This article has been
cited by other articles in ScienceCentral.
Abstract
Although liver function test abnormality is frequently noted in children, there is no report about the distribution of the etiology and natural recovery time of the abnormal liver function. From March 2005 to February 2014, clinical information was retrospectively collected from 559 children who had abnormal liver function and were hospitalized or visited the outpatient clinic at the Jeju National University Hospital. The etiology of abnormal liver function was classified into groups and the natural recovery time of abnormal liver function was analyzed. The etiological groups of 559 patients included ‘nonspecific hepatitis’ in 42 (7.5%), ‘infection’ in 323 (57.8%), ‘rheumatologic and autoimmune’ in 66 (11.8%), ‘nonalcoholic fatty liver disease’ in 57 (10.2%), ‘anatomic’ in 12 (2.1%), ‘toxic’ in 13 (2.1%), ‘metabolic’ in 8 (1.4%), ‘hematologic’ in 7 (1.3%), ‘hemodynamic’ in 4 (0.7%), and ‘others’ in 27 (4.8%). Among the ‘infection’ group (57.8%), the ‘viral infection in the respiratory tract’ subgroup, which had 111 patients (19.8%), was the most common. The natural recovery time of the abnormal liver function was 27 days (median) in ‘nonspecific hepatitis’, 13 days (median) in ‘viral respiratory tract disease’, 16 days (median) in ‘viral gastroenteritis’, 42 days (median) in ‘viral febrile illness”, and 7 days (median) in “Kawasaki disease”. The information on the natural recovery time of abnormal liver function may help the physician to perform good clinical consultation for patients and their parents.
Keywords: Liver Function Test, Children, Recovery
INTRODUCTION
In the pediatric ward of our hospital, we often encounter many children with abnormal liver function test (
1). Most patients only have the elevated aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels in the blood chemistry. AST and ALT elevation indicate hepatic injury, which is a primary hepatic disease or secondary to extrahepatic diseases. A few patients have jaundice or liver dysfunction associated with hepatic failure. The causes of the abnormal liver function test in children are multiple and more variable than those in adults. An overview of the etiology and grouping of the abnormal liver function test can guide the physician to take a good diagnostic approach in the patients.
We often observe slow spontaneous resolution of the elevated AST and ALT levels in the patients after recovery from their acute illness. Resolution may take from several weeks to several months. The parents wonder when their child’s abnormal liver function test result will be resolved.
Although liver function test abnormality is frequently noted in children, there is no report about the distribution of the etiology and there is no report about the natural recovery time of the abnormal liver function in diseases which show a transient abnormality in the test.
MATERIALS AND METHODS
From March 2005 to February 2014, clinical information was retrospectively collected from 559 children. All patients had abnormal liver function and were hospitalized or visited the outpatient clinic at the Jeju National University Hospital. Liver function abnormality was basically defined as elevated aspartate aminotransferase (AST) and alanine aminotransferase (ALT) higher than 50 IU/L, respectively. Liver function abnormality might occur in combination with or without an increased bilirubin level and/or protrombin time prolongation and low level of serum albumin. All patients in this study were differentially diagnosed using liver battery, hepatotrophic virus marker, muscle enzyme, serum ceruloplasmin level, viral markers in diseases suspecting systemic infection, and/or virus polymerase chase reaction (PCR) in diseases suspecting respiratory tract infection or gatrotenterisis, radiologic examination, and et Cetra.
We classified the etiology of the abnormal liver function test into 10 groups. These groups included ‘nonspecific hepatitis’, ‘infection’, ‘rheumatologic and autoimmune’, ‘nonalcoholic fatty liver disease (NAFLD)’, ‘anatomic’, ‘toxic’, ‘metabolic’, ‘hematologic’, ‘hemodynamic’, and ‘others’. ‘Nonspecific hepatitis’ is a disease which is characterized by only elevated AST and ALT levels without any other clue for suspecting other disease group or specific disease. ‘Infection’ group was further classified into 9 subgroups. These nine subgroups were ‘hepatotropic virus infection’, ‘cytomegalovirus (CMV) infection’, ‘epstein barr virus (EBV) infection’, ‘enterovirus infection’, ‘viral infection in the respiratory tract’, ‘viral acute gastroenteritis (AGE)’, ‘r/o viral febrile illness’, ‘other viral infection’, and ‘nonviral infection’. We also analyzed the natural recovery time of abnormal liver function in the disease group or subgroup showing an acute illness combined with abnormal liver function during some part of the study period.
