Abstract
The conventional laparoscopic approach to rectal surgery has several limitations, and therefore many colorectal surgeons have great expectations for the robotic surgical system as an alternative modality in overcoming challenges of laparoscopic surgery and thus enhancing oncologic and functional outcomes. This review explores the possibility of robotic surgery as an alternative approach in laparoscopic surgery for rectal cancer. The da Vinci® Surgical System was developed specifically to compensate for the technical limitations of laparoscopic instruments in rectal surgery. The robotic rectal surgery is associated with comparable or better oncologic and pathologic outcomes, as well as low morbidity and mortality. The robotic surgery is generally easier to learn than laparoscopic surgery, improving the probability of autonomic nerve preservation and genitourinary function recovery. Furthermore, in very complex procedures such as intersphincteric dissections and transabdominal transections of the levator muscle, the robotic approach is associated with increased performance and safety compared to laparoscopic surgery. The robotic surgery for rectal cancer is an advanced technique that may resolve the issues associated with laparoscopic surgery. However, high cost of robotic surgery must be addressed before it can become the new standard treatment.
Rectal cancer surgery can be a very difficult procedure and involves attempting to radically excise the cancer without damaging the surrounding tissue. For this reason, functional and oncologic outcomes are not always favorable. However, after development of total mesorectal excision (TME), functional outcomes and the rate of local recurrences have improved remarkably (1).
Neoadjuvant chemoradiation therapy for rectal cancer increases resectability, allowing for performance of sphincter-saving curative resections, decreasing the locoregional recurrence rate, and improving survival rate. This modality has become common in most countries, according to National Comprehensive Cancer Network (NCCN) guideline (2, 3, 4).
Several randomized controlled trials and reviews confirmed that laparoscopic colorectal resection results in improved early postoperative outcomes including reduction in intraoperative blood loss, postoperative pain, ileus and duration of hospital stay (5). Large randomized trials such as the CLASICC trial and the COREAN trial found minimally invasive approaches to be feasible and oncologically safe (6, 7). However, some randomized trials that evaluated long-term clinical outcomes of rectal cancer did not observe an increase in overall survival or in disease-free survival in patients who underwent laparoscopic-assisted treatment (8, 9, 10). In addition, a previous study suggested that laparoscopic-assisted rectal surgery should not be used routinely because circumferential resection margin (CRM) positivity was higher in the laparoscopic group than in the open surgery group (6).
Unplanned intraoperative conversions from laparoscopic to open surgery indicate issues with the safety and feasibility of laparoscopic methods (6, 11). However, in Asian countries, many surgeons showed the conversion rate less than 5%. Kim et al. (12) reported that only two of 170 patients (1.2%) who underwent laparoscopic surgery were converted to open surgery. However, those results have some limitations because the laparoscopic surgery was performed by highly skilled laparoscopic specialists, and the study was performed in patients with limited oncologic risk due to the exclusion of cT4 lesions and focus on patients with a relatively low BMI. Kwak et al. (13) reported that two of 59 laparoscopic surgeries for rectal cancer were converted to open surgery (2/59, 3.4%). Even though the conversion rate was relatively low, they acknowledged that laparoscopic fine pelvic dissection is very difficult and can cause bleeding from the lateral pelvic wall, rectal perforations, and unintended injury to adjacent organs.
Laparoscopic surgery has been used for more than 20 yr in the field of rectal cancer surgery, but there has been no significant improvement in the postoperative complication rate over time. This may be due to the inherently high morbidity associated with rectal surgery or to limitations of current laparoscopic instruments (14). The conventional laparoscopic approach is particularly difficult because it involves unarticulated rigid instruments, an assistant-dependent, unstable, two-dimensional view, and poor ergonomics. In addition, surgical outcomes can be negatively impacted if the surgeon performing the surgery experiences tremors or is unable to perform high-precision suturing. These limitations are particularly remarkable during rectal dissection in the pelvis as they result in poor nerve visualization, traction injury, rectal cross stapling, difficult retraction, and crowding of the instruments. Because the pelvis is a relatively confined space, the operative view can be obscured by condensation, which often results in fogging of the camera that can slow the progress of an already technically-demanding procedure (5).
Since the first prospective randomized trial comparing robotic low anterior resection and laparoscopic low anterior resection was launched by Baik et al. in 2006, several meta-analyses have been published on this technique, indicating a marked interest in robotic surgery for rectal cancer. The studies demonstrated the feasibility and safety of robotic low anterior resection and reported a better mesorectal grade in the robotic low anterior resection group (15, 16, 17).
This review aims to explore the possibility of robotic surgery as a new standard treatment to overcome challenges associated with laparoscopic surgery for rectal cancer.
A literature search of electronic databases was performed using the terms 'robot,' 'laparoscopic,' 'rectal surgery,' 'colonic surgery,' 'total mesorectal excision' and 'proctectomy.' Reference lists from papers identified in the first literature search were then reviewed for additional articles. Original articles, review articles and two case reports were included; all articles were published in English. Data from these studies are critically analyzed and summarized in this paper.
