INTRODUCTION
CASE DESCRIPTION
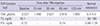
Table 1
Result of TRH stimulation test (TRH 400 μg IV)
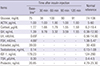
Table 2
Result of insulin tolerance test and baseline hormonal profile (regular insulin 0.1 U/kg IV)
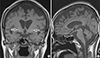
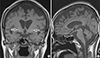
Fig. 2
Journal List > J Korean Med Sci > v.31(8) > 1023064
Hae Won Lee 
https://orcid.org/http://orcid.org/0000-0002-7744-2187
Jin Du Kang 
https://orcid.org/http://orcid.org/0000-0003-2191-7718
Chang Woo Yeo 
https://orcid.org/http://orcid.org/0000-0001-5753-4191
Sung Woon Yoon 
https://orcid.org/http://orcid.org/0000-0001-7073-020X
Kwang Jae Lee 
https://orcid.org/http://orcid.org/0000-0001-5468-6499
Mun Ki Choi 
https://orcid.org/http://orcid.org/0000-0002-5725-7128