Abstract
Infectious diseases have historically resulted in suspended or cancelled military operations. Vaccination for disease prevention is a critical component of the military's force readiness doctrine. Until recently, Korea had not recognized the importance of vaccinating military personnel. However, a 2011 meningococcal disease outbreak at an army recruit training center led to dramatic changes in the paradigm of traditional medical practice in the Korean armed forces. A new vaccination policy was formed by a 2012 Military Healthcare Service Act. Since then, Neisseria meningitidis, hepatitis A, and measles-mumps-rubella vaccines have been routinely administered to all new recruits early in basic training to ensure protection against these diseases. All active-duty soldiers also receive seasonal influenza vaccination annually. Despite quantitative improvements in vaccination policies, several instances of major infectious diseases and adverse vaccine reactions have threatened soldier health. In the future, vaccination policies in the Korean armed forces should be based on epidemiologic data and military medical research for vaccine use and safety management.
Infectious disease has had a tremendous impact on warfare and armed forces. During the World War I, an influenza pandemic was responsible for 791,907 primary admissions and 44,270 deaths of American soldiers due to pneumonia and influenza (1). During the epidemic, about 40% of military personnel were infected (2). In the Korean War, hemorrhagic fever with renal syndrome caused by Hantaan virus affected more than 3,000 soldiers, with a 10% mortality rate (3, 4). Infectious diseases in military personnel could spread easily and lead to largescale epidemics even outside times of war. The potential loss of military power means that epidemic outbreaks in military populations have larger ripple effects than in civilian communities. Hence, the priority of military medicine is to prevent disease and keep soldiers healthy. Vaccination is a key to achieving this primary target (5, 6).
Mandatory military service is required of adult Korean men over 18 yr of age; therefore, young men around 20 yr of age generally are enlisted as soldiers. Because enrolled soldiers are typically healthy young men, their risks of disease are generally lower than other age groups. However, soldier age, working environment, and military activities increase risk of certain infectious diseases. Young soldiers live in crowded conditions and participate in activities in fields and mountains, resulting in higher incidence rates and outbreaks of airborne diseases such as chicken pox, tuberculosis, influenza, and meningococcal disease than community populations (7, 8, 9, 10, 11, 12, 13, 14, 15). At basic training sites, new recruits from different geographical and socioeconomic backgrounds gather and live in close contact. New recruits have the highest risk of developing infectious disease because they are exposed to microbes against which they have been not immunized (16). Outdoor activities increase risks of vector-borne diseases such as scrub typhus, hemorrhagic fever with renal syndrome due to Hantaan virus, and leptospirosis (17, 18, 19). In addition, modern military missions involve not only warfare, but also disaster relief from earthquakes and floods as well as overseas deployment for international peacekeeping (20, 21). It is often difficult to maintain sufficient hygiene in various parts of the world during these operations. For example, troops dispatched to South Sudan could be exposed to severe endemic diseases, such as meningococcal disease or tropical malaria (22). Troops must also be prepared for the possibility of bioterrorism or biowarfare (23, 24, 25). Smallpox, anthrax, and plague are easily transmitted and have high prevalence and mortality. Combined, these characteristics of modern military operations provide support for vaccination of healthy young soldiers.
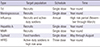
The US military has a long history of vaccination to prevent communicable diseases based on previous experiences (26). However, the Korean military only recently recognized the value of vaccination. In 2011, an outbreak of meningococcal disease at an army basic training center raised awareness of the importance of military vaccination and increased momentum to expand vaccination programs (27). A military healthcare service act passed in March 2012 enforced development of an immunization schedule for Korean soldiers, including vaccine type and timing (28). Before 2011, soldiers received vaccines against tetanus, influenza, Hantaan virus, typhoid fever, and cholera (29). However, cholera vaccination was suspended in the early 1990s due to changing disease epidemiology, and typhoid vaccination is administered only to food handlers. Table 1 shows the current soldier immunization schedule.
The tetanus toxoid vaccine was used until 2011, but the tetanus-diphtheria toxoids (Td) vaccine is currently administered to new recruits due to its suspended production. Because soldiers may be wounded outdoors, especially in battle where proper wound management is difficult, tetanus vaccination is mandatory. In Korea, around 10 adult tetanus cases have been reported annually since 2000 (30). A total of 9 tetanus cases have been reported since 2006 in Korean soldiers (31). Although data on tetanus immunity in new recruits is not available before enlistment, 25.0% of teens and 42.0% of people in their 20s in the Korean population require booster vaccination to sustain protective immunity (32). Currently enlisted soldiers have a 90% rate of childhood universal Diphtheria toxoid-Tetanus toxoid-acellular Pertussis (DTaP) vaccination coverage. However, it is unlikely that they received an adult Td vaccine booster in their 20s. Therefore, new recruits typically receive a single dose Td vaccine. Td vaccination coverage in Korean soldiers was 87% from July 2005 to January 2007 (33).
The Hantaan virus vaccine (Hantavax®) has been administered to soldiers in high-risk areas for hemorrhagic fever with renal syndrome (HFRS) since 1993. The Korean armed forces classified army units with one more patient diagnosed with HFRS in the previous three years, or any HFRS-associated mortality in the last 5 yr as high-risk areas. Although millions of Hantavirus vaccine doses were administered to soldiers, its protective effectiveness remains controversial (34, 35). Although the vaccine failed to provide field effectiveness in a case-control study among soldiers in early 2000, the number of HFRS cases among Korean soldiers declined after introduction of the vaccine (36). Before its introduction, 50-80 HFRS cases were reported annually through 1993, and this incidence has declined to 20-40 annual cases since 2000 (Fig. 1). This reduced HFRS incidence in the Korean armed forces might be related to vaccination, but also suggests that climate changes and other factors might be associated with variation in annual incidence rates.
Meningococcal disease incidence is highest in infants below 1 yr old, with a second peak in adolescents between 15-24 yr of age (37). New military recruits in their 20s are a well-known high-risk group. The U.S. military administered a monovalent serogroup C meningococcal vaccine from 1971 until 1982, when the vaccine was replaced by a quadrivalent meningococcal polysaccharide vaccine (MPSV4) for serogroups A, C, Y, and W135 (38). This vaccine, in turn, was replaced by another quadrivalent meningococcal conjugate vaccine, MCV4, which has been administered to US military trainees since 2007 (39). Meningococcal vaccination has decreased the overall incidence of meningococcal disease among US military personnel by more than 90% (14). From 2006-2010, the incidence rate among US military members was 0.38 cases per 100,000 person-years, a rate not significantly different from age-matched general US populations. This long history of meningococcal vaccination in the US military provided the evidence to support vaccination of college freshman since 2000 (40). Since 2005, despite its high cost, routine MCV4 vaccination against Neisseria meningitidis was initiated for young adolescents aged 11-12 yr in addition to groups with increased risks such as college freshmen living in dormitories, military recruits, and patients with asplenia and terminal complement deficiencies (41, 42). The incidence rate of meningococcal disease in Korean soldiers was assessed during a meningococcal epidemic in civilian populations in the late 1980s and early 2000s. During 1988-1991, the annual incidence rate of meningococcal disease was 0.8-3.3 cases per 100,000 new recruits, and 0.5-1.3 cases per 100,000 soldiers (43). From 2000 to 2001, the annual incidence rate was 2.2 cases per 100,000 soldiers (11). Meningococcal disease has a mortality rate above 10%, and 15% of survivors experience severe sequelae such as neurological deficits and loss of limbs (44). Thus, the necessity of vaccination for new recruits has been emphasized. Four cases of meningococcal disease and 1 case of mortality were reported at an Army basic training center in April 2011. This outbreak led to required meningococcal vaccination of all recruits starting in 2012. Although microbiological data on meningococcal disease in Korean soldiers are limited, a military study in early 2000 confirmed patient infection of Neisseria meningitidis serogroups A and C (11). All cases since 2010 have been serogroup W135 (45). Based on this microbiological data and herd immunity, the MCV4 (Menveo®; Novartis Vaccines and Diagnostics, Cambridge, Massachusetts, USA) vaccine is currently used.
Respiratory infection is the most prevalent disease because of closed and clustered military environments (46). During the World War I, about 40% of all US military soldiers were infected with influenza virus, and 1.5% died from either influenza or associated pneumonia (2, 39). Thus, soon after development of the influenza vaccine in the mid-1940s, all 7 million US troops were vaccinated against influenza (39). In the early 2000s in Korea, several trainee deaths during basic training from pneumonia with unknown etiology during seasonal influenza epidemics led to seasonal influenza vaccination of new recruits starting in 2004 (47). Since 2012, influenza vaccination has expanded to all active-duty soldiers. In Korea, sentinel surveillance for influenza-like illness (ILI) among soldiers was started in late 2011. Surveillance in the 2011-12 season revealed that ILI in military populations was 2- to 10-fold higher than in civilian populations during non-epidemic seasons and 4- to 8-fold higher during the epidemic season, compared to ILI surveillance data from the Korean Center for Disease Control and Prevention (Fig. 2) (10). The seasonal influenza vaccination rate among soldiers in 2012 was approximately 80%. Further assessment of influenza vaccine effectiveness using ILI surveillance data is necessary.
Hepatitis A virus (HAV) is transmitted person-to-person by fecal-oral transmission and also spread through contaminated food or drinking water. Hepatitis A infections could lead to epidemics in military populations because of working conditions. In Korea, a hepatitis A outbreak of 102 cases was reported in northwest region of Gyeonggi-do in 1998 (48). In May-August 2007, a unit in Gangwon-do Province suffered an outbreak of hepatitis A, resulting in 73 cases among 332 military personnel (49). From 2001 to 2005, the hepatitis A incidence rate was 1.6 to 9.8 cases per 100,000 military personnel (50). In 2009, the number increased to 34.5 cases (51). Considering the low HAV seroprevalence among adolescents (11%-18%) and the high incidence rate among Korean soldiers, the HAV vaccine has been administered to new recruits since 2012 (52). HAV vaccination can produce protective antibodies in 95% of vaccinees by single-dose vaccination, and provide protective immunity for at least 2 yr (53). Although HAV vaccine has recommended 2-dose schedule with intervals of 6 to 18 months for Korean adults, single-dose HAV vaccination has been partially introduced for new recruits serving 21-24 months on the front line area from 2013. It will be progressively expanded to all military trainees.
Measles and mumps are highly infectious and easily spread among susceptible soldiers living in crowded conditions such as military barracks. These diseases have historically been major causes of non-battle-related disease in wars during the pre-vaccine era (54). Since 2000, the Korean armed forces have reported 0-2 annual cases of measles and rubella. However, mumps cases have continued to increase since 2005 (Fig. 3) (51). The annual incidence rate of mumps over the last five years has reached 28-80 cases per 100,000 soldiers. Since 2001, when pre-school children were required to submit vaccination records showing a second MMR dose to enter schools, the 2-dose vaccination rate among pre-teen adolescents is more than 95%. The increased incidence of mumps among young Korean soldiers born before 1993 was suspected to be associated with a lack of a second MMR vaccine dose (55). The seroprevalence of mumps among young Korean soldiers was 81.1% in 2010 (56). To prevent mumps epidemics, a herd immunity threshold above 88%-92% is required (57). Thus, a temporary single-dose MMR vaccination program was initiated without antibody testing for new recruits enlisting in basic training camps from April to June until recruits born after 1995 who had received 2-dose MMR vaccines joined the military. Despite high 2-dose MMR vaccine coverage, mumps outbreaks continue to occur in young adults and adolescents living in crowded environments such as military bases and schools (58, 59, 60). Mumps outbreaks in highly vaccinated populations might be due to multiple factors such as waning immunity, antigenic difference between vaccine and outbreak strains, or dense populations in schools (61). Continued mumps outbreaks in community populations suggest that high childhood 2-dose MMR vaccination rates based on national immunization program policies may not decrease mumps incidence in young Korean soldiers. All new recruits have been vaccinated against MMR in all seasons since 2012. A number of recruits may have received a third MMR vaccine dose under this policy.
Respiratory infection is the most common infectious disease among soldiers that requires hospitalization and treatment. New recruits have 2- to 10-fold higher hospitalization rates for acute respiratory diseases compared to active-duty soldiers (62). Adenovirus is the major cause of respiratory infection among recruits (63). In the US military, 10% of recruits are infected with adenovirus during early phases of basic training, and 90% of pneumonia cases are caused by adenovirus infections (16). An oral live attenuated vaccine for adenovirus serotypes 4 and 7 was administered to recruits starting in 1971, followed by a rapid decrease in adenovirus-related respiratory infections (64). Since 1996, when vaccine production ceased, incidence of acute respiratory infections due to adenovirus infections resurged with reported mortality (65, 66). A second-generation adenovirus vaccine has been administered to U.S. military trainees since 2011 (67). From 2011 to 2012 in Korea, 6 cases of severe adenovirus pneumonia have been reported, with 3 deaths (68). During the same period in the Armed Forces Capital Hospital, 63.2% of patients diagnosed with acute lower respiratory infection tested for respiratory viruses were positive for adenovirus infections (63). Because the Korean military is expected to have a similar disease burden as the US military, adenovirus vaccination should be considered despite the current unavailability of the vaccine in Korea. Studies on adenovirus serotypes and disease burden in Korean soldiers are necessary for development of an adenovirus vaccination program.
Pertussis has high incidence among foreign militaries, and an increasing incidence among young adults and adolescents in Korea (69, 70). Currently enlisted soldiers in their 20s are unlikely to have protective immunity against pertussis from their childhood DTaP vaccine, as more than 10 yr have passed since their last DTaP vaccination. Considering the community incidence and waning pertussis immunity in this age group, pertussis might also increase among Korean soldiers. However, there is no current data on the incidence of pertussis among military personnel. The switch from Td to the Tdap vaccine that includes protection against pertussis has been suspended because of scant epidemiologic data and budget shortfalls.
In 2012, the Korean armed forces purchased 1.69 million vaccine doses, a 3-fold increase over 2009, when only 0.63 million doses were used. The vaccination budget for Korean soldiers has increased 6-fold in the past five years (Fig. 4). Vaccination is necessary for military medicine to preserve combat effectiveness. However, vaccination can also lead to safety issues. Current soldier vaccination programs are mainly conducted outside military medical facilities as mass immunizations of thousands of new recruits at basic training sites. Consequently, it is difficult to manage adverse reactions such as anaphylaxis and post vaccination syncope (71, 72). In addition, constant monitoring and surveillance is required to detect severe adverse central nervous system events such as Guillain-Barre syndrome. However, adverse event surveillance systems following vaccination are very limited. Management of vaccination records through electronic systems is another important issue (73, 74). Currently, vaccination records are application forms manually filed and stored at each military base. This makes difficult to track vaccination coverage for individual soldiers. Armed forces vaccination programs are related to national immunization policies. Therefore, an exchange of information between national and military vaccination programs is required to avoid overlap and inadequate vaccination.
Soldiers confront a variety of infectious diseases associated with military operations, such as battles and biological warfare, as well as age-specific disease epidemiology. Vaccination of military populations is more cost-effectiveness than civilian populations because vaccination not only prevents transmission of communicable diseases, but also minimizes health-related reduction of fighting power. The Korean armed forces have recognized the value of military preventive medicine and vaccination. New recruits received booster vaccinations only for tetanus before 2012. Thereafter, programs to administer meningococcal disease, influenza, MMR, and hepatitis A vaccines to recruits and active-duty soldiers were adopted or expanded. Although various types of vaccinations have been administered to soldiers, the Korean armed forces are still not well organized to manage vaccination records or monitor adverse events following vaccination. Furthermore, more research on vaccine effectiveness and disease epidemiology is necessary to validate the adequacy of existing vaccines and to evaluate the necessity of newly introduced vaccines.
Figures and Tables
Fig. 1
Number of reported HFRS cases and Hantavax® consumption in Korean military personnel, 1990-2012.

Fig. 2
Incidence of Influenza-like Illness (ILI) in Korean military and civilian population, 2011-2012. aILI cases per 1,000 patients-week; bLaboratory-confirmed influenza cases per 10,000 patients-week on military hospitals.

Table 1
Current administered vaccines for Korean military service members
References
1. Siler JF. The U.S. Army Medical Department in the World War. Vol 9: Communicable and other diseases. Washinnton: U.S. Government Printing Office;1928. p. 66–70.
2. Gray GC, Feighner B, Trump DH, Berg SW, Zajdowicz MJ, Zajdowicz TR. Disease spread by close personal contact. In : Lenhart MK, Lounsbury DE, editors. Military Preventive Medicine: Mobilization and Deployment, Vol 2. Washington DC: Borden Institute;2005. p. 1127–1128.
3. Chun CH, Kim SW, Kim WD, Yoon HJ. Changing patterns of epidemiology and death: Causes on epidemic hemorrhagic fever in Korea. Korean J Infect Dis. 1976; 8:58–74.
4. Johnson KM. Hantaviruses: history and overview. Curr Top Microbiol Immunol. 2001; 256:1–14.
5. Murray CK, Horvath LL. An approach to prevention of infectious diseases during military deployments. Clin Infect Dis. 2007; 44:424–430.
6. Artenstein AW, Opal JM, Opal SM, Tramont EC, Peter G, Russell PK. History of U.S. military contributions to the study of vaccines against infectious diseases. Mil Med. 2005; 170:3–11.
7. Mancuso JD, Tobler SK, Eick AA, Keep LW. Active tuberculosis and recent overseas deployment in the U.S. military. Am J Prev Med. 2010; 39:157–163.
8. Finnie TJ, Copley VR, Hall IM, Leach S. An analysis of influenza outbreaks in institutions and enclosed societies. Epidemiol Infect. 2014; 142:107–113.
9. Duron S, Mayet A, Lienhard F, Haus-Cheymol R, Verret C, Védy S, Le Guen P, Berbineau L, Brisou P, Dubrous P, et al. MISS staff. The French Military influenza surveillance system (MISS): overview of epidemiological and virological results during four influenza seasons--2008-2012. Swiss Med Wkly. 2013; 143:w13848.
10. Heo JY, Yoon CG, Kim KH, Choe KW. Incidence of influenza-like illness in Korean military personnel: comparison between military and community population. In : International Interscience Conference on Infection and Chemotherapy; 2013; Seoul, Korea.
11. Lee SO, Ryu SH, Park SJ, Ryu J, Woo JH, Kim YS. Meningococcal disease in the republic of Korea army: incidence and serogroups determined by PCR. J Korean Med Sci. 2003; 18:163–166.
12. Kang CI, Choi CM, Kim DH, Kim CH, Lee DJ, Kim HB, Kim NJ, Oh MD, Choe KW. Pulmonary tuberculosis in young Korean soldiers: incidence, drug resistance and treatment outcomes. Int J Tuberc Lung Dis. 2006; 10:970–974.
13. Lee SW, Jang YS, Park CM, Kang HY, Koh WJ, Yim JJ, Jeon K. The role of chest CT scanning in TB outbreak investigation. Chest. 2010; 137:1057–1064.
14. Broderick MP, Faix DJ, Hansen CJ, Blair PJ. Trends in meningococcal disease in the United States military, 1971-2010. Emerg Infect Dis. 2012; 18:1430–1437.
15. Kang CI, Choi CM, Park TS, Lee DJ, Oh MD, Choe KW. Incidence of herpes zoster and seroprevalence of varicella-zoster virus in young adults of South Korea. Int J Infect Dis. 2008; 12:245–247.
16. Gray GC, Callahan JD, Hawksworth AW, Fisher CA, Gaydos JC. Respiratory diseases among U.S. military personnel: countering emerging threats. Emerg Infect Dis. 1999; 5:379–385.
17. Song JY, Chun BC, Kim SD, Baek LJ, Kim SH, Sohn JW, Cheong HJ, Kim WJ, Park SC, Kim MJ. Epidemiology of hemorrhagic fever with renal syndrome in endemic area of the Republic of Korea, 1995-1998. J Korean Med Sci. 2006; 21:614–620.
18. Kim SS, Kim JS. Epiderniologic characteristics and trends of leptospirosis in Korea by literature review. Korean J Epidemiol. 1994; 16:66–83.
19. Sames WJ, Kim HC, Klein TA. Perspectives on scrub typhus, tick-borne pathogens, and hantavirus in the Republic of Korea. US Army Med Dep J. 2009; 40–49.
20. Baker MS, Ryals PA. The medical department in military operations other than war. Part I. Planning for deployment. Mil Med. 1999; 164:572–579.
21. Ryals PA, Baker MS. Military medicine in operations other than war. Part II: Humanitarian relief missions for Naval Reserve fleet hospitals. Mil Med. 1996; 161:502–504.
22. Ministry of National Defense. Current overseas deployment of Korean armed forces in five Asian and African counties 2013. accessed on 1 September 2014. Available at http://www.index.go.kr/egams/stts/jsp/potal/stts/PO_STTS_IdxMain.jsp?idx_ cd=1715&bbs=INDX_001&clas_div=C&rootKey=1.48.0.
23. Korean Center for Diseases Control. Current preparedness against bioterrorism using smallpox in Korea. accessed on 1 September 2014. Available at http://www.cdc.go.kr/CDC/info/CdcKrInfo0301.jsp?menuIds=HOME001-MNU1132-MNU1138-MNU0037-MNU1380&cid=12467.
24. Rusnak JM, Boudreau EF, Hepburn MJ, Martin JW, Bavari S. Medical Counter measures. In : Lenhart MK, Lounsbury DE, editors. Medical Aspects of Biological Warfare. Washington DC: Borden Institute;2007. p. 465–467.
25. Korean Center for Diseases Control. Trends in development of Anthrax Vaccine. accessed on 1 September 2014. Available at http://www.cdc.go.kr/CDC/info/CdcKrInfo0301.jsp?menuIds=HOME001-MNU1132-MNU1138-MNU0037-MNU1380&cid=12372.
26. Artenstein AW. Vaccines for military use. Vaccine. 2009; 27:D16–D22.
27. Lee SO. Commencement of the meningococcal vaccination for the republic of Korea army. Infect Chemother. 2013; 45:113–115.
28. Ministry of Goverment Legislation. Act on Military Healthcare Service. accessed on 1 September 2014. Available at http://www.law.go.kr/lsInfoP.do?lsiSeq=124038&efYd=20120922#0000.
29. Ministry of National Defense. Manual for military immunization. 2010.
30. Korea Centers for Disease Control and Prevention. Disease web statistics system. accessed on 1 September 2014. Available at http://is.cdc.go.kr/nstat/index.jsp.
31. Armed Forces Medical Research Institute. Infect Dis Wkly Rep. 2013; 7:3–4.
32. Lee SY, Kim JS, Ahn JH, Choi JH, Ma SH, Park JS, Kim HM, Kang JH. Immunoassay of Diphtheria and Tetanus according to Ages. Infect Chemother. 2012; 44:62–66.
33. Kim CK, Shin JH. Qualitative analysis of the tetanus antibody in Korean Army Personnel after visiting a Tertiary Armed Forces Hospital. J Korean Soc Traumatol. 2007; 20:65–71.
34. Chu YK, Gligic A, Tomanovic S, Bozovjc B, Obradovic M, Woo YD, An CN, Kim H, Jiang YS, Park SