a population based study. Ann Rheum Dis. 1998; 57:20–24.
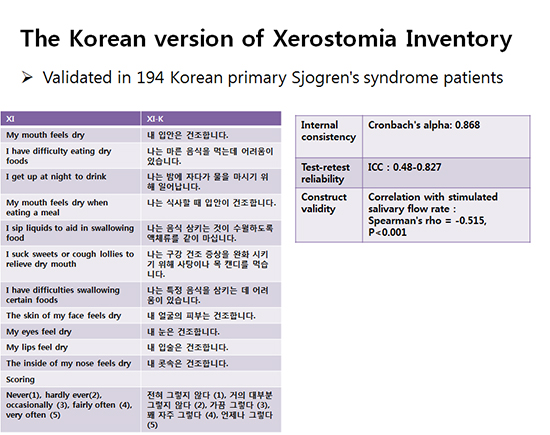
10. Thomson WM, Chalmers JM, Spencer AJ, Williams SM. The Xerostomia Inventory: a multi-item approach to measuring dry mouth. Community Dent Health. 1999; 16:12–17.
11. Cho HJ, Yoo JJ, Yun CY, Kang EH, Lee HJ, Hyon JY, Song YW, Lee YJ. The EULAR Sjogren’s syndrome patient reported index as an independent determinant of health-related quality of life in primary Sjogren’s syndrome patients: in comparison with non-Sjogren’s sicca patients. Rheumatology (Oxford). 2013; 52:2208–2217.
12. Serrano C, Fariña MP, Pérez C, Fernández M, Forman K, Carrasco M. Translation and validation of a Spanish version of the xerostomia inventory. Gerodontology. Forthcoming. 2015.
13. da Mata AD, da Silva Marques DN, Freitas FM, de Almeida Rato Amaral JP, Trindade RT, Barcelos FA, Vaz Patto JM. Translation, validation, and construct reliability of a Portuguese version of the Xerostomia Inventory. Oral Dis. 2012; 18:293–298.
14. He SL, Wang JH, Li M. Validation of the Chinese version of the Summated Xerostomia Inventory (SXI). Qual Life Res. 2013; 22:2843–2847.
15. Bland JM, Altman DG. Cronbach’s alpha. BMJ. 1997; 314:572.
16. Thomson WM, Williams SM. Further testing of the xerostomia inventory. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 89:46–50.
17. Borges BC, Fulco GM, Souza AJ, de Lima KC. Xerostomia and hyposalivation: a preliminary report of their prevalence and associated factors in Brazilian elderly diabetic patients. Oral Health Prev Dent. 2010; 8:153–158.
18. Leung KC, McMillan AS, Wong MC, Leung WK, Mok MY, Lau CS. The efficacy of cevimeline hydrochloride in the treatment of xerostomia in Sjögren’s syndrome in southern Chinese patients: a randomised double-blind, placebo-controlled crossover study. Clin Rheumatol. 2008; 27:429–436.






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download