This article has been
cited by other articles in ScienceCentral.
Abstract
Delayed hemothorax after blunt torso injury is rare, but might be associated with significant morbidity and mortality. We present a case of delayed hemothorax bleeding from phrenic artery injury in a 24-year-old woman. The patient suffered from multiple rib fractures on the right side, a right hemopneumothorax, thoracic vertebral injury and a pelvic bone fracture after a fall from a fourth floor window. Delayed hemothorax associated with phrenic artery bleeding, caused by a stab injury from a fractured rib segment, was treated successfully by a minimally invasive thoracoscopic surgery. Here, we have shown that fracture of a lower rib or ribs might be accompanied by delayed massive hemothorax that can be rapidly identified and promptly managed by thoracoscopic means.
Keywords: Thoracic Trauma, Hemothorax, Diaphragmatic Injury, Thoracic Surgery, Video-Assisted
INTRODUCTION
Delayed hemothorax after blunt torso injury is rare, but might be associated with significant morbidity and mortality. Hemothorax resulting from injuries involving the intercostal artery, internal mammary artery, vena azygos, pericardial rupture and diaphragm have been reported after blunt and penetrating thoracic traumas (
12). To the best of our knowledge, this is the first report of delayed hemothorax due to an injury caused by the sharpened ends of a broken rib penetrating the phrenic artery, without concomitant diaphragm injury.
CASE DESCRIPTION
A 24-year-old female presented to the emergency department shortly after a fall from a fourth floor window in 2012. On full assessment, there were multiple lower rib fractures on the right side (
Fig. 1), with a right hemopneumothorax, a flexion-extension injury of 11-12
th thoracic vertebrae, and a pelvic bone fracture. An intercostal drain was inserted and emergency vertebroplasty and internal fixation of the pelvis were performed. She was making excellent recovery; however, on the 13
th postoperative day, after incentive spirometry exercise and coughing, she became acutely unwell and complained of breathlessness. On examination, she was found to be hypotensive and tachycardic, with a dull right hemithorax and decreased air supply over the right lung field. She was resuscitated and a chest radiograph confirmed a white-out of the right hemithorax (
Fig. 2). Initially, 1.5 L of blood was drained from an inserted intercostal drain, and drainage continued at more than 100 mL/h. As the nature of the underlying injury was uncertain, we conducted an urgent computed tomography that revealed absence of intrathoracic vascular injury. Fluid resuscitation for hemodynamic stabilization was administered due to a suspicion of bleeding from intercostal vessels. This was followed by an urgent thoracoscopic exploration with a double-lumen endotracheal tube, performed through the previous intercostal drain site, and 2 additional working port sites in the 4
th and 8
th intercostal space along the posterior axillary line. The right pleural cavity was full of blood clots, amounting to approximately 2 L. The mediastinum, intercostal vessels, and lungs had no evidence of penetrating injury or inward displacement of rib fragment. Active arterial bleeding was found from a tear of musculophrenic artery in the dome of the right hemidiaphragm, corresponding to a broken right 11
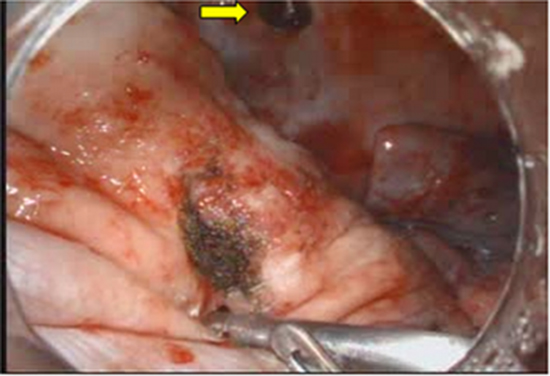
th rib end. We used a 10-mm aspiration/irrigation catheter that enabled us to perform an accurate lavage of the pleural cavity, and thus rapidly identify the bleeding sites with sufficient accuracy. Immediate hemostasis was achieved with thoracoscopic bovie cauterization (
Fig. 3). The patient made a completely uneventful postoperative recovery.
 | Fig. 1Three dimensional reconstructed computed tomography showing right lower rib fractures (arrow) and compression fracture of thoracic vertebrae. 
|
 | Fig. 2Chest X-ray on 13th postoperative day, showing right-sided hemothorax with chest tube placement. 
|
 | Fig. 3Thoracoscopic view of the lesion. (A) Active arterial bleeding of a phrenic artery. (B) Site of hemostasis, noting the proximity between fractured rib end (arrow) and bleeding site. 
|
DISCUSSION
About 10% of all trauma patients sustain rib fractures, and hemothorax, pneumothorax, and lesions of the lung are not uncommon. However, delayed penetrating internal thoracic injury by a fractured rib is rare. The mechanism of injury of the phrenic artery is unclear; however, it is reportedly believed to be associated with maneuvers such as chest physiotherapy, position change and violent coughing (
23). In view of the clinical manifestation following coughing in our patient, the forced expiration likely caused the abdominal wall muscles to contract and push the diaphragm upward and the fractured rib end inwards and downwards, resulting in stabbing of the right diaphragm phrenic artery.
Post-traumatic hemothorax in most cases require a closed treatment with insertion of a chest tube. In cases of massive hemothorax, as seen in our patient, once the essential diagnostic tests are conducted, an emergency thoracotomy must be performed to control underlying lesions since they are generally life-threatening. Although transcatheter arterial embolization may be a useful therapeutic modality in select patients (
4), concurrent hemodynamic instability frequently necessitates an emergency thoracotomy (
123).
While it is generally accepted that video-assisted thoracoscopic surgery (VATS) is indicated in various thoracic procedures, its indications for thoracic trauma can be controversial, especially in patients with hemodynamic instability. Fabbrucci et al. (
5) proposed a best approach treatment protocol by VATS in cases of moderate to severe traumatic hemothorax, which yielded excellent results, including an uneventful postoperative course, rapid resolution of the signs and symptoms of the chest problem, and no disabling sequelae (empyema and fibrothorax). Villavicencio et al. (
6) reviewed a total of more than 500 patients treated by VATS in numerous international centers. They found that VATS yielded optimal results in 90% of post-traumatic hemothorax cases with just 2% postoperative complications, and failed to recognize lesions in only 0.8% of cases. Previous studies and our own experience collectively suggests that in cases of massive hemothorax, treatment by VATS along with advanced perioperative care by an experienced anesthesiologist, may be a useful alternative to thoracotomy, particularly for young female patients.
Finally, delayed hemothorax from penetrating injuries to intrathoracic structures such as phrenic artery, may result from fractured ribs a number of days after the initial injuries. Caregivers of patients with multiple rib fractures need to be aware of this possibility. Continuous vigilance and a low index of clinical suspicion during the treatment and rehabilitation phases of the patient are needed. Such conditions might be resolved with the advent of minimally invasive surgery and the increased use of VATS.
ACKNOWLEDGMENT
This paper was presented at the International Conference of Emergency Medicine (ICEM) 2014 on 11-14 June, Hong Kong.
References
1. Sharma OP, Hagler S, Oswanski MF. Prevalence of delayed hemothorax in blunt thoracic trauma. Am Surg. 2005; 71:481–486.
2. Ashrafian H, Kumar P, Sarkar PK, DeSouza A. Delayed penetrating intrathoracic injury from multiple rib fractures. J Trauma. 2005; 58:858–859.
3. Daniel R, Naidu B, Khalil-Marzouk J. Cough-induced rib fracture and diaphragmatic rupture resulting in simultaneous abdominal visceral herniation into the left hemithorax and subcutaneously. Eur J Cardiothorac Surg. 2008; 34:914–915.
4. Hagiwara A, Yanagawa Y, Kaneko N, Takasu A, Hatanaka K, Sakamoto T, Okada Y. Indications for transcatheter arterial embolization in persistent hemothorax caused by blunt trauma. J Trauma. 2008; 65:589–594.
5. Fabbrucci P, Nocentini L, Secci S, Manzoli D, Bruscino A, Fedi M, Paroli GM, Santoni S. Video-assisted thoracoscopy in the early diagnosis and management of post-traumatic pneumothorax and hemothorax. Surg Endosc. 2008; 22:1227–1231.
6. Villavicencio RT, Aucar JA, Wall MJ Jr. Analysis of thoracoscopy in trauma. Surg Endosc. 1999; 13:3–9.