1. Wolff M, Bower DJ, Marbella AM, Casanova JE. US family physicians' experiences with practice guidelines. Fam Med. 1998; 30:117–121.
2. Davis DA, Taylor-Vaisey A. Translating guidelines into practice: a systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. CMAJ. 1997; 157:408–416.
3. Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ. 2008; 337:a1714.
4. Oh MK, Jo H, Lee YK. Improving the reliability of clinical practice guideline appraisals: effects of the Korean AGREE II scoring guide. J Korean Med Sci. 2014; 29:771–775.
5. Jo MW, Lee JY, Kim NS, Kim SY, Sheen S, Kim SH, Lee SI. Assessment of the quality of clinical practice guidelines in Korea using the AGREE instrument. J Korean Med Sci. 2013; 28:357–365.
6. Lee YK, Shin ES, Shim JY, Min KJ, Kim JM, Lee SH. Executive Committee for CPGs. Korean Academy of Medical Sciences. Developing a scoring guide for the Appraisal of Guidelines for Research and Evaluation II instrument in Korea: a modified Delphi consensus process. J Korean Med Sci. 2013; 28:190–194.
7. Kim YK, Lee SH, Seo JH, Kim JH, Kim SD, Kim GK. A comprehensive model of factors affecting adoption of clinical practice guidelines in Korea. J Korean Med Sci. 2010; 25:1568–1573.
8. Flores G, Lee M, Bauchner H, Kastner B. Pediatricians' attitudes, beliefs, and practices regarding clinical practice guidelines: a national survey. Pediatrics. 2000; 105:496–501.
9. Gagliardi AR, Brouwers MC, Bhattacharyya OK. The guideline implementability research and application network (GIRAnet): an international collaborative to support knowledge exchange: study protocol. Implement Sci. 2012; 7:26.
10. Cranney M, Warren E, Barton S, Gardner K, Walley T. Why do GPs not implement evidence-based guidelines? A descriptive study. Fam Pract. 2001; 18:359–363.
11. McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. N Engl J Med. 2003; 348:2635–2645.
12. Kim N, Kim S, Eunja P. Promoting the quality of medicine: based on clinical practice guidelines. Seoul: Korea Institute for Health and Social Affairs;2004.
13. Yang J, Han C, Yoon HK, Pae CU, Kim MJ, Park SY, Ahn J. Experiences and barriers to implementation of clinical practice guideline for depression in Korea. BMC Psychiatry. 2013; 13:150.
14. Shiffman RN, Dixon J, Brandt C, Essaihi A, Hsiao A, Michel G, O'Connell R. The GuideLine Implementability Appraisal (GLIA): development of an instrument to identify obstacles to guideline implementation. BMC Med Inform Decis Mak. 2005; 5:23.
15. Korean Association of Urogenital Tract Infection and Inflammation (KR). Sexually transmitted infections-Korean guidelines. 2011. accessed on 20 November 2014. Available at
http://www.uti.or.kr/file/2011051601.pdf.
16. Christl B, Lloyd J, Krastev Y, Litt J, Harris MF. Preventing vascular disease - effective strategies for implementing guidelines in general practice. Aust Fam Physician. 2011; 40:825–828.
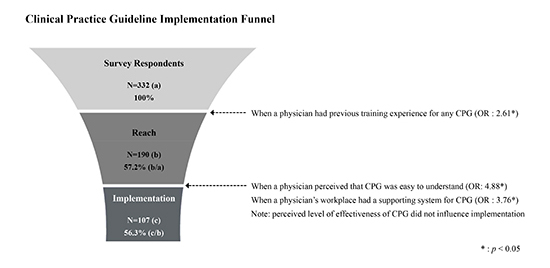
17. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999; 89:1322–1327.
18. Carlfjord S, Andersson A, Bendtsen P, Nilsen P, Lindberg M. Applying the RE-AIM framework to evaluate two implementation strategies used to introduce a tool for lifestyle intervention in Swedish primary health care. Health Promot Int. 2012; 27:167–176.
19. Farris RP, Will JC, Khavjou O, Finkelstein EA. Beyond effectiveness: evaluating the public health impact of the WISEWOMAN program. Am J Public Health. 2007; 97:641–647.
20. Reach Effectiveness Adoption Implementation Maintenance (RE-AIM). Blacksburg (VI): Virginia Tech, College of Agriculture and Life Sciences, Department of Human Nutrition, Foods and Exercise;accessed on 20 November 2014. Available at
http://www.re-aim.org.
21. Grilli R, Lomas J. Evaluating the message: the relationship between compliance rate and the subject of a practice guideline. Med Care. 1994; 32:202–213.
22. Jeong HJ, Pham JC, Kim M, Engineer C, Pronovost PJ. Major cultural-compatibility complex: considerations on cross-cultural dissemination of patient safety programmes. BMJ Qual Saf. 2012; 21:612–615.
23. Kotler P, Rackham N, Krishnaswamy S. Ending the war between Sales & Marketing. Harv Bus Rev. 2006; 84:68–78. 187
24. Patterson L. Marketing and sales alignment for improved effectiveness. J Digit Asset Manag. 2007; 3:185–189.
25. West R. Time for a change: putting the Transtheoretical (Stages of Change) Model to rest. Addiction. 2005; 100:1036–1039.
26. Banait G, Sibbald B, Thompson D, Summerton C, Hann M, Talbot S. Salford and Trafford Ulcer Research Network. Modifying dyspepsia management in primary care: a cluster randomised controlled trial of educational outreach compared with passive guideline dissemination. Br J Gen Pract. 2003; 53:94–100.
27. Francke AL, Smit MC, de Veer AJ, Mistiaen P. Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC Med Inform Decis Mak. 2008; 8:38.
28. Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005; 330:765.
29. Haagen EC, Nelen WL, Hermens RP, Braat DD, Grol RP, Kremer JA. Barriers to physician adherence to a subfertility guideline. Hum Reprod. 2005; 20:3301–3306.
30. Gordis L. Epidemiology. 3rd ed. Philadelphia, PA: Elsevier Saunders;2004.
31. Jeong HJ, Kim M. A practical guide to behavioral theory-driven statistical development of quality and safety improvement program in health care. Biom Biostat Int J. 2014; 1:00001. DOI:
10.15406/bbij.2014.01.00001.
32. Jeong HJ, Jo HS, Jung SM, Lee JY. Factors related to condom use behavior among club-working women in South Korea: importance of subjective norms and customer-related attitudes. Asia Pac J Public Health. 2014; 26:147–159.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download