1. Glezen WP. Effect of maternal antibodies on the infant immune response. Vaccine. 2003; 21:3389–3392.
2. Albrecht P, Ennis FA, Saltzman EJ, Krugman S. Persistence of maternal antibody in infants beyond 12 months: mechanism of measles vaccine failure. J Pediatr. 1977; 91:715–718.
3. Cherry JD. Measles virus. In : Cherry JD, Harrison GJ, Kaplan SL, Hotez PJ, Steinbach WJ, editors. Feigin & Cherry's Textbook of Pediatric Infectious Diseases. 7th ed. Philadelphia, PA: Elsevier/Saunders;2014. p. 2723–2795.
4. American Academy of Pediatrics. Measles. In : Kimberlin DW, Brady MT, Jackson MA, Long SS, editors. Red Book: 2015 Report of the Committee on Infectious Diseases. 30th ed. Elk Grove Village, IL: American Academy of Pediatrics;2015. p. 535–547.
6. The Korean Pediatric Society. Measles, mumps, rubella vaccine. The Korean Pediatric Society. Immunization Guideline. 8th ed. Seoul: The Korean Pediatric Society;2015. p. 141–162.
7. Centers for Disease Control and Prevention (CDC). Elimination of measles--South Korea, 2001-2006. MMWR Morb Mortal Wkly Rep. 2007; 56:304–307.
8. Gans H, DeHovitz R, Forghani B, Beeler J, Maldonado Y, Arvin AM. Measles and mumps vaccination as a model to investigate the developing immune system: passive and active immunity during the first year of life. Vaccine. 2003; 21:3398–3405.
9. Cohen BJ, Audet S, Andrews N, Beeler J. WHO working group on measles plaque reduction neutralization test. Plaque reduction neutralization test for measles antibodies: description of a standardised laboratory method for use in immunogenicity studies of aerosol vaccination. Vaccine. 2007; 26:59–66.
10. Filia A, Brenna A, Panà A, Cavallaro GM, Massari M. Ciofi degli Atti ML. Health burden and economic impact of measles-related hospitalizations in Italy in 2002-2003. BMC Public Health. 2007; 7:169.
11. Leuridan E, Van Damme P. Passive transmission and persistence of naturally acquired or vaccine-induced maternal antibodies against measles in newborns. Vaccine. 2007; 25:6296–6304.
12. Hwang I. Results of 2nd MMR entry requirement, 2006-2011. Public Health Weekly Report. 2011; 4:749–751.
13. Korea Centers for Disease Control and Prevention. Disease web statistics system [Internet]. accessed on 19 June 2016. Available at
http://stat.cdc.go.kr.
14. Gagneur A, Pinquier D, Aubert M, Balu L, Brissaud O, De Pontual L, Gras Le Guen C, Hau-Rainsard I, Mory O, Picherot G, et al. Kinetics of decline of maternal measles virus-neutralizing antibodies in sera of infants in France in 2006. Clin Vaccine Immunol. 2008; 15:1845–1850.
16. Leuridan E, Hens N, Hutse V, Ieven M, Aerts M, Van Damme P. Early waning of maternal measles antibodies in era of measles elimination: longitudinal study. BMJ. 2010; 340:c1626.
17. Andrews N, Tischer A, Siedler A, Pebody RG, Barbara C, Cotter S, Duks A, Gacheva N, Bohumir K, Johansen K, et al. Towards elimination: measles susceptibility in Australia and 17 European countries. Bull World Health Organ. 2008; 86:197–204.
19. Nicoara C, Zäch K, Trachsel D, Germann D, Matter L. Decay of passively acquired maternal antibodies against measles, mumps, and rubella viruses. Clin Diagn Lab Immunol. 1999; 6:868–871.
20. Desgrandchamps D, Schaad UB, Glaus J, Tusch G, Heininger U. Seroprevalence of IgG antibodies against measles, mumps and rubella in Swiss children during the first 16 months of life. Schweiz Med Wochenschr. 2000; 130:1479–1486.
21. Leuridan E, Hens N, Hutse V, Aerts M, Van Damme P. Kinetics of maternal antibodies against rubella and varicella in infants. Vaccine. 2011; 29:2222–2226.
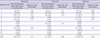
22. Oh SH, Kim HW, Lim Y, Lee H. Measles antibodies measured by plaque reduction neutralization test in infants during the first year of life. Korean J Pediatr. 2004; 47:827–832.
23. Kohler PF, Farr RS. Elevation of cord over maternal IgG immunoglobulin: evidence for an active placental IgG transport. Nature. 1966; 210:1070–1071.
24. Centers for Disease Control and Prevention (US). Measles. In : Hamborsky J, Kroger A, Wolfe C, editors. Epidemiology and Prevention of Vaccine-Preventable Diseases. 13th ed. Washington, D.C.: Public Health Foundation;2015. p. 209–230.
25. Rohani P, Drake JM. The decline and resurgence of pertussis in the US. Epidemics. 2011; 3:183–188.
26. Hellenbrand W, Beier D, Jensen E, Littmann M, Meyer C, Oppermann H, Wirsing von König CH, Reiter S. The epidemiology of pertussis in Germany: past and present. BMC Infect Dis. 2009; 9:22.
27. Kang HR, Kim SY, Cha HH, An YM, Park IA, Kang HJ, Eun BW. An outbreak of mumps in a high school, Seoul, 2013. Pediatr Infect Vaccine. 2015; 22:1–6.
28. Centers for Disease Control and Prevention (CDC). Update: mumps outbreak - New York and New Jersey, June 2009-January 2010. MMWR Morb Mortal Wkly Rep. 2010; 59:125–129.
29. Orenstein WA, Markowitz L, Preblud SR, Hinman AR, Tomasi A, Bart KJ. Appropriate age for measles vaccination in the United States. Dev Biol Stand. 1986; 65:13–21.
30. Kumar ML, Johnson CE, Chui LW, Whitwell JK, Staehle B, Nalin D. Immune response to measles vaccine in 6-month-old infants of measles seronegative mothers. Vaccine. 1998; 16:2047–2051.
31. Gans H, Yasukawa L, Rinki M, DeHovitz R, Forghani B, Beeler J, Audet S, Maldonado Y, Arvin AM. Immune responses to measles and mumps vaccination of infants at 6, 9, and 12 months. J Infect Dis. 2001; 184:817–826.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download