Statistical analyses
Statistical analysis was performed using the Anova, Post Hoc (Bonferroni) of SPSS 18.0 (SPSS Inc., Chicago, IL, USA).
Ethics statement
This study had been done under the institutional review board (IRB No. JNUH 2014-07-005-002) in the Jeju National University Hospital. No informed consent form from the patients was received, because the study was just a retrospective study collecting clinical information in the electronic medical chart.
RESULTS
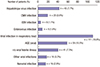
The age of these 559 children was 3.6 ± 4.4 years (mean ± SD), and it ranged from 1 month to 16 years. There were 338 male patients (60.5%) and 221 female patients (39.5%). Among these 559 children, the distribution of etiologic disease groups was as follows: ‘nonspecific hepatitis’, 42 patients (7.5%), ‘infection’, 323 patients (57.8%), ‘rheumatologic and autoimmune’, 66 patients (11.8%), ‘nonalcoholic fatty liver disease’, 57 patients (10.2%), ‘anatomic’, 12 patients (2.1%), ‘toxic’, 13 patients (2.3%), ‘metabolic’, 8 patients (1.4%), ‘hematologic’, 7 patients (1.3%), ‘hemodynamic’, 4 patients (0.7%), and ‘others’, 27 patients (4.8%) (
Fig. 1).
 | Fig. 1The distribution of the etiologic disease groups causing abnormal liver test in 559 children. The ‘Infection’ group was the most common, followed by ‘Rheumatologic and autoimmune’, ‘NAFLD’, ‘Nonspecific hepatitis’, ‘Others’, ‘Toxic’, and ‘Anatomic’ groups et cetera. 
|
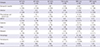
In the ‘infection’ (57.8%) group, the distribution of subgroups was as follows: ‘hepatotropic virus infection’, 43 patients (7.7%), ‘CMV infection’, 20 patients (3.6%), ‘EBV infection’, 6 patients (1.1%), ‘enterovirus infection’, 9 patients (1.6%), ‘viral infection in the respiratory tract’, 111 patients (19.8%), ‘viral AGE’, 59 patients (10.5%), ‘r/o viral febrile illness’, 41 patients (7.3%), ‘other viral infections’, 18 patients (3.2%), and ‘nonviral infection’, 16 patients (2.9%) (
Fig. 2).
 | Fig. 2The distribution of the etiologic disease subgroups in the ‘Infection’ group. The ‘Viral infection in the respiratory tract’ subgroup was the most common, followed by ‘viral AGE’, ‘hepatotropic virus infection’, ‘r/o viral febrile illness’, ‘CMV infection’, ‘Other viral infection’, and ‘Nonviral infection subgroups et cetera. 
|
The distribution of all diseases in each group is presented in
Table 1. In the ‘hepatotropic virus infection’ subgroup, hepatitis B virus infection was the most common. The ‘viral infections in the respiratory tract’ included influenza, adenovirus infection, respiratory syncytial virus infection, rhinovirus infection, upper respiratory infection, pneumonia, and bronchiolitis. The ‘viral AGE’ subgroup consisted of rotavirus infection and nonrotavirus infection. The ‘nonviral infection’ included urinary tract infection, orbital cellulitis, and acute acalculous cholecystitis et cetera. In ‘rheumatologic and autoimmune’ group, Kawasaki disease was the most common. The ‘anatomic’ group included biliary atresia. The ‘toxic’ group included drug induced hepatitis and TPN induced hepatitis. The ‘metabolic’ group consisted of Wilson disease and glycogen storage disease. The ‘hematologic’ group included leukemia, lymphoma, secondary hemochromatosis, pancytopenia and hemophagocytic lymphohistiocytosis. The ‘others’ group included neonatal hepatitis, cervical lymphadenitis, fulminant hepatic failure, and muscular dystrophy et cetera. Muscular dystrophy is a disorder mimicking abnormal liver function.
