1. Stam J, van Stuijvenberg M, Grüber C, Mosca F, Arslanoglu S, Chirico G, Braegger CP, Riedler J, Boehm G, Sauer PJ, et al. Multicenter Infection Prevention Study 1 (MIPS 1) Study Group. Antibiotic use in infants in the first year of life in five European countries. Acta Paediatr. 2012; 101:929–934.
2. Holstiege J, Garbe E. Systemic antibiotic use among children and adolescents in Germany: a population-based study. Eur J Pediatr. 2013; 172:787–795.
3. Vernacchio L, Kelly JP, Kaufman DW, Mitchell AA. Medication use among children <12 years of age in the United States: results from the Slone Survey. Pediatrics. 2009; 124:446–454.
4. Risnes KR, Belanger K, Murk W, Bracken MB. Antibiotic exposure by 6 months and asthma and allergy at 6 years: Findings in a cohort of 1,401 US children. Am J Epidemiol. 2011; 173:310–318.
5. Ng SC, Bernstein CN, Vatn MH, Lakatos PL, Loftus EV Jr, Tysk C, O'Morain C, Moum B, Colombel JF. Epidemiology and Natural History Task Force of the International Organization of Inflammatory Bowel Disease (IOIBD). Geographical variability and environmental risk factors in inflammatory bowel disease. Gut. 2013; 62:630–649.
6. Chang HT, Krezolek D, Johnson S, Parada JP, Evans CT, Gerding DN. Onset of symptoms and time to diagnosis of Clostridium difficile-associated disease following discharge from an acute care hospital. Infect Control Hosp Epidemiol. 2007; 28:926–931.
7. Baquero F, Negri MC, Morosini MI, Blázquez J. Antibiotic-selective environments. Clin Infect Dis. 1998; 27:S5–S11.
8. Austin DJ, Kristinsson KG, Anderson RM. The relationship between the volume of antimicrobial consumption in human communities and the frequency of resistance. Proc Natl Acad Sci U S A. 1999; 96:1152–1156.
9. Urbánek K, Kolár M, Lovecková Y, Strojil J, Santavá L. Influence of third-generation cephalosporin utilization on the occurrence of ESBL-positive Klebsiella pneumoniae strains. J Clin Pharm Ther. 2007; 32:403–408.
10. Steinman MA, Landefeld CS, Gonzales R. Predictors of broad-spectrum antibiotic prescribing for acute respiratory tract infections in adult primary care. JAMA. 2003; 289:719–725.
11. Hersh AL, Shapiro DJ, Pavia AT, Shah SS. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics. 2011; 128:1053–1061.
12. Jacobs MR, Johnson CE. Macrolide resistance: an increasing concern for treatment failure in children. Pediatr Infect Dis J. 2003; 22:S131–S138.
13. McCaig LF, Besser RE, Hughes JM. Trends in antimicrobial prescribing rates for children and adolescents. JAMA. 2002; 287:3096–3102.
14. Grijalva CG, Nuorti JP, Griffin MR. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA. 2009; 302:758–766.
15. Halasa NB, Griffin MR, Zhu Y, Edwards KM. Decreased number of antibiotic prescriptions in office-based settings from 1993 to 1999 in children less than five years of age. Pediatr Infect Dis J. 2002; 21:1023–1028.
16. Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997; 278:901–904.
17. Nyquist AC, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA. 1998; 279:875–877.
18. Pichichero ME. Dynamics of antibiotic prescribing for children. JAMA. 2002; 287:3133–3135.
19. Jeong HS. Korea's National Health Insurance--lessons from the past three decades. Health Aff (Millwood). 2011; 30:136–144.
20. Kim LY, Sakong J, Kim Y, Kim SR, Kim SY, Tchoe BH, Jeong H, Lee TR. Developing the inpatient sample for the National Health Insurance claims data. Health Policy Manag. 2013; 23:152–161.
21. Park BJ, Sung JH, Park KD, Seo SW. Report of the evaluation for validity of discharged diagnoses in Korean Health Insurance Database. Seoul: Seoul National University College of Medicine;2003.
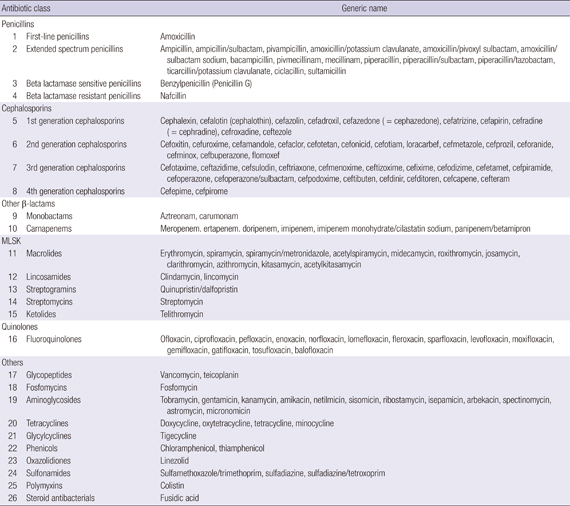
22. Deck DH, Winston LG. Chemotherapeutic drugs. In : Katzung BG, Masters SB, Trevor AJ, editors. Basic & clinical pharmacology. 12th ed. New York: McGraw-Hill Medical;2012.
23. Kim DS, Kim NS, Lee SH. Determination of defined daily dose of medicines using nominal group technique and analysis of antibiotics use in national insurance claim data: focused on antibiotics without DDD of WHO. Korean J Clin Pharm. 2007; 17:19–32.
24. Mainous AG 3rd, Hueston WJ, Davis MP, Pearson WS. Trends in antimicrobial prescribing for bronchitis and upper respiratory infections among adults and children. Am J Public Health. 2003; 93:1910–1914.
25. Finkelstein JA, Stille C, Nordin J, Davis R, Raebel MA, Roblin D, Go AS, Smith D, Johnson CC, Kleinman K, et al. Reduction in antibiotic use among US children, 1996-2000. Pediatrics. 2003; 112:620–627.
26. Rahal JJ, Urban C, Horn D, Freeman K, Segal-Maurer S, Maurer J, Mariano N, Marks S, Burns JM, Dominick D, et al. Class restriction of cephalosporin use to control total cephalosporin resistance in nosocomial Klebsiella. JAMA. 1998; 280:1233–1237.
27. Youn YS, Lee KY. Mycoplasma pneumoniae pneumonia in children. Korean J Pediatr. 2012; 55:42–47.
28. Mulholland S, Gavranich JB, Chang AB. Antibiotics for community-acquired lower respiratory tract infections secondary to Mycoplasma pneumoniae in children. Cochrane Database Syst Rev. 2010; CD004875.
29. Daneman N, McGeer A, Green K, Low DE. Macrolide resistance in bacteremic pneumococcal disease: implications for patient management. Clin Infect Dis. 2006; 43:432–438.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download