There is some concern about the higher rate of circumferential resection margin (CRM) involvement among rectal cancer patients undergoing low anterior resection with laparoscopic surgery (12.4%) compared to that of open surgery (6.3%) in the CLASICC trial. In addition, the rectal laparoscopic subgroup had a higher conversion rate than the colon laparoscopic subgroup (34% vs. 25%). Furthermore, in the CLASICC trial, mortality and morbidity rates were highest in colon and rectal cancer patients who were converted from laparoscopic to open surgery. Patients who underwent conversion had a higher mortality rate than open or laparoscopic patients (9% vs. 5% and 1%, respectively, P=0.34). The complication rate was also higher in converted patients compared to non-converted patients and patients who underwent open surgery (P=0.002). This suggests that there are still technical issues that need to be addressed for the use of the laparoscopic approach for rectal cancer (6, 18). In addition, the COLOR II trial reported non-inferior oncological outcomes but a high conversion rate (17%) in patients undergoing laparoscopic rectal surgery, although the conversion rate was decreased compared with previous studies. The study was a large multicentric randomized trial, but it was performed in selected patients treated by skilled surgeons (11).
The da Vinci® Surgical System was developed specifically to compensate for the technical limitations of laparoscopic instruments. The system provides an ergonomic position, elimination of physiologic tremors, improved dexterity, seven degrees of freedom, motion scaling, stable camera, platform and stereoscopic views, and three-dimensional imaging (19). TME is the secure dissection of an avascular plane between the Waldeyer fascia and fascia propria or Denonvillier fascia and fascia propria without injuring the proper fascia of the rectum. Thus, the da Vinci surgical system is an excellent tool for performing TME in rectal cancer patients (20).
However, the da Vinci system has some technical drawbacks. First, there is a lack of tactile sensation and tensile feedback to the surgeon. Consequently, tissue damage can occur easily during traction by the robotic arm and during movement of the robotic instrument. Moreover, suture material may be cut because there is no tensile feedback during suturing. Nevertheless, these technical disadvantages can be overcome by visual feedback, assuming the surgeon has sufficient experience (16).
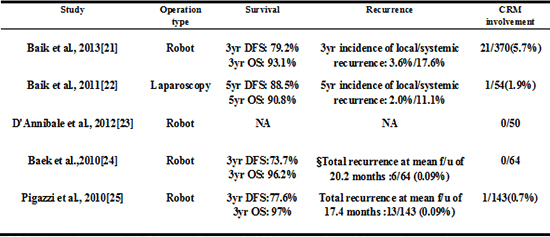
In several non-randomized studies using participants from a single health center in Korea, robotic surgery for rectal cancer is associated with better oncologic outcomes. Baik et al. (21) reported that the three-year overall survival and three-year disease-free survival rates in patients who underwent robotic rectal surgery were 93.1% and 79.2%, respectively. In the present study, the CRM involvement rate, which represents a negative impact on oncologic outcomes, was 5.7%, and the three-year cumulative incidence of local recurrence was 3.6%. These results are similar to previous studies that evaluated the oncologic outcomes of conventional laparoscopic surgery for rectal cancer (22). Besides, there are some studies showing totally negative circumferential resection margin which lead to favorable oncologic outcomes. The authors in these studies claim that the negative resection margin rate may reflect better visualization and ergonomics with robotic technology (23, 24). In a multicentric study of robotic TME by Pigazzi et al. (25), remarkable short-term clinical outcomes were identified. The three-year overall survival rate was 97% in 143 consecutive patients with rectal cancer who underwent robotic surgery, and no isolated local recurrence was found during the mean follow-up period of 17.4 months. This study did not have a control group, had a relatively short follow-up period, and involved the extensive use of neoadjuvant chemoradiation. However, the results indicate that robotic surgery improves survival rate and patient quality of life (Table 1).
We briefly describe the procedure of totally robotic rectal surgery with a single-docking technique as performed in our institution. Totally robotic rectal surgeries using the da Vinci Surgical System consist of two phases: the lateral phase and the pelvic phase. During all processes, the robotic surgical cart is fixed, and the patient's position does not change. The robotic surgical cart is located at the left caudal side of the surgical table. An assistant stands at the patient's right side in order to avoid mirror imaging during the operation. We used a six-port system including a camera port to perform rectal cancer surgery from the splenic flexure to the pelvic diaphragm without any change in the initial setup. Of the five working ports, one is used for dissection, another is used for traction and a third is used for the surgeon's non-dominant hand. The remaining ports are used for the assistant's hand or application of the endolinear stapler at the end of the pelvic phase (Fig. 1).
The procedure during the lateral phase includes medial to lateral dissection from the sacral promontory to the splenic flexure along the avascular plane, dissection of tissue-bearing lymph nodes around the root of the inferior mesenteric artery, ligation and division of the inferior mesenteric artery, and splenic flexure mobilization if needed. Procedures during the pelvic phase include dissection of the pelvic cavity along the plane between the mesorectal fascia proper and the parietal pelvic fascia preserving the pelvic autonomic nerve plexus, division of the mesorectum if needed, and division of the rectum with the endolinear stapler. Finally, anastomosis is performed laparoscopically or under direct vision after removal of the specimen through the Pfannelstiel skin incision made by extension of the port site (26).