Table 1
Distribution of all diseases in each group and subgroup of children with abnormal liver function test

|
Groups |
Subgroups |
Diseases |
No. of patients (%) |
Age, yr
mean ± SD |
|
Nonspecific hepatitis |
|
42 (7.5%)
|
2.4 ± 3.1
|
|
Infection |
Hepatotropic virus Infection |
Hepatitis A virus infection |
11 |
12.4 ± 3.1 |
|
Hepatitis B virus infection |
31 |
7.0 ± 5.5 |
|
Hepatitis C virus infection |
1 |
2.4 ± 0.0 |
|
Subtotal |
43 (7.7%)
|
8.2 ± 5.6
|
|
CMV infection |
|
20 (3.6%)
|
1.3 ± 2.0
|
|
EBV infection |
|
6 (1.1%)
|
4.5 ± 2.7
|
|
Enterovirus infection |
|
9 (1.6%)
|
0.9 ± 0.5
|
|
Viral infection in the respiratory tract |
Influenza |
6 |
2.8 ± 3.2 |
|
Adenovirus infection |
13 |
1.1 ± 0.5 |
|
RSV infection |
9 |
0.8 ± 0.6 |
|
Rhinovirus infection |
2 |
0.9 ± 0.1 |
|
URI |
24 |
1.3 ± 1.1 |
|
LRI (Pneumonia, bronchiolitis) |
57 |
2.2 ± 2.7 |
|
Subtotal |
111 (19.8%)
|
1.7 ± 2.2
|
|
AGE(viral) |
Rotavirus infection |
26 |
1.3 ± 1.3 |
|
Non-Rota. AGE |
33 |
2.5 ± 3.5 |
|
Subtotal |
59 (10.5%)
|
1.9 ± 2.8
|
|
r/o Viral febrile illness |
|
41 (7.3%)
|
1.1 ± 1.8
|
|
Other viral infections |
Fever without a focus |
16 |
2.4 ± 3.9 |
|
Herpetic gingibostomatitis |
1 |
1.3 |
|
Rubella infection |
1 |
1.1 |
|
Subtotal |
18 (3.2%)
|
2.3 ± 3.7
|
|
Non-viral infection |
Urinary tract infection |
3 |
0.4 ± 0.2 |
|
Orbital cellulitis |
2 |
2.4 ± 1.8 |
|
Tonsillitis |
2 |
1.1 ± 0.2 |
|
4S |
1 |
1.7 |
|
Acute otitis media |
3 |
1.2 ± 0.2 |
|
r/o Sepsis |
2 |
0.7 ± 0.7 |
|
Scarlet fever |
1 |
2.8 |
|
Streptococcal pharyngitis |
1 |
7.7 |
|
Acute acalculous cholecystitis |
1 |
13.9 |
|
Subtotal |
16 (2.9%)
|
2.5 ± 3.5
|
|
Total |
|
323 (57.8%)
|
2.6 ± 3.8
|
|
Rheumatologic, autoimmune |
Kawasaki disease |
|
63 |
2.3 ± 1.7 |
|
JRA |
|
1 |
5.0 |
|
Autoimmune hepatitis |
|
1 |
13.1 |
|
Kikuchi disease |
|
1 |
14.9 |
|
Subtotal |
66 (11.8%)
|
2.7 ± 2.6
|
|
NAFLD |
|
57 (10.2%)
|
11.1 ± 2.6
|
|
Anatomic |
Biliary atresia |
|
12 (2.1%)
|
1.1 ± 2.8
|
|
Toxic |
Drug induced hepatitis |
|
10 |
2.6 ± 3.2 |
|
TPN induced hepatitis |
|
3 |
1.2 ± 1.3 |
|
Subtotal |
13 (2.3%)
|
2.3 ± 2.9
|
|
Metabolic |
Wilson disease |
|
5 |
9.9 ± 3.1 |
|
Glycogen storage disease |
|
3 |
8.3 ± 3.4 |
|
Subtotal |
8 (1.4%)
|
9.3 ± 3.3
|
|
Hematologic |
|
7 (1.3%)
|
3.2 ± 3.2
|
|
Hemodynamic (congestive heart failure) |
|
4 (0.7%)
|
0.3 ± 0.5
|
|
Others |
Hereditary pancreatitis |
|
1 |
5.6 |
|
Neonatal hepatitis |
|
8 |
0.2 ± 0.1 |
|
Fulminant hepatic failure |
|
5 |
6.3 ± 5.2 |
|
Cervical lymphadenitis |
|
7 |
6.5 ± 4.1 |
|
Diabetes Mellitus |
|
1 |
13.4 |
|
Acute epididymitis |
|
1 |
0.2 |
|
Idiopathic hepatosplenomegaly |
|
1 |
10.4 |
|
Muscular dystrophy |
|
3 |
2.2 ± 1.2 |
|
