1. Kalin R, Stanton MS. Current clinical issues for MRI scanning of pacemaker and defibrillator patients. Pacing Clin Electrophysiol. 2005; 28:326–328.
2. Levine GN, Gomes AS, Arai AE, Bluemke DA, Flamm SD, Kanal E, Manning WJ, Martin ET, Smith JM, Wilke N, et al. Safety of magnetic resonance imaging in patients with cardiovascular devices: an American Heart Association scientific statement from the Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology, and the Council on Cardiovascular Radiology and Intervention: endorsed by the American College of Cardiology Foundation, the North American Society for Cardiac Imaging, and the Society for Cardiovascular Magnetic Resonance. Circulation. 2007; 116:2878–2891.
3. Roguin A, Schwitter J, Vahlhaus C, Lombardi M, Brugada J, Vardas P, Auricchio A, Priori S, Sommer T. Magnetic resonance imaging in individuals with cardiovascular implantable electronic devices. Europace. 2008; 10:336–346.
4. Wilkoff BL, Bello D, Taborsky M, Vymazal J, Kanal E, Heuer H, Hecking K, Johnson WB, Young W, Ramza B, et al. Magnetic resonance imaging in patients with a pacemaker system designed for the magnetic resonance environment. Heart Rhythm. 2011; 8:65–73.
5. Mitka M. First MRI-safe pacemaker receives conditional approval from FDA. JAMA. 2011; 305:985–986.
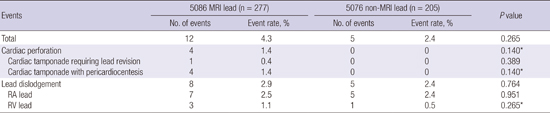
6. Elmouchi DA, Rosema S, Vanoosterhout SM, Khan M, Davis AT, Gauri AJ, Finta B, Woelfel AK, Chalfoun NT. Cardiac perforation and lead dislodgement after implantation of a MR-conditional pacing lead: a single-center experience. Pacing Clin Electrophysiol. 2014; 37:4–10.
7. Rickard J, Taborsky M, Bello D, Johnson WB, Ramza B, Chang Y, Wilkoff BL. Short- and long-term electrical performance of the 5086MRI pacing lead. Heart Rhythm. 2014; 11:222–229.
8. Acha MR, Keaney JJ, Lubitz SA, Milan DJ, Mansour M, Heist KE, Ptaszek LM, Singh JP, Blendea D, Mela T. Increased perforation risk with an MRI-conditional pacing lead: a single-center study. Pacing Clin Electrophysiol. 2015; 38:334–342.
9. Forleo GB, Santini L, Della Rocca DG, Romano V, Papavasileiou LP, Magliano G, Sgueglia M, Romeo F. Safety and efficacy of a new magnetic resonance imaging-compatible pacing system: early results of a prospective comparison with conventional dual-chamber implant outcomes. Heart Rhythm. 2010; 7:750–754.
10. Gimbel JR, Bello D, Schmitt M, Merkely B, Schwitter J, Hayes DL, Sommer T, Schloss EJ, Chang Y, Willey S, et al. Randomized trial of pacemaker and lead system for safe scanning at 1.5 Tesla. Heart Rhythm. 2013; 10:685–691.
11. Reddy VY, Exner DV, Cantillon DJ, Doshi R, Bunch TJ, Tomassoni GF, Friedman PA, Estes NA 3rd, Ip J, Niazi I, et al. Percutaneous implantation of an entirely intracardiac leadless pacemaker. N Engl J Med. 2015; 373:1125–1135.
12. Link MS, Estes NA 3rd, Griffin JJ, Wang PJ, Maloney JD, Kirchhoffer JB, Mitchell GF, Orav J, Goldman L, Lamas GA. Complications of dual chamber pacemaker implantation in the elderly. Pacemaker Selection in the Elderly (PASE) Investigators. J Interv Card Electrophysiol. 1998; 2:175–179.
13. Ghani A, Delnoy PP, Ramdat Misier AR, Smit JJ, Adiyaman A, Ottervanger JP, Elvan A. Incidence of lead dislodgement, malfunction and perforation during the first year following device implantation. Neth Heart J. 2014; 22:286–291.
14. Armaganijan LV, Toff WD, Nielsen JC, Andersen HR, Connolly SJ, Ellenbogen KA, Healey JS. Are elderly patients at increased risk of complications following pacemaker implantation? A meta-analysis of randomized trials. Pacing Clin Electrophysiol. 2012; 35:131–134.
15. Pakarinen S, Oikarinen L, Toivonen L. Short-term implantation-related complications of cardiac rhythm management device therapy: a retrospective single-centre 1-year survey. Europace. 2010; 12:103–108.
16. Udo EO, Zuithoff NP, van Hemel NM, de Cock CC, Hendriks T, Doevendans PA, Moons KG. Incidence and predictors of short- and long-term complications in pacemaker therapy: the FOLLOWPACE study. Heart Rhythm. 2012; 9:728–735.
17. Mahapatra S, Bybee KA, Bunch TJ, Espinosa RE, Sinak LJ, McGoon MD, Hayes DL. Incidence and predictors of cardiac perforation after permanent pacemaker placement. Heart Rhythm. 2005; 2:907–911.
18. Migliore F, Zorzi A, Bertaglia E, Leoni L, Siciliano M, De Lazzari M, Ignatiuk B, Veronese M, Verlato R, Tarantini G, et al. Incidence, management, and prevention of right ventricular perforation by pacemaker and implantable cardioverter defibrillator leads. Pacing Clin Electrophysiol. 2014; 37:1602–1609.
19. Sterliński M, Przybylski A, Maciag A, Syska P, Pytkowski M, Lewandowski M, Kowalik I, Firek B, Kołsut P, Religa G, et al. Subacute cardiac perforations associated with active fixation leads. Europace. 2009; 11:206–212.
20. Laborderie J, Barandon L, Ploux S, Deplagne A, Mokrani B, Reuter S, Le Gal F, Jais P, Haissaguerre M, Clementy J, et al. Management of subacute and delayed right ventricular perforation with a pacing or an implantable cardioverter-defibrillator lead. Am J Cardiol. 2008; 102:1352–1355.
21. Ohlow MA, Lauer B, Brunelli M, Geller JC. Incidence and predictors of pericardial effusion after permanent heart rhythm device implantation: prospective evaluation of 968 consecutive patients. Circ J. 2013; 77:975–981.
22. Ellenbogen KA, Hellkamp AS, Wilkoff BL, Camunãs JL, Love JC, Hadjis TA, Lee KL, Lamas GA. Complications arising after implantation of DDD pacemakers: the MOST experience. Am J Cardiol. 2003; 92:740–741.
23. Nowak B, Misselwitz B; Expert Committee Pacemaker, Institute of Quality Assurance Hessen. Effects of increasing age onto procedural parameters in pacemaker implantation: results of an obligatory external quality control program. Europace. 2009; 11:75–79.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download