Stefanidis et al. (27) showed that robotic assistance led to improved suturing performance by novice surgeons, limited the number of inadvertent injuries to structures outside the operating field, and decreased operator workload in a live animal model. They also showed a shorter learning curve for intracorporeal suturing with robotic assistance compared with laparoscopy. Suturing and knot-tying with robotic assistance were easier as evidenced by the higher participant performance scores, improved ability to complete the task within the allowed time, and rapid improvement in score from the first to third attempt. Another study comparing robotic suture technique to laparoscopic suture techniq ue showed that the advantage about intracorporeal suturing in robot was presented not only in novice group but also in expert group. This result means that robotic device is feasible regardless of amount of laparoscopic experience (28). The intracorporeal suture technique could allow for greater technical performance and accuracy in delicate operative fields. During an operation, surgeons sometime encounter unwanted events, such as bowel injury and bleeding, and robotic suturing could help surgeons to resolve these difficult situations, especially in narrow spaces. Additionally, the improved performance and accuracy afforded by robotic instruments allows surgeons to get closer to a natural orifice transluminal endoscopic surgery. Previously, Park et al. reported on the usefulness of a hybrid technique that eliminated the need for mini-laparotomy for removal a specimen through the anus or vagina after complete intracorporeal resection and anastomosis in the rectal cancer using robotic intracorporeal suture (29, 30). This study showed not only how easy a surgeon manipulated the robotic devices but also how accurate movement of the robotic device was during an operation.
A meta-analysis undertaken by Memon et al. (31) included seven refined review articles and analyzed a total of 353 robot-assisted laparoscopic proctectomies and 401 conventional laparoscopic proctectomies. The overall conversion rate was higher for laparoscopic surgery compared to robotic surgery in all studies (total risk difference:-0.07 (95%CI, -0.12 ~ -0.01), Heterogeneity, I2=80%, P=0.03), and overall operation time was not significantly different (total risk difference, 2.96 [95%CI, -0.12 ~ -0.01], Heterogeneity, I2=95%, P=0.19). Scarpinata et al. (32) reported that the conversion rate in robotic rectal surgery (1% to 7.3%) was lower than in laparoscopic rectal surgery (3% to 22%), and the author claimed that the robotic approach was more optimal in difficult cases such as previous abdominal surgery, lower rectal cancers, lower rectal cancers and previous chemoradiation therapy.
Baek et al. (33) performed a retrospective study comparing short-term and long-term outcomes between robotic and laparoscopic ultralow anterior resection with or without coloanal anastomosis. They showed that robotic surgery is a safe and feasible approach with a lower conversion rate, a shorter hospital stay and similar oncologic outcomes compared with laparoscopic surgery. As previously mentioned, conversions have been associated suboptimal outcomes in terms of morbidity and mortality. Therefore, a relatively low conversion rate in robotic rectal surgery may indicate favorable long-term clinical outcomes.
In a study analyzed a learning curve in laparoscopic surgery using the moving average method for operative time, they showed that the surgeon typically became proficient in laparoscopic low anterior resection for rectal cancer after 50 cases. This was similar to previous studies, in which the learning curve for laparoscopic colectomy ranged from 30 to 70 cases (34).
In some studies focused on the learning curve for robotic rectal surgery, operative time and console time decreased remarkably after about 20 cases. The three-dimensional view and the ability of the robot to transfer the surgeon's hand movements to the tips of the surgical instruments might greatly decrease the learning curve of robotic surgery compared to that of laparoscopic colorectal surgery. In addition, the technical advantages described above enable inexperienced laparoscopic surgeons to operate the robot safely and easily (5, 35, 36, 37). However, recent studies of a large number of patients, in which multiple methods for evaluating learning curves were analyzed, have shown different results. The studies used not only operative time but also surgical outcomes related to risk factors as a tool for evaluating learning curves. Among the results of a multidimensional analysis, studies have shown that there is multiphasic learning curve and initial learning period up to 32-44 cases (38, 39, 40). In these studies, the reason why the learning curve of robotic rectal surgery is not shorter than conventional laparoscopic surgery, despite easy manipulation of the robotic console, was absence of haptic sensation. If this drawback is overcome, the learning curve is expected to be shortened due to the technical advantages described above. Additionally, the reason why the learning curve consisted of two peaks and three phases was that technical competence to reduce an operative time was achieved in the initial phase. Surgical completion to overcome difficult cases, such as lower tumor location and obese patients, or to reduce surgical failure was achieved in the second phase. Hereafter, a comparative analysis of learning curves between robot and laparoscopy using a multidimensional analytic method is necessary to demonstrate the advantages of robotic techniques.
Some studies have raised the concern that laparoscopic mesorectal excisions may be associated with urinary and sexual dysfunction, which is not typically an issue in conventional open surgery. Sexual function and behavior after laparoscopic total mesorectal excision were remarkably reduced compared to those before the operation or after open surgery (41, 42, 43).