Subtotal |
27 (4.8%)
|
3.9 ± 4.6
|
|
Total
|
|
|
559 (100%)
|
3.6 ± 4.4
|

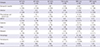
Laboratory test results for the etiological disease groups are presented in
Table 2. All groups showed variable AST and ALT levels. The ‘nonalcoholic fatty liver’ group showed relatively low AST/ALT level. Total bilirubin level in the ‘anatomic’ group was 9.93 ± 3.38 (mean ± SD) mg/dL. The ‘Anatomic’ group had a markedly higher total bilirubin than the other groups.
Table 2
Laboratory test results of of etiological groups in children with abnormal liver function test
|
Etiologies |
ALP (U/L)
(± SD) |
AST (IU/L)
(± SD) |
ALT (IU/L)
(± SD) |
T.Bil (mg/dL)
(± SD) |
WBC (/uL)
(± SD) |
CRP (mg/dL)
(± SD) |
|
Nonspecific hepatitis |
673 (± 285) |
274 (± 438) |
367 (± 659) |
0.59 (± 0.98) |
9,682 (± 4,387) |
0.89 (± 1.88) |
|
Infection |
714 (± 338) |
272 (± 481) |
345 (± 519) |
0.64 (± 1.22) |
11,349 (± 5,645) |
1.55 (± 2.60) |
|
Rheumatologic and autoimmune |
821 (± 388) |
197 (± 311) |
232 (± 256) |
1.03 (± 1.24) |
13,191 (± 4,622) |
8.73 (± 6.93) |
|
NAFLD |
812 (± 254) |
80 (± 48) |
161 (± 99) |
0.61 (± 0.48) |
8,074 (± 2,071) |
0.73 (± 1.25) |
|
Anatomic |
2,180 (± 1,136) |
236 (± 103) |
172 (± 76) |
9.93 (± 3.38) |
12,413 (± 6,103) |
0.27 (± 0.20) |
|
Toxic |
1,014 (± 619) |
443 (± 274) |
391 (± 300) |
1.66 (± 2.46) |
10,283 (± 5,420) |
2.4 (± 5.25) |
|
Metabolic |
647 (± 193) |
228 (± 169) |
261 (± 217) |
0.43 (± 0.18) |
8,763 (± 7,111) |
2.47 (± 3.11) |
|
Hematologic |
684 (± 210) |
411 (± 231) |
310 (± 267) |
4.41 (± 4.73) |
81,186 (± 173,467) |
3.29 (± 3.83) |
|
Hemodynamic |
714 (± 397) |
371 (± 292) |
182 (± 119) |
2.65 (± 1.77) |
13,854 (± 13,846) |
0.12 (± 0.07) |
|
Others |
848 (± 587) |
359 (± 525) |
352 (± 345) |
2.87 (± 3.17) |
9,933 (± 4,971) |
1.23 (± 1.40) |

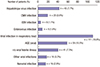
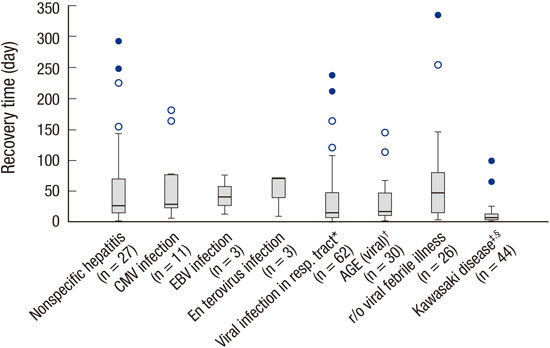
Natural recovery time of the abnormal liver function in the etiologic disease groups, which had a transient abnormal liver function test, is presented in
Fig. 3. The natural recovery time was analyzed in the patients who completed follow-up until recovery of abnormal liver function. The natural recovery time of 8 etiological subgroups was 27 days (median) ranged from 2 days to 293 days in the ‘nonspecific hepatitis’ subgroup, 29 days (median) ranged from 7 days to 181 days in the ‘CMV infection’ subgroup, 40 days (median) ranged from 13 days to 76 days in the ‘EBV infection’ subgroup, 70 days (median) ranged from 9 days to 71 days in the ‘enterovirus infection’ subgroup, 13 days (median) ranged from 2 days to 238 days in the ‘viral infection in the respiratory tract’ subgroup, 16 days (median) ranged from 2 days to 145 days in the ‘viral AGE’ subgroup, 42 days (median) ranged from 4 days to 335 days in the ‘r/o viral febrile illness’ subgroup, and 7 days (median) ranged from 2 days to 99 days in the ‘Kawasaki disease’ subgroup.
