1. Al-Ghazal SK, Sully L, Fallowfield L, Blamey RW. The psychological impact of immediate rather than delayed breast reconstruction. Eur J Surg Oncol. 2000; 26:17–19.
2. Kronowitz SJ, Robb GL. Radiation therapy and breast reconstruction: a critical review of the literature. Plast Reconstr Surg. 2009; 124:395–408.
3. Whitfield GA, Horan G, Irwin MS, Malata CM, Wishart GC, Wilson CB. Incidence of severe capsular contracture following implant-based immediate breast reconstruction with or without postoperative chest wall radiotherapy using 40 gray in 15 fractions. Radiother Oncol. 2009; 90:141–147.
4. Rosato RM, Dowden RV. Radiation therapy as a cause of capsular contracture. Ann Plast Surg. 1994; 32:342–345.
5. Spano A, Palmieri B, Taidelli TP, Nava MB. Reduction of capsular thickness around silicone breast implants by zafirlukast in rats. Eur Surg Res. 2008; 41:8–14.
6. Grella E, Grella R, Siniscalco D, Fuccio C, Rossi F, De Novellis V, Maione S, D'Andrea F. Modification of cysteinyl leukotriene receptors expression in capsular contracture: follow-up study and definitive results. Ann Plast Surg. 2009; 63:206–208.
7. Kuhn A, Singh S, Smith PD, Ko F, Falcone R, Lyle WG, Maggi SP, Wells KE, Robson MC. Periprosthetic breast capsules contain the fibrogenic cytokines TGF-beta1 and TGF-beta2, suggesting possible new treatment approaches. Ann Plast Surg. 2000; 44:387–391.
8. Katzel EB, Koltz PF, Tierney R, Williams JP, Awad HA, O'keefe RJ, Langstein HN. The impact of Smad3 loss of function on TGF-β signaling and radiation-induced capsular contracture. Plast Reconstr Surg. 2011; 127:2263–2269.
9. Watts KL, Sampson EM, Schultz GS, Spiteri MA. Simvastatin inhibits growth factor expression and modulates profibrogenic markers in lung fibroblasts. Am J Respir Cell Mol Biol. 2005; 32:290–300.
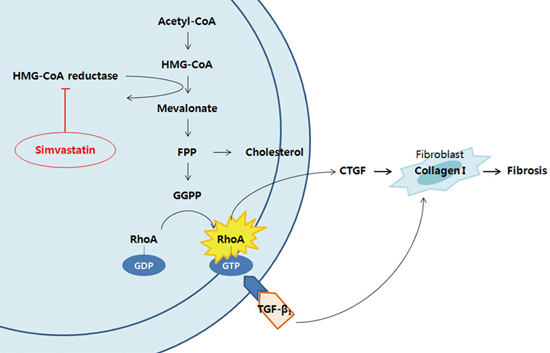
10. Rupérez M, Rodrigues-Díez R, Blanco-Colio LM, Sánchez-López E, Rodríguez-Vita J, Esteban V, Carvajal G, Plaza JJ, Egido J, Ruiz-Ortega M. HMG-CoA reductase inhibitors decrease angiotensin II-induced vascular fibrosis: role of RhoA/ROCK and MAPK pathways. Hypertension. 2007; 50:377–383.
11. O'Brien MJ, Keating NM, Elderiny S, Cerda S, Keaveny AP, Afdhal NH, Nunes DP. An assessment of digital image analysis to measure fibrosis in liver biopsy specimens of patients with chronic hepatitis C. Am J Clin Pathol. 2000; 114:712–718.
12. Fischer S, Hirche C, Reichenberger MA, Kiefer J, Diehm Y, Mukundan S Jr, Alhefzi M, Bueno EM, Kneser U, Pomahac B. Silicone implants with smooth surfaces induce thinner but denser fibrotic capsules compared to those with textured surfaces in a rodent model. PLoS One. 2015; 10:e0132131.
13. Kwak B, Mulhaupt F, Myit S, Mach F. Statins as a newly recognized type of immunomodulator. Nat Med. 2000; 6:1399–1402.
14. Weitz-Schmidt G. Statins as anti-inflammatory agents. Trends Pharmacol Sci. 2002; 23:482–487.
15. Branton MH, Kopp JB. TGF-beta and fibrosis. Microbes Infect. 1999; 1:1349–1365.
16. Rubin P, Johnston CJ, Williams JP, McDonald S, Finkelstein JN. A perpetual cascade of cytokines postirradiation leads to pulmonary fibrosis. Int J Radiat Oncol Biol Phys. 1995; 33:99–109.
17. Martin M, Lefaix J, Delanian S. TGF-beta1 and radiation fibrosis: a master switch and a specific therapeutic target? Int J Radiat Oncol Biol Phys. 2000; 47:277–290.
18. Katzel EB, Koltz PF, Tierney R, Williams JP, Awad HA, O'Keefe RJ, Langstein HN. A novel animal model for studying silicone gel-related capsular contracture. Plast Reconstr Surg. 2010; 126:1483–1491.
19. Mazaheri MK, Schultz GS, Blalock TD, Caffee HH, Chin GA. Role of connective tissue growth factor in breast implant elastomer capsular formation. Ann Plast Surg. 2003; 50:263–268.
20. Hayashi N, Kakimuma T, Soma Y, Grotendorst GR, Tamaki K, Harada M, Igarashi A. Connective tissue growth factor is directly related to liver fibrosis. Hepatogastroenterology. 2002; 49:133–135.
21. Chen S, Crawford M, Day RM, Briones VR, Leader JE, Jose PA, Lechleider RJ. RhoA modulates smad signaling during transforming growth factor-beta-induced smooth muscle differentiation. J Biol Chem. 2006; 281:1765–1770.
22. Law M, Rudnicka AR. Statin safety: a systematic review. Am J Cardiol. 2006; 97:52C–60C.
23. Preiss D, Seshasai SR, Welsh P, Murphy SA, Ho JE, Waters DD, DeMicco DA, Barter P, Cannon CP, Sabatine MS, et al. Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis. JAMA. 2011; 305:2556–2564.
24. Pedersen TR, Berg K, Cook TJ, Faergeman O, Haghfelt T, Kjekshus J, Miettinen T, Musliner TA, Olsson AG, Pyörälä K, et al. Safety and tolerability of cholesterol lowering with simvastatin during 5 years in the Scandinavian Simvastatin Survival Study. Arch Intern Med. 1996; 156:2085–2092.
25. Goldkind L, Laine L. A systematic review of NSAIDs withdrawn from the market due to hepatotoxicity: lessons learned from the bromfenac experience. Pharmacoepidemiol Drug Saf. 2006; 15:213–220.
26. Chitturi S, George J. Hepatotoxicity of commonly used drugs: nonsteroidal anti-inflammatory drugs, antihypertensives, antidiabetic agents, anticonvulsants, lipid-lowering agents, psychotropic drugs. Semin Liver Dis. 2002; 22:169–184.
27. Ou XM, Feng YL, Wen FQ, Huang XY, Xiao J, Wang K, Wang T. Simvastatin attenuates bleomycin-induced pulmonary fibrosis in mice. Chin Med J (Engl). 2008; 121:1821–1829.
28. Hsieh CH, Sun CK, Lu TH, Chen YC, Lin CJ, Wu CJ, Rau CS, Jeng SF. Simvastatin induces heme oxygenase-1 expression but fails to reduce inflammation in the capsule surrounding a silicone shell implant in rats. J Surg Res. 2011; 168:272–280.