1. Caroli A, Manini S, Antiga L, Passera K, Ene-Iordache B, Rota S, Remuzzi G, Bode A, Leermakers J, van de Vosse FN, et al. Validation of a patient-specific hemodynamic computational model for surgical planning of vascular access in hemodialysis patients. Kidney Int. 2013; 84:1237–1245.
2. Sidawy AN, Spergel LM, Besarab A, Allon M, Jennings WC, Padberg FT Jr, Murad MH, Montori VM, O'Hare AM, Calligaro KD, et al. The Society for Vascular Surgery: clinical practice guidelines for the surgical placement and maintenance of arteriovenous hemodialysis access. J Vasc Surg. 2008; 48:2S–25S.
3. Long B, Brichart N, Lermusiaux P, Turmel-Rodrigues L, Artru B, Boutin JM, Pengloan J, Bertrand P, Bruyère F. Management of perianastomotic stenosis of direct wrist autogenous radial-cephalic arteriovenous accesses for dialysis. J Vasc Surg. 2011; 53:108–114.
4. Rooijens PP, Tordoir JH, Stijnen T, Burgmans JP. Smet de AA, Yo TI. Radiocephalic wrist arteriovenous fistula for hemodialysis: meta-analysis indicates a high primary failure rate. Eur J Vasc Endovasc Surg. 2004; 28:583–589.
5. Roy-Chaudhury P, Sukhatme VP, Cheung AK. Hemodialysis vascular access dysfunction: a cellular and molecular viewpoint. J Am Soc Nephrol. 2006; 17:1112–1127.
6. Clark EG, Barsuk JH. Temporary hemodialysis catheters: recent advances. Kidney Int. 2014; 86:888–895.
7. Benedetto B, Lipkowitz G, Madden R, Kurbanov A, Hull D, Miller M, Bow L. Use of cryopreserved cadaveric vein allograft for hemodialysis access precludes kidney transplantation because of allosensitization. J Vasc Surg. 2001; 34:139–142.
8. Kim HO, Kim J, Jin HL. Evaluation of domestic cryostorage blood bags. Korean J Blood Transfus. 2006; 17:48–53.
9. Pegg DE, Wusteman MC, Boylan S. Fractures in cryopreserved elastic arteries. Cryobiology. 1997; 34:183–192.
10. Lee T, Barker J, Allon M. Comparison of survival of upper arm arteriovenous fistulas and grafts after failed forearm fistula. J Am Soc Nephrol. 2007; 18:1936–1941.
11. Asif A, Cherla G, Merrill D, Cipleu CD, Briones P, Pennell P. Conversion of tunneled hemodialysis catheter-consigned patients to arteriovenous fistula. Kidney Int. 2005; 67:2399–2406.
12. Szilagyi DE, McDonald RT, Smith RF, Whitcomb JG, Whitcomb JG. Biologic fate of human arterial homografts. AMA Arch Surg. 1957; 75:506–527.
13. Allaire E, Guettier C, Bruneval P, Plissonnier D, Michel JB. Cell-free arterial grafts: morphologic characteristics of aortic isografts, allografts, and xenografts in rats. J Vasc Surg. 1994; 19:446–456.
14. Schmitz-Rixen T, Megerman J, Colvin RB, Williams AM, Abbott WM. Immunosuppressive treatment of aortic allografts. J Vasc Surg. 1988; 7:82–92.
15. Bia D, Pessana F, Armentano R, Pérez H, Graf S, Zócalo Y, Saldías M, Perez N, Alvarez O, Silva W, et al. Cryopreservation procedure does not modify human carotid homografts mechanical properties: an isobaric and dynamic analysis. Cell Tissue Bank. 2006; 7:183–194.
16. Kieffer E, Gomes D, Chiche L, Fléron MH, Koskas F, Bahnini A. Allograft replacement for infrarenal aortic graft infection: early and late results in 179 patients. J Vasc Surg. 2004; 39:1009–1017.
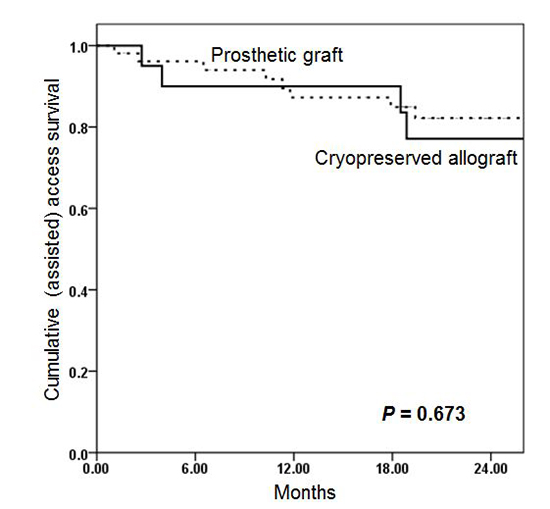
17. Madden RL, Lipkowitz GS, Browne BJ, Kurbanov A. A comparison of cryopreserved vein allografts and prosthetic grafts for hemodialysis access. Ann Vasc Surg. 2005; 19:686–691.
18. Kakkos SK, Andrzejewski T, Haddad JA, Haddad GK, Reddy DJ, Nypaver TJ, Scully MM, Schmid DL. Equivalent secondary patency rates of upper extremity Vectra Vascular Access Grafts and transposed brachial-basilic fistulas with aggressive access surveillance and endovascular treatment. J Vasc Surg. 2008; 47:407–414.
19. Walker PJ, Mitchell RS, McFadden PM, James DR, Mehigan JT. Early experience with cryopreserved saphenous vein allografts as a conduit for complex limb-salvage procedures. J Vasc Surg. 1993; 18:561–569.
20. Zehr BP, Niblick CJ, Downey H, Ladowski JS. Limb salvage with CryoVein cadaver saphenous vein allografts used for peripheral arterial bypass: role of blood compatibility. Ann Vasc Surg. 2011; 25:177–181.






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download