 | Fig. 3
Natural recovery time (median) of the abnormal liver function in etiologic disease subgroups, which had transient abnormal liver function test. The natural recovery time was analyzed in the patients of 8 etiological subgroups who completed follow-up until recovery of abnormal liver function. The natural recovery time of 8 etiological subgroups was 27 days (median) ranged from 2 days to 293 days in the ‘nonspecific hepatitis’ subgroup, 29 days (median) ranged from 7 days to 181 days in the ‘CMV infection’ subgroup, 40 days (median) ranged from 13 days to 76 days in the ‘EBV infection’ subgroup, 70 days (median) ranged from 9 days to 71 days in the ‘enterovirus infection’ subgroup, 13 days (median) ranged from 2 days to 238 days in the ‘viral infection in the respiratory tract’ subgroup, 16 days (median) ranged from 2 days to 145 days in the ‘viral AGE’ subgroup, 42 days (median) ranged from 4 days to 335 days in the ‘r/o viral febrile illness’ subgroup, and 7 days (median) ranged from 2 days to 99 days in the ‘Kawasaki disease’ subgroup.
CMV = cytomegalovirus, EBV = epstein bar virus, AGE = acute gastroenteritis.
*,†,‡Compared to the ‘r/o viral febrile illness’ subgroup: *P = 0.008, †P = 0.020, ‡P = 0.000; §Compared to the ‘nonspecific hepatitis’ subgroup: §P = 0.005 (ANOVA, Post Hoc analysis, Bonferroni).

|
DISCUSSION
Although liver function tests literally mean tests of hepatic synthetic function, liver function tests usually include hepatocellular enzymes, protein synthesis, bilirubin metabolism, and production of bile acids (
23). This definition might be based on the fact that almost all diseases with liver dysfunction have abnormal levels of hepatocellular enzymes in the clinical field. The elevation of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) indicates injury to the hepatocytes (
4). Most patients with primary or secondary liver diseases show abnormal elevation of AST and ALT (
5). All patients included in this study showed abnormal AST and ALT elevation. Small proportion of patients only had abnormal hepatic synthetic function or cholestatic processes in this study. Isolated elevation of AST and ALT may be either of hepatic origin or not, because the enzymes can also be derived from cardiac muscle, skeletal muscle, kidneys et cetera (
36). Except for only a few patients with muscular dystrophy in this study, almost all patients had abnormal AST and ALT levels of hepatic origin.
This is the first report which reveals the distribution of diseases causing liver function test abnormality in children and natural recovery time of the abnormal liver function after acute illness in some diseases. Etiological groups included ‘nonspeficic hepatitis’, ‘infection’, ‘rheumatologic and autoimmune’, ‘nonalcoholic fatty liver disease’, ‘anatomic’, ‘toxic’, ‘metabolic’, ‘hematologic’, ‘hemodynamic’, and ‘others’ (
Fig. 1). The groups were modified from Yazigi’s classification for hepatitis (
7). The ‘infection’ group (57.8%) was the most common among the 10 groups, followed by ‘rheumatologic and autoimmune’ group (11.8%), ‘non-alcoholic fatty liver disease (NAFLD)’ group (10.2%), ‘nonspecific hepatitis’ group (7.5%), ‘toxic’ group (2.3%), ‘anatomic’ group (biliary atresia, 2.1%), ‘metabolic’ group (1.4%) et cetera. The ‘nonspecific hepatitis’ is different from nonspecific reactive hepatitis. The ‘nonspecific hepatitis’ is a disease which is characterized by only elevated AST and ALT levels without any other clue for suspecting other disease group or specific disease. Nonspecific reactive hepatitis is just a pathological terminology, which indicates a nonspecific inflammatory process without any specific histologic findings suspecting a specific liver disease (
89).
In the ‘infection’ group (57.8%), the ‘viral infection in the respiratory tract’ subgroup was the most common (19.8%), followed by ‘viral acute gastroenteritis’ subgroup (10.5%), ‘hepatotropic virus infection’ subgroup (7.7%), ‘r/o viral febrile illness’ subgroup (7.3%), ‘cytomegalovirus infection’ subgroup (3.6%), ‘nonviral infection’ subgroup (2.9%) et cetera (
Fig. 2).
Spectrum and incidence of diseases causing liver function test abnormality greatly differ between children and adults. In adults, most of the abnormal liver function test includes acute and chronic hepatitis (
10). Acute hepatitis is classified into several etiological groups, which include acute hepatotropic viral hepatitis, acute nonhepatotropic viral hepatitis, drug-induced acute hepatitis, cholestatic hepatitis, nonspecific reactive hepatitis, and diseases mimicking acute hepatitis (
10). Chronic hepatitis is classified into the several etiological groups, which include chronic viral hepatitis, autoimmune hepatitis, drug-induced hepatitis, alcoholic liver disease, nonalcoholic fatty liver diseases and nonalcoholic steatohepatitis, metabolic diseases and other causes of chronic hepatitis, and diseases mimicking chronic hepatitis (
10).
Fig. 3 shows distribution of natural recovery time data in 8 etiological disease groups or subgroups. The median natural recovery time in the ‘Kawasaki disease’ group was shortest. The ‘viral infection in the respiratory tract’ was most common in the etiological subgroups (
Table 1) and had the natural recovery time with 13 days (median) ranged from 2 days to 238 days (
Fig. 3).
The limitations of this study are as follows: the first, this study was a retrospective study. Although the work-up for differential diagnosis of hepatitis was performed in almost all patients, it was not done in a few patients. The interval of the follow-up liver function test, in the patients who have slow natural recovery of abnormal liver function after acute illness, was not always the same.
In conclusion, the ‘Infection’ group was most common among the etiological groups causing abnormal liver function in children. Among the subgroups, ‘viral infection in the respiratory tract’ subgroup was the most common, followed by Kawasaki disease, NAFLD, Viral AGE, hepatotropic virus, ‘nonspecific hepatitis’, ‘r/o viral febrile illness’ subgroups et cetera. Wilson disease was found in about 1% of all patients with liver function abnormality. The overview of the distribution causing liver function abnormality can make the diagnostic approach easier. The information about the natural recovery time will help the physician to perform good consultation for the patients and their parents, who have abnormal liver function tests in some disease subgroups.







 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download