1. Kim YL. The quality of life in hysterectomy women and social support. Korean J Fam Welf. 2010; 15:49–71.
2. Ministry of Health and Welfare (KR). Korea Institute for Health and Social Affairs. For 2011, Patient Survey In-Depth Analysis: Policy Rreport 2013-11. Seoul: Korea Institute for Health and Social Affairs;2013.
3. Raedah A, Togas T. Treatment options for uterine myoma. Int Congr Ser. 2004; 1266:197–201.
5. Somigliana E, Vercellini P, Daguati R, Pasin R, De Giorgi O, Crosignani PG. Fibroids and female reproduction: a critical analysis of the evidence. Hum Reprod Update. 2007; 13:465–476.
6. Song E. Ultrasound imaging guided high intensity focused ultrasound (HIFU) may be a safe tool to ablate uterine myoma. Korean J Obstet Gynecol. 2009; 52:843–849.
7. Smart OC, Hindley JT, Regan L, Gedroyc WM. Magnetic resonance guided focused ultrasound surgery of uterine fibroids--the tissue effects of GnRH agonist pre-treatment. Eur J Radiol. 2006; 59:163–167.
8. Wang W, Wang Y, Wang T, Wang J, Wang L, Tang J. Safety and efficacy of US-guided high-intensity focused ultrasound for treatment of submucosal fibroids. Eur Radiol. 2012; 22:2553–2558.
9. Zhang X, Li K, Xie B, He M, He J, Zhang L. Effective ablation therapy of adenomyosis with ultrasound-guided high-intensity focused ultrasound. Int J Gynaecol Obstet. 2014; 124:207–211.
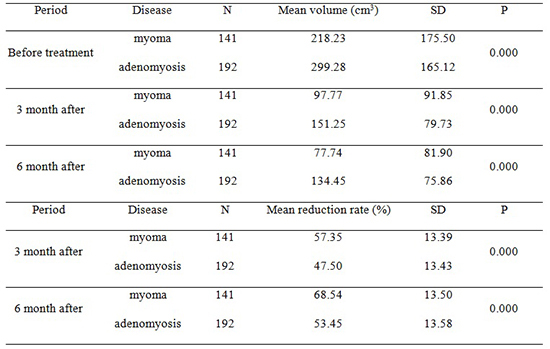
10. Lee JS, Hong GY, Park BJ, Kim TE. Ultrasound-guided high-intensity focused ultrasound treatment for uterine fibroid & adenomyosis: a single center experience from the Republic of Korea. Ultrason Sonochem. 2015; 27:682–687.
11. Ren XL, Zhou XD, Yan RL, Liu D, Zhang J, He GB, Han ZH, Zheng MJ, Yu M. Sonographically guided extracorporeal ablation of uterine fibroids with high-intensity focused ultrasound: midterm results. J Ultrasound Med. 2009; 28:100–103.
12. Wu F, Wang ZB, Chen WZ, Zou JZ, Bai J, Zhu H, Li KQ, Xie FL, Jin CB, Su HB, et al. Extracorporeal focused ultrasound surgery for treatment of human solid carcinomas: early Chinese clinical experience. Ultrasound Med Biol. 2004; 30:245–260.
13. Qin J, Chen JY, Zhao WP, Hu L, Chen WZ, Wang ZB. Outcome of unintended pregnancy after ultrasound-guided high-intensity focused ultrasound ablation of uterine fibroids. Int J Gynaecol Obstet. 2012; 117:273–277.
14. Bohlmann MK, Hoellen F, Hunold P, David M. High-intensity focused ultrasound ablation of uterine fibroids - potential impact on fertility and pregnancy outcome. Geburtshilfe Frauenheilkd. 2014; 74:139–145.
15. Fukunishi H, Funaki K, Sawada K, Yamaguchi K, Maeda T, Kaji Y. Early results of magnetic resonance-guided focused ultrasound surgery of adenomyosis: analysis of 20 cases. J Minim Invasive Gynecol. 2008; 15:571–579.








 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download