This article has been
cited by other articles in ScienceCentral.
Abstract
A 36-year-old male presented with progressive exertional dyspnea over months. Physical examination showed jugular venous distension, lung crecipitations, femoral bruit and pitting pedal edema. Echocardiogram showed a dilated right ventricle with severe pulmonary hypertension and a non collapsing inferior vena cava (IVC). On right heart catheterization, IVC oxygen saturation was noted at 92% suggesting arterial mixing; a computed tomography of the abdomen showed a fistula between the right common iliac artery to the right common iliac vein at L4 level and a massive IVC; this was linked to trauma from a disectomy done 16 years ago at L4–L5 level. Endovascular sealing with a 16 × 60 mm bifurcated stent graft (S & G Biotech, Seoul, Korea) was performed which led to complete resolution of the patient’s dyspnea. Iatrogenic vascular injury during lumbar disc surgery, although rare, can lead to high output cardiac failure developing over months to years.
Keywords: Arteriovenous Fistula, Herniated Disc Surgery, High Output Cardiac Failure, Endovascular Stent Graft
INTRODUCTION
The symptoms and signs of heart failure can occur in the setting of ‘high output heart failure.’ This condition is associated with several diseases including chronic anemia, systemic arterio-venous (AV) fistula, sepsis, hypercapnia and hyperthyroidism. High cardiac output state causing gradual changes of heart and finally ended up with decompensated heart failure (
1).
The cases of high output heart failure related to AV fistula during lumbar disc surgery are rarely reported. But the removal of a prolapsed disc, at the level of L4–L5 disc spaces where broad vascular bed is formed, has relatively high risk of complication with AV fistula than other levels of disc surgery (
2).
Herein, we report a case of successful endovascular intervention to repair iatrogenic iliac arteriovenous fistula which caused high output heart failure. This AV fistula was delayed complication from the previous discectomy.
CASE DESCRIPTION
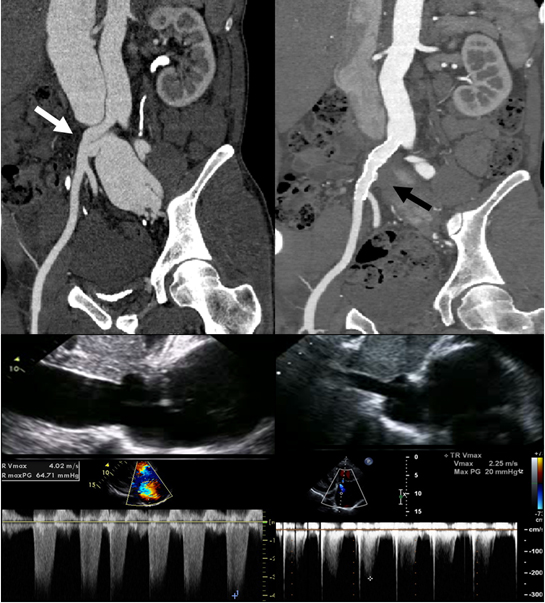
A 36-year-old Asian male was admitted to hospital for progressively worsening exertion dyspnea and orthopnea at January 28th 2013. Physical examination showed warm extremities, irregular heart rate, jugular venous distention, wet crackles in lungs, bilateral pitting edema and hepatomegaly. Relevant laboratory findings included a brain natriuretic peptide of 3,298 pg/mL. An electrocardiogram showed atrial fibrillation with right ventricular strain. Chest X-ray showed cardiomegaly and pulmonary congestion but the echocardiogram showed that an ejection fraction of 68%, increased chamber size, high pulmonary pressures of 65 mmHg with a tricuspid regurgitation (TR) maximum velocity (V-max) of 4.02 m/s, inferior vena cava (IVC) was non collapsible. A computed tomographic (CT) pulmonary angiogram showed increased pulmonary vascularity but no evidence of pulmonary embolism or parenchymal lung disease. A provisional diagnosis of ‘Primary Pulmonary Hypertension’ was made initially.
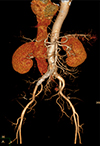
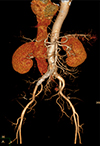
On right cardiac catheterization, oxygen saturation in the inferior vena cava was high at 92.3% indicating arterial mixing. A CT evaluation of aorta showed a fistula between right common iliac artery and right common iliac vein (
Fig. 1), this was linked to a herniated disc repair he had 16 years ago at lower lumbar level. The diagnosis was revised to ‘High output congestive heart failure with preserved ejection fraction due to an iatrogenic iliac arteriovenous fistula.’
Fig. 1
Computed tomography demonstrated the right common iliac artery and right common iliac venous fistula (white arrow).

The patient underwent an Endovascular repair with a 16 × 60 mm ‘S & G seal bifurcated graft’ (S & G Biotech, Seoul, Korea) which led to the resolution of his high output heart failure (
Figs. 2 and
3). After graft stent deployment, residual stenosis was approximately 50%–55% and adjuvant ballooning with Powerflex 12.0 × 40 mm was done. Puncture site was closed by perclosure. The procedure was successfully achieved.
Fig. 2
Computed tomography after the endovascular repair with the bifurcated graft placement and the resolution of common iliac arterio-venous (AV) fistula (black arrow).
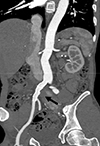
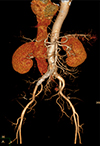
Fig. 3
Three dimensional reconstruction computed tomography of the bifurcated graft placement and the resolution of common iliac arterio-venous (AV) fistula.
The patient’s symptoms of heart failure including exertional dyspnea and orthopnea were resolved in 3 weeks. A follow up CT aorta confirmed the anatomic correction and 8 weeks later the Echocardiogram showed resolution of the dilated heart chambers, IVC diameter and decrease in pulmonary pressures with a reduction in the TR V-max to 2.25 m/s. Chest X-ray showed significant improvement of cardiomegaly and pulmonary congestion (
Fig. 4).
Fig. 4
Chest X-ray demonstrated the improvement of cardiomegaly and pulmonary congestion.

DISCUSSION
An elevated cardiac output with clinical heart failure is associated with several diseases including chronic anemia, systemic AV fistula, sepsis, hypercapnia and hyperthyroidism. Reduced systemic vascular resistance due to AV shunting or peripheral vasodilatation is the underlying physiologic problem. Iatrogenic systemic AV fistula is not only made for renal dialysis but also created by trauma (
1).
The types of vascular injury during lumbar disc operation are AV fistula, laceration or psedoaneurysm. AV fistula (67%) is the most common cause of vascular complication from lumbar disc operation. Especially the location commonly related to this complications are at the level of L4–L5 disc (59%) and common iliac artery (72%) (
2).
If there is a case of high output cardiac failure, chronic AV fistula formation should be excluded. The Doppler technique, Angiography and computed tomography are the imaging modalities to diagnose AV fistula. For the iliac AV fistulas, the arteriotomy along with suturing the lumen from inside and graft interposition has been preferred technique. However recently endovascular management becomes the preferred option due to the lower risk compared to conventional repair of an AV fistula (
2).
In our case, we decided to do endovascular repair with graft insertion. After bifemoral artery puncture, the S & G graft stent was deployed without immediate complication and AV fistula successfully sealed off. Along with graft stent deployment, the residual stenosis was fixed by adjuvant ballooning.
To recognize the AV fistula early, the suspicion of AV fistula is the most important when the patient present with exertional dyspnea or orthopnea with history of previous discectomy. We report a case of successful endovascular intervention to repair iatrogenic iliac arteriovenous fistula which caused high output heart failure. This AV fistula was delayed complication from the previous discectomy.
In conclusion, iatrogenic vascular injury during lumbar disc surgery (iliac artery more commonly injured than the iliac vein) is rare but can lead to high output cardiac failure developing over months to years and should be considered in the differential of heart failure in young patients (
23).