Three studies evaluating genitourinary function after robotic rectal surgery reported that postoperative sexual dysfunction improved one month after surgery and recovered gradually thereafter. Kim et al. reported that the robotic group showed earlier functional recovery than the laparoscopic group (Fig. 2), and D'Annibale et al. reported that erectile function was restored completely in the robotic group and partially restored in the laparoscopic group. All of the authors agreed that it was easier to identify the nerves and the planes of dissection using the robotic system (Fig. 3) (23, 44, 45).
Studies about lateral pelvic side-wall recurrence in advanced rectal cancer advocate that lateral pelvic lymph node dissection should be performed, because the overall incidence of metastasis to lateral pelvic lymph nodes ranges from 8.6 to 27%. This result associates with positive nodes which are not cleared in patients who undergo TME only (46, 47, 48). One recent study suggested that lateral pelvic side wall recurrence is a major cause of locoregional recurrence in patients treated with neoadjuvant chemoradiotherapy followed by TME (49). However, lateral pelvic lymph node dissection, in itself, can increase blood loss, urinary and sexual dysfunction, and longer operation times without survival benefits (47, 50, 51). Nonetheless, surgeons have demonstrated the feasibility and safety of a robotic approach for pelvic lymph node dissection for radical surgery, although these reports are outside the field of colorectal surgery (52, 53). If precise lymphovascular dissection with advanced robotic techniques applies to locally advanced rectal cancer requiring pelvic lymph node dissection, then radical surgery can be performed more safely and more easily.
Intersphincteric dissection is one of the hardest forms of rectal surgical procedures. The procedure is associated with favorable long-term oncological and functional outcomes (54, 55). The technical advantages of robotic surgery, including accurate dissection and clear visibility, are particularly useful qualities during pelvic dissection, especially because the cul de sac is very confined, and the pelvic structures adjacent to the rectum are easily injured (56). In addition, the robotic approach helps improve intersphincteric dissection, which in turns decreases the duration of the perineal procedure. As a result, robotic intersphincteric dissection has led to several improved functional outcomes (57). Further prospective randomized trials are needed to clarify the findings of recent studies about robotic intersphincteric dissection.
One study suggested new criteria to preserve the sphincter in ultra-low rectal cancer at the levator muscle level. Technically, the procedure is challenging, but with the endo-wrist advantage of the robotic system, the abdominal phase becomes easier. Also, perineal phase dissection can be simplified via an approach to the levator ani from the abdominal phase and division at its origin. This method allows a preferred shallow shape of the levator ani plate, complicating the perineal phase due to the high location of the levator origin. This procedure preserving anus can be safe and feasible in the cases which were down-sized after chemoradiation therapy (Fig. 4). However, long-term functional and oncological outcomes still need to be assessed after loop ileostomy reversal (58).
The lower rectum has a relatively thin mesorectal envelope because the mesorectum cones along the levator muscles end at the level of the puborectalis muscle. Poor visibility and inadequate surgical exposure in the deep pelvis as well as this anatomical coning result in high circumferential margin (CRM) positivity of tumors within 5 cm of the anal verge. Abdominal perineal resection (APR) can lead to higher CRM positivity than low anterior resection because it involves the blind perineal approach phase. CRM positivity is a predictive factor for local recurrence and disease-free survival (59). The extralevator approach to APR is associated with lower CRM positivity and incidence of rectal perforation, and as a result, the rate of local recurrence may decrease. However, approaching the levator muscles through the perineum remains difficult due to the blind approach. This can be overcome using robotic assistance to perform the transabdominal transection of levator muscles under direct visualization (Fig. 5). Marecik et al. (60) reported excellent immediate postoperative and pathological results of robotic abdominoperineal resection with transabdominal levator transection involving wide excision of the levator muscles, even though it was a small study with only five participants. An intact fascia propria and negative circumferential resection margin were achieved in all cases, and all specimens had a cylindrical shape.
Anastomotic leakage is a major life-threatening complication that can lead to frequent reoperations, multiple drainage procedures, and in rare cases, death. There are many factors associated with anastomotic leakage including male gender, level of anastomosis (less than 5 cm), and preoperative radiation (61). Furthermore, perfusion abnormalities and technical factors which is caused by surgeons may become additional adverse factors (62).
Predictive tests for anastomotic leakage include active bleeding from the resection margin, palpable pulsation in the mesentery and lack of discoloration. However, these measures are highly unreliable and fail to accurately predict postoperative leakage. (63). Indocyanine green (ICG) is a sterile, water-soluble, tricarnocyanine compound that absorbs near infrared (NIR) light with a peak spectral absorption at 800 nm. When ICG is injected intravenously, it rapidly and extensively binds to plasma protein and remains intravascular with minimal leakage into the interstitium. ICG fluorescene can be seen by the NIR camera system (64). Jafari et al. (65) showed that determination of resection point by ICG fluorescene during robot-assisted low anterior resection decreased anastomotic leakage. Kudszus et al. (66) used laser fluorescene angiography with ICG and a laser-mounted scope to visualize the tissue perfusion and reported a 60% reduction in reoperation for anastomotic leaks. ICG imaging can also be applied to vessel division and ligation without adjacent tissue injury (67).
