1. Warwick D, Williams MH, Bannister GC. Death and thromboembolic disease after total hip replacement. A series of 1162 cases with no routine chemical prophylaxis. J Bone Joint Surg Br. 1995; 77:6–10.
2. Warwick D. New concepts in orthopaedic thromboprophylaxis. J Bone Joint Surg Br. 2004; 86:788–792.
3. Coventry MB, Nolan DR, Beckenbaugh RD. “Delayed” prophylactic anticoagulation: a study of results and complications in 2,012 total hip arthroplasties. J Bone Joint Surg Am. 1973; 55:1487–1492.
4. Clagett GP, Anderson FA Jr, Heit J, Levine MN, Wheeler HB. Prevention of venous thromboembolism. Chest. 1995; 108:312S–34S.
5. Miric A, Lombardi P, Sculco TP. Deep vein thrombosis prophylaxis: a comprehensive approach for total hip and total knee arthroplasty patient populations. Am J Orthop. 2000; 29:269–274.
6. Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, Colwell CW. American College of Chest Physicians. Prevention of venous thromboembolism: American college of chest physicians evidence-based clinical practice guidelines (8th edition). Chest. 2008; 133:381S–453S.
7. Lieberman JR, Pensak MJ. Prevention of venous thromboembolic disease after total hip and knee arthroplasty. J Bone Joint Surg Am. 2013; 95:1801–1811.
8. Kakkar VV, Stringer MD. Prophylaxis of venous thromboembolism. World J Surg. 1990; 14:670–678.
9. Leijtens B, Kremers van de Hei K, Jansen J, Koëter S. High complication rate after total knee and hip replacement due to perioperative bridging of anticoagulant therapy based on the 2012 ACCP guideline. Arch Orthop Trauma Surg. 2014; 134:1335–1341.
10. Klatsky AL, Armstrong MA, Poggi J. Risk of pulmonary embolism and/or deep venous thrombosis in Asian-Americans. Am J Cardiol. 2000; 85:1334–1337.
11. White RH, Zhou H, Gage BF. Effect of age on the incidence of venous thromboembolism after major surgery. J Thromb Haemost. 2004; 2:1327–1333.
12. White RH, Zhou H, Murin S, Harvey D. Effect of ethnicity and gender on the incidence of venous thromboembolism in a diverse population in California in 1996. Thromb Haemost. 2005; 93:298–305.
13. Nguyen HN, Fujiyoshi A, Abbott RD, Miura K. Epidemiology of cardiovascular risk factors in Asian countries. Circ J. 2013; 77:2851–2859.
14. Brush BE, Heldt TJ. A device for relief of lymphedema. J Am Med Assoc. 1955; 158:34–35.
15. Morris RJ, Woodcock JP. Evidence-based compression: prevention of stasis and deep vein thrombosis. Ann Surg. 2004; 239:162–171.
16. Comerota AJ, Chouhan V, Harada RN, Sun L, Hosking J, Veermansunemi R, Comerota AJ Jr, Schlappy D, Rao AK. The fibrinolytic effects of intermittent pneumatic compression: mechanism of enhanced fibrinolysis. Ann Surg. 1997; 226:306–313.
17. Kessler CM, Hirsch DR, Jacobs H, MacDougall R, Goldhaber SZ. Intermittent pneumatic compression in chronic venous insufficiency favorably affects fibrinolytic potential and platelet activation. Blood Coagul Fibrinolysis. 1996; 7:437–446.
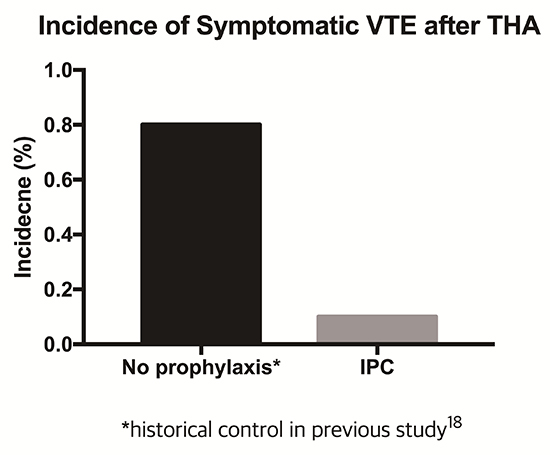
18. Kang BJ, Lee YK, Kim HJ, Ha YC, Koo KH. Deep venous thrombosis and pulmonary embolism are uncommon in East Asian patients after total hip arthroplasty. Clin Orthop Relat Res. 2011; 469:3423–3428.
19. Price MJ. Monitoring platelet function to reduce the risk of ischemic and bleeding complications. Am J Cardiol. 2009; 103:35A–9A.
20. Cohen AT, Skinner JA, Kakkar VV. Antiplatelet treatment for thromboprophylaxis: a step forward or backwards? BMJ. 1994; 309:1213–1215.
21. Huber O, Bounameaux H, Borst F, Rohner A. Postoperative pulmonary embolism after hospital discharge. An underestimated risk. Arch Surg. 1992; 127:310–313.
22. Wroblewski BM, Siney PD, White R. Fatal pulmonary embolism after total hip arthroplasty. Seasonal variation. Clin Orthop Relat Res. 1992; 222–224.
23. Carson JL, Kelley MA, Duff A, Weg JG, Fulkerson WJ, Palevsky HI, Schwartz JS, Thompson BT, Popovich J Jr, Hobbins TE, et al. The clinical course of pulmonary embolism. N Engl J Med. 1992; 326:1240–1245.
24. Werbel GB, Shybut GT. Acute compartment syndrome caused by a malfunctioning pneumatic-compression boot. A case report. J Bone Joint Surg Am. 1986; 68:1445–1446.
25. Won SH, Lee YK, Suh YS, Koo KH. Extensive bullous complication associated with intermittent pneumatic compression. Yonsei Med J. 2013; 54:801–802.
26. Sugano N, Miki H, Nakamura N, Aihara M, Yamamoto K, Ohzono K. Clinical efficacy of mechanical thromboprophylaxis without anticoagulant drugs for elective hip surgery in an Asian population. J Arthroplasty. 2009; 24:1254–1257.
27. Piovella F, Wang CJ, Lu H, Lee K, Lee LH, Lee WC, Turpie AG, Gallus AS, Planès A, Passera R, et al. Deep-vein thrombosis rates after major orthopedic surgery in Asia. An epidemiological study based on postoperative screening with centrally adjudicated bilateral venography. J Thromb Haemost. 2005; 3:2664–2670.
28. Leizorovicz A, Turpie AG, Cohen AT, Wong L, Yoo MC, Dans A; SMART Study Group. Epidemiology of venous thromboembolism in Asian patients undergoing major orthopedic surgery without thromboprophylaxis. The SMART study. J Thromb Haemost. 2005; 3:28–34.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download