1. Lawes CM, Vander Hoorn S, Rodgers A; International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet. 2008; 371:1513–1518.
2. Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ; Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet. 2002; 360:1347–1360.
3. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005; 365:217–223.
4. Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993; 88:1973–1998.
5. Albert MA, Glynn RJ, Buring J, Ridker PM. Impact of traditional and novel risk factors on the relationship between socioeconomic status and incident cardiovascular events. Circulation. 2006; 114:2619–2626.
6. Wang Y, Chen J, Wang K, Edwards CL. Education as an important risk factor for the prevalence of hypertension and elevated blood pressure in Chinese men and women. J Hum Hypertens. 2006; 20:898–900.
7. Xu X, Niu T, Christiani DC, Weiss ST, Zhou Y, Chen C, Yang J, Fang Z, Jiang Z, Liang W, et al. Environmental and occupational determinants of blood pressure in rural communities in China. Ann Epidemiol. 1997; 7:95–106.
8. Minh HV, Byass P, Chuc NT, Wall S. Gender differences in prevalence and socioeconomic determinants of hypertension: findings from the WHO STEPs survey in a rural community of Vietnam. J Hum Hypertens. 2006; 20:109–115.
9. Conen D, Glynn RJ, Ridker PM, Buring JE, Albert MA. Socioeconomic status, blood pressure progression, and incident hypertension in a prospective cohort of female health professionals. Eur Heart J. 2009; 30:1378–1384.
10. Vathesatogkit P, Woodward M, Tanomsup S, Hengprasith B, Aekplakorn W, Yamwong S, Sritara P. Long-term effects of socioeconomic status on incident hypertension and progression of blood pressure. J Hypertens. 2012; 30:1347–1353.
11. Cha SH, Park HS, Cho HJ. Socioeconomic disparities in prevalence, treatment, and control of hypertension in middle-aged Koreans. J Epidemiol. 2012; 22:425–432.
12. Kim YM, Jung-Choi K. Socioeconomic inequalities in health risk factors in Korea. J Korean Med Assoc. 2013; 56:175–183.
13. Kim YJ, Kwak C. Prevalence and associated risk factors for cardiovascular disease: findings from the 2005, 2007 Korea National Health and Nutrition Examination Survey. Korean J Health Promot. 2011; 11:169–176.
14. Lee HY, Won JC, Kang YJ, Yoon SH, Choi EO, Bae JY, Sung MH, Kim HR, Yang JH, Oh J, et al. Type 2 diabetes in urban and rural districts in Korea: factors associated with prevalence difference. J Korean Med Sci. 2010; 25:1777–1783.
15. Colhoun HM, Hemingway H, Poulter NR. Socio-economic status and blood pressure: an overview analysis. J Hum Hypertens. 1998; 12:91–110.
16. Zhang Q, Wang Y. Trends in the association between obesity and socioeconomic status in U.S. adults: 1971 to 2000. Obes Res. 2004; 12:1622–1632.
17. Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007; 29:6–28.
18. Khang YH, Yun SC. Trends in general and abdominal obesity among Korean adults: findings from 1998, 2001, 2005, and 2007 Korea National Health and Nutrition Examination Surveys. J Korean Med Sci. 2010; 25:1582–1588.
19. Park JI, Baek H, Jung HH. Prevalence of chronic kidney disease in Korea: the Korean National Health and Nutritional Examination Survey 2011-2013. J Korean Med Sci. 2016; 31:915–923.
20. Shin C, Abbott RD, Lee H, Kim J, Kimm K. Prevalence and correlates of orthostatic hypotension in middle-aged men and women in Korea: the Korean health and genome study. J Hum Hypertens. 2004; 18:717–723.
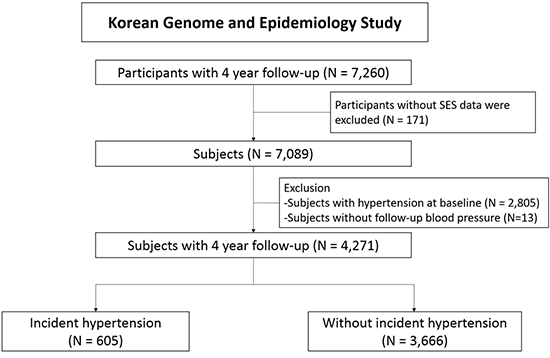
21. Baek TH, Lee HY, Lim NK, Park HY. Gender differences in the association between socioeconomic status and hypertension incidence: the Korean genome and epidemiology study (KoGES). BMC Public Health. 2015; 15:852.
22. Ha KH, Kim HC, Park S, Ihm SH, Lee HY. Gender differences in the association between serum gamma-glutamyltransferase and blood pressure change: a prospective community-based cohort study. J Korean Med Sci. 2014; 29:1379–1384.
23. 1999 World Health Organization-International Society of Hypertension guidelines for the management of hypertension. Guidelines Subcommittee. J Hypertens. 1999; 17:151–183.
24. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507–520.
26. Expert Consultation WH. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–163.
27. Ashfaq T, Anjum Q, Siddiqui H, Shaikh S, Vohra EA. Awareness of hypertension among patients attending primary health care centre and outpatient department of tertiary care hospital of Karachi. J Pak Med Assoc. 2007; 57:396–399.
28. Addo J, Smeeth L, Leon DA. Socioeconomic position and hypertension: a study of urban civil servants in Ghana. J Epidemiol Community Health. 2009; 63:646–650.
29. Min H, Chang J, Balkrishnan R. Sociodemographic risk factors of diabetes and hypertension prevalence in Republic of Korea. Int J Hypertens. 2010; 2010:410794.
30. Samal D, Greisenegger S, Auff E, Lang W, Lalouschek W. The relation between knowledge about hypertension and education in hospitalized patients with stroke in Vienna. Stroke. 2007; 38:1304–1308.
31. Paek KW, Chun KH. Moderating effects of interactions between dietary intake and socioeconomic status on the prevalence of metabolic syndrome. Ann Epidemiol. 2011; 21:877–883.
32. Pickering T. Cardiovascular pathways: socioeconomic status and stress effects on hypertension and cardiovascular function. Ann N Y Acad Sci. 1999; 896:262–277.
33. Baum A, Garofalo JP, Yali AM. Socioeconomic status and chronic stress. Does stress account for SES effects on health? Ann N Y Acad Sci. 1999; 896:131–144.
34. Jin HS, An AR, Choi HC, Lee SH, Shin DH, Oh SM, Seo YG, Cho BL. Physical activity level of Korean adults with chronic diseases: The Korean National Health and Nutritional Examination Survey, 2010-2012. Korean J Fam Med. 2015; 36:266–272.
35. Mensink GB, Deketh M, Mul MD, Schuit AJ, Hoffmeister H. Physical activity and its association with cardiovascular risk factors and mortality. Epidemiology. 1996; 7:391–397.
36. Andersen UO, Jensen G. Decreasing population blood pressure is not mediated by changes in habitual physical activity. Results from 15 years of follow-up. Blood Press. 2007; 16:28–35.
37. Park MY, Kim SH, Cho YJ, Chung RH, Lee KT. Association of leisure time physical activity and metabolic syndrome over 40 years. Korean J Fam Med. 2014; 35:65–73.
38. Lim S, Jang HC, Lee HK, Kimm KC, Park C, Cho NH. A rural-urban comparison of the characteristics of the metabolic syndrome by gender in Korea: the Korean health and genome study (KHGS). J Endocrinol Invest. 2006; 29:313–319.








 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download