Abstract
Figures and Tables
Fig. 1
Change in the relationships among family members after the patient's suicide attempt. Note that the relationships among families improved in Group A, while they deteriorated in Group B, P=0.007.
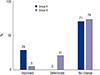
Fig. 2
Proportion of families that were aware of a lack of familial preventative action. The proportion of families that were aware of the lack of preventative action was greater in Group A (24 out of 31) than in Group B (8 of 19), P=0.013.
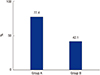
Fig. 3
The person who paid the hospital expenses. In Group A, the parents and/or children were most often responsible for bearing the patient's medical costs, while in Group B, it was often the patients themselves or their spouses (P<0.016).

Table 1
Comparison between Groups A and B in terms of demographics, income, amount of pesticide or drug ingested, time lag after ingestion, APACHE II score, and number of days spent in hospital
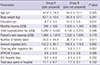
Table 2
Survey items

Notes
This work was carried out with the support of the "Cooperative Research Program for Agriculture Science & Technology Development (Project No. PJ01083201)" Rural Development Administration, Republic of Korea.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download