Cost is a major drawback of robotic rectal surgery. In a cost-comparison analysis between robotic rectal surgery and laparoscopic rectal surgery, Baek et al. (68) reported that robotic surgery is significantly more expensive than laparoscopic surgery for rectal cancer, with total hospital charges approximately 1.5 times higher in the robotic group compared to the laparoscopic group (13,644 USD vs. 9,065 USD, respectively; P<0.001). Moreover, actual payments by patients were also significantly higher in the robotic group than the laparoscopic group, which the payment was almost three times as much in the robotic group compared to the laparoscopic group (11,540 USD vs. 3,956 USD, respectively; P<0.001), but the total hospital charge and payment were decreasing according to accumulation of cases. In addition, hospital profit was significantly lower in the robotic group (689 USD vs. 1,671 USD respectively; P<0.001) (Fig. 6). However, the authors pointed out that this was not a cost-effectiveness study, but a cost-analysis study.
For the popularization of robotic surgery, first of all, medical insurance cost should be adjusted and then patients sharing of the medical cost should be down. Second, in order to justify the high cost of robotic surgery, it must be shown that robotic surgery is significantly better than other methods in terms of oncologic and functional outcomes, especially in difficult cases such as those involving preoperative chemoradiation therapy, obese patients, patients with a relatively narrow pelvis, or large tumors.
In conclusion, robotic surgery for rectal cancer is a novel technique that has advanced the treatment of rectal cancer. Robotic surgery seems to address most of the shortcomings of laparoscopic surgery and is proven to be safe, easy to learn, and physical less taxing for surgeons. However, the high cost of robotic surgery is a major drawback. Robotic surgery may not become widespread until its obvious superiority over other methods is demonstrated in terms of oncologic and functional outcomes.
Presently, randomized trials to support robotic-assisted surgery for rectal cancer such as the Robotic versus LAparoscopic Resection for Rectal cancer (ROLARR) trial and Comparison of Laparoscopic-Assisted vs. Robot-Assisted surgery for rectal cancer study Group (COLARAR) trial are ongoing to address this issue. We expect that the results from these trials will help establish the robotic approach as the new standard treatment in rectal cancer surgery.
Figures and Tables
 | Fig. 2Changes in IIEF score and IPSS before surgery and several months after surgery. IIEF, international index of erectile function; IPSS, international prostate symptom score; L/R-TME, laparoscopic/robot-assisted total mesorectal excision. Red circle, R-TME allowed for an earlier recovery. Kim (43); Fab (44). |
 | Fig. 3Preservation of autonomic nerve system related to genitourinary function (43). |
 | Fig. 4Multimodality treatment preserving anus: Neoadjuvant chemoradiation therapy and robotic rectal sleeve resection with colo-anal anastomosis (57). |
 | Fig. 5The difference between conventional abdominoperineal resection and extralevator abdominoperineal resection using robotic assistance. |
 | Fig. 6Changes of cost according to accumulation of cases in robotic surgery (67). |
Table 1
Oncologic outcomes of robotic surgery

| Study | Operation type | Survival | Recurrence | CRM involvement |
|---|---|---|---|---|
| Baik et al., 2013 (21) | Robot | 3 yr DFS: 79.2% | 3 yr incidence of local/systemic recurrence: 3.6%/17.6% | 21/370 (5.7%) |
| 3 yr OS: 93.1% | ||||
| Baik et al., 2011 (22) | Laparoscopy | 5 yr DFS: 88.5% | 5 yr incidence of local/systemic recurrence: 2.0%/11.1% | 1/54 (1.9%) |
| 5 yr OS: 90.8% | ||||
| D'Annibale et al., 2012 (23) | Robot | NA | NA | 0/50 |
| Baek et al., 2010 (24) | Robot | 3 yr DFS: 73.7% | *Total recurrence at mean f/u of 20.2 months: 6/64 (0.09%) | 0/64 |
| 3 yr OS: 96.2% | ||||
| Pigazzi et al., 2010 (25) | Robot | 3 yr DFS: 77.6% | Total recurrence at mean f/u of 17.4 months: 13/143 (0.09%) | 1/143 (0.7%) |
| 3 yr OS: 97% |
References
1. Kim NK, Kim MS, Al-Asari SF. Update and debate issues in surgical treatment of middle and low rectal cancer. J Korean Soc Coloproctol. 2012; 28:230–240.
2. Kim NK, Baik SH, Seong JS, Kim H, Roh JK, Lee KY, Sohn SK, Cho CH. Oncologic outcomes after neoadjuvant chemoradiation followed by curative resection with tumor-specific mesorectal excision for fixed locally advanced rectal cancer: Impact of postirradiated pathologic downstaging on local recurrence and survival. Ann Surg. 2006; 244:1024–1030.
3. Engstrom PF, Arnoletti JP, Benson AB 3rd, Chen YJ, Choti MA, Cooper HS, Covey A, Dilawari RA, Early DS, Enzinger PC, et al. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: rectal cancer. J Natl Compr Canc Netw. 2009; 7:838–881.
4. van Gijn W, Marijnen CA, Nagtegaal ID, Kranenbarg EM, Putter H, Wiggers T, Rutten HJ, Påhlman L, Glimelius B, van de Velde CJ, et al. Dutch Colorectal Cancer Group. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol. 2011; 12:575–582.
5. Aly EH. Robotic colorectal surgery: summary of the current evidence. Int J Colorectal Dis. 2014; 29:1–8.
6. Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM. MRC CLASICC trial group. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005; 365:1718–1726.
7. Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW, Lim SB, Lee TG, Kim DY, Kim JS, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol. 2010; 11:637–645.
8. Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004; 350:2050–2059.
9. Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS, Lai PB, Lau WY. Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet. 2004; 363:1187–1192.
10. Milsom JW, Böhm B, Hammerhofer KA, Fazio V, Steiger E, Elson P. A prospective, randomized trial comparing laparoscopic versus conventional techniques in colorectal cancer surgery: a preliminary report. J Am Coll Surg. 1998; 187:46–54. discussion -5.
11. van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC, Bonjer HJ. COlorectal cancer Laparoscopic or Open Resection II (COLOR II) Study Group. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol. 2013; 14:210–218.
12. Kim NK, Kang J. Optimal Total Mesorectal Excision for Rectal Cancer: the Role of Robotic Surgery from an Expert's View. J Korean Soc Coloproctol. 2010; 26:377–387.
13. Kwak JM, Kim SH, Kim J, Son DN, Baek SJ, Cho JS. Robotic vs laparoscopic resection of rectal cancer: short-term outcomes of a case-control study. Dis Colon Rectum. 2011; 54:151–156.
14. Shearer R, Gale M, Aly O, Aly E. Have early postoperative complications from laparoscopic rectal cancer surgery improved over the past 20 years? Colorectal Dis. 2013; 15:1211–1226.
15. Kim SH, Kwak JM. Robotic total mesorectal excision: operative technique and review of the literature. Tech Coloproctol. 2013; 17:S47–S53.
16. Baik SH. Robotic colorectal surgery. Yonsei Med J. 2008; 49:891–896.
17. Bianchi PP, Luca F, Petz W, Valvo M, Cenciarelli S, Zuccaro M, Biffi R. The role of the robotic technique in minimally invasive surgery in rectal cancer. Ecancermedicalscience. 2013; 7:357.
18. Rottoli M, Bona S, Rosati R, Elmore U, Bianchi PP, Spinelli A, Bartolucci C, Montorsi M. Laparoscopic rectal resection for cancer: effects of conversion on short-term outcome and survival. Ann Surg Oncol. 2009; 16:1279–1286.
19. Baik SH, Ko YT, Kang CM, Lee WJ, Kim NK, Sohn SK, Chi HS, Cho CH. Robotic tumor-specific mesorectal excision of rectal cancer: short-term outcome of a pilot randomized trial. Surg Endosc. 2008; 22:1601–1608.
20. Baik SH, Lee WJ, Rha KH, Kim NK, Sohn SK, Chi HS, Cho CH, Lee SK, Cheon JH, Ahn JB, et al. Robotic total mesorectal excision for rectal cancer using four robotic arms. Surg Endosc. 2008; 22:792–797.
21. Baik SH, Kim NK, Lim DR, Hur H, Min BS, Lee KY. Oncologic outcomes and perioperative clinicopathologic results after robot-assisted tumor-specific mesorectal excision for rectal cancer. Ann Surg Oncol. 2013; 20:2625–2632.
22. Baik SH, Gincherman M, Mutch MG, Birnbaum EH, Fleshman JW. Laparoscopic vs open resection for patients with rectal cancer: comparison of perioperative outcomes and long-term survival. Dis Colon Rectum. 2011; 54:6–14.
23. D'Annibale A, Pernazza G, Monsellato I, Pende V, Lucandri G, Mazzocchi P, Alfano G. Total mesorectal excision: a comparison of oncological and functional outcomes between robotic and laparoscopic surgery for rectal cancer. Surg Endosc. 2013; 27:1887–1895.
24. Baek JH, McKenzie S, Garcia-Aguilar J, Pigazzi A. Oncologic outcomes of robotic-assisted total mesorectal excision for the treatment of rectal cancer. Ann Surg. 2010; 251:882–886.
25. Pigazzi A, Luca F, Patriti A, Valvo M, Ceccarelli G, Casciola L, Biffi R, Garcia-Aguilar J, Baek JH. Multicentric study on robotic tumor-specific mesorectal excision for the treatment of rectal cancer. Ann Surg Oncol. 2010; 17:1614–1620.
26. Park YA, Kim JM, Kim SA, Min BS, Kim NK, Sohn SK, Lee KY. Totally robotic surgery for rectal cancer: from splenic flexure to pelvic floor in one setup. Surg Endosc. 2010; 24:715–720.
27. Stefanidis D, Wang F, Korndorffer JR Jr, Dunne JB, Scott DJ. Robotic assistance improves intracorporeal suturing performance and safety in the operating room while decreasing operator workload. Surg Endosc. 2010; 24:377–382.
28. Chandra V, Nehra D, Parent R, Woo R, Reyes R, Hernandez-Boussard T, Dutta S. A comparison of laparoscopic and robotic assisted suturing performance by experts and novices. Surgery. 2010; 147:830–839.
29. Choi GS, Park IJ, Kang BM, Lim KH, Jun SH. A novel approach of robotic-assisted anterior resection with transanal or transvaginal retrieval of the specimen for colorectal cancer. Surg Endosc. 2009; 23:2831–2835.
30. Park JS, Choi GS, Lim KH, Jang YS, Jun SH. S052: a comparison of robot-assisted, laparoscopic, and open surgery in the treatment of rectal cancer. Surg Endosc. 2011; 25:240–248.
31. Memon S, Heriot AG, Murphy DG, Bressel M, Lynch AC. Robotic versus laparoscopic proctectomy for rectal cancer: a meta-analysis. Ann Surg Oncol. 2012; 19:2095–2101.
32. Scarpinata R, Aly EH. Does robotic rectal cancer surgery offer improved early postoperative outcomes? Dis Colon Rectum. 2013; 56:253–262.
33. Baek SJ, Al-Asari S, Jeong DH, Hur H, Min BS, Baik SH, Kim NK. Robotic versus laparoscopic coloanal anastomosis with or without intersphincteric resection for rectal cancer. Surg Endosc. 2013; 27:4157–4163.
34. Kayano H, Okuda J, Tanaka K, Kondo K, Tanigawa N. Evaluation of the learning curve in laparoscopic low anterior resection for rectal cancer. Surg Endosc. 2011; 25:2972–2979.
35. Jiménez-Rodríguez RM, Díaz-Pavón JM, de la Portilla de Juan F, Prendes-Sillero E, Dussort HC, Padillo J. Learning curve for robotic-assisted laparoscopic rectal cancer surgery. Int J Colorectal Dis. 2013; 28:815–821.
36. Kim YW, Lee HM, Kim NK, Min BS, Lee KY. The learning curve for robot-assisted total mesorectal excision for rectal cancer. Surg Laparosc Endosc Percutan Tech. 2012; 22:400–405.
37. Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM. Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc. 2011; 25:855–860.
38. Park EJ, Kim CW, Cho MS, Baik SH, Kim DW, Min BS, Lee KY, Kim NK. Multidimensional analyses of the learning curve of robotic low anterior resection for rectal cancer: 3-phase learning process comparison. Surg Endosc. 2014; 28:2821–2831.
39. Kim HJ, Choi GS, Park JS, Park SY. Multidimensional analysis of the learning curve for robotic total mesorectal excision for rectal cancer: lessons from a single surgeon's experience. Dis Colon Rectum. 2014; 57:1066–1074.
40. Sng KK, Hara M, Shin JW, Yoo BE, Yang KS, Kim SH. The multiphasic learning curve for robot-assisted rectal surgery. Surg Endosc. 2013; 27:3297–3307.
41. Jayne DG, Brown JM, Thorpe H, Walker J, Quirke P, Guillou PJ. Bladder and sexual function following resection for rectal cancer in a randomized clinical trial of laparoscopic versus open technique. Br J Surg. 2005; 92:1124–1132.
42. Sartori CA, Sartori A, Vigna S, Occhipinti R, Baiocchi GL. Urinary and sexual disorders after laparoscopic TME for rectal cancer in males. J Gastrointest Surg. 2011; 15:637–643.
43. Morino M, Parini U, Allaix ME, Monasterolo G, Brachet Contul R, Garrone C. Male sexual and urinary function after laparoscopic total mesorectal excision. Surg Endosc. 2009; 23:1233–1240.
44. Kim JY, Kim NK, Lee KY, Hur H, Min BS, Kim JH. A comparative study of voiding and sexual function after total mesorectal excision with autonomic nerve preservation for rectal cancer: laparoscopic versus robotic surgery. Ann Surg Oncol. 2012; 19:2485–2493.
45. Luca F, Valvo M, Ghezzi TL, Zuccaro M, Cenciarelli S, Trovato C, Sonzogni A, Biffi R. Impact of robotic surgery on sexual and urinary functions after fully robotic nerve-sparing total mesorectal excision for rectal cancer. Ann Surg. 2013; 257:672–678.
46. Ueno H, Mochizuki H, Hashiguchi Y, Hase K. Prognostic determinants of patients with lateral nodal involvement by rectal cancer. Ann Surg. 2001; 234:190–197.
47. Fujita S, Yamamoto S, Akasu T, Moriya Y. Lateral pelvic lymph node dissection for advanced lower rectal cancer. Br J Surg. 2003; 90:1580–1585.
48. Moriya Y, Sugihara K, Akasu T, Fujita S. Importance of extended lymphadenectomy with lateral node dissection for advanced lower rectal cancer. World J Surg. 1997; 21:728–732.
49. Kim TH, Jeong SY, Choi DH, Kim DY, Jung KH, Moon SH, Chang HJ, Lim SB, Choi HS, Park JG. Lateral lymph node metastasis is a major cause of locoregional recurrence in rectal cancer treated with preoperative chemoradiotherapy and curative resection. Ann Surg Oncol. 2008; 15:729–737.
50. Stearns MW Jr, Deddish MR. Five-year results of abdominopelvic lymph node dissection for carcinoma of the rectum. Dis Colon Rectum. 1959; 2:169–172.
51. Moriya Y, Hojo K, Sawada T, Koyama Y. Significance of lateral node dissection for advanced rectal carcinoma at or below the peritoneal reflection. Dis Colon Rectum. 1989; 32:307–315.
52. Marshall SJ, Hayn MH, Stegemann AP, Agarwal PK, Badani KK, Balbay MD, Dasgupta P, Hemal AK, Hollenbeck BK, Kibel AS, et al. Impact of surgeon and volume on extended lymphadenectomy at the time of robot-assisted radical cystectomy: results from the International Robotic Cystectomy Consortium (IRCC). BJU Int. 2013; 111:1075–1080.
53. Lee YS, Chong GO, Lee YH, Hong DG, Cho YL, Park IS. Robot-assisted total preservation of the pelvic autonomic nerve with extended systematic lymphadenectomy as part of nerve-sparing radical hysterectomy for cervical cancer. Int J Gynecol Cancer. 2013; 23:1133–1138.
54. Zhang YJ, Yin L, Huang L, Zhang HB, Han Y, Lin MB. Long-term results of intersphincteric resection for low rectal cancer. J Invest Surg. 2013; 26:217–222.
55. Yamada K, Ogata S, Saiki Y, Fukunaga M, Tsuji Y, Takano M. Long-term results of intersphincteric resection for low rectal cancer. Dis Colon Rectum. 2009; 52:1065–1071.
56. Pigazzi A, Ellenhorn JD, Ballantyne GH, Paz IB. Robotic-assisted laparoscopic low anterior resection with total mesorectal excision for rectal cancer. Surg Endosc. 2006; 20:1521–1525.
57. Park SY, Choi GS, Park JS, Kim HJ, Ryuk JP. Short-term clinical outcome of robot-assisted intersphincteric resection for low rectal cancer: a retrospective comparison with conventional laparoscopy. Surg Endosc. 2013; 27:48–55.
58. AlAsari S, Lim D, Kim N. Robotic hemi-levator excision for low rectal cancer: a novel technique for sphincter preservation. OA Robot Surg. 2013; 1:3.
59. Marr R, Birbeck K, Garvican J, Macklin CP, Tiffin NJ, Parsons WJ, Dixon MF, Mapstone NP, Sebag-Montefiore D, Scott N, et al. The modern abdominoperineal excision: the next challenge after total mesorectal excision. Ann Surg. 2005; 242:74–82.
60. Marecik SJ, Zawadzki M, Desouza AL, Park JJ, Abcarian H, Prasad LM. Robotic cylindrical abdominoperineal resection with transabdominal levator transection. Dis Colon Rectum. 2011; 54:1320–1325.
61. Choi HK, Law WL, Ho JW. Leakage after resection and intraperitoneal anastomosis for colorectal malignancy: analysis of risk factors. Dis Colon Rectum. 2006; 49:1719–1725.
62. Kingham TP, Pachter HL. Colonic anastomotic leak: risk factors, diagnosis, and treatment. J Am Coll Surg. 2009; 208:269–278.
63. Karliczek A, Harlaar NJ, Zeebregts CJ, Wiggers T, Baas PC, van Dam GM. Surgeons lack predictive accuracy for anastomotic leakage in gastrointestinal surgery. Int J Colorectal Dis. 2009; 24:569–576.
64. Alander JT, Kaartinen I, Laakso A, Pätilä T, Spillmann T, Tuchin VV, Venermo M, Välisuo P. A review of indocyanine green fluorescent imaging in surgery. Int J Biomed Imaging. 2012; 2012:940585.
65. Jafari MD, Lee KH, Halabi WJ, Mills SD, Carmichael JC, Stamos MJ, Pigazzi A. The use of indocyanine green fluorescence to assess anastomotic perfusion during robotic assisted laparoscopic rectal surgery. Surg Endosc. 2013; 27:3003–3008.
66. Kudszus S, Roesel C, Schachtrupp A, Höer JJ. Intraoperative laser fluorescence angiography in colorectal surgery: a noninvasive analysis to reduce the rate of anastomotic leakage. Langenbecks Arch Surg. 2010; 395:1025–1030.
67. Bae SU, Baek SJ, Hur H, Baik SH, Kim NK, Min BS. Intraoperative near infrared fluorescence imaging in robotic low anterior resection: three case reports. Yonsei Med J. 2013; 54:1066–1069.
68. Baek SJ, Kim SH, Cho JS, Shin JW, Kim J. Robotic versus conventional laparoscopic surgery for rectal cancer: a cost analysis from a single institute in Korea. World J Surg. 2012; 36:2722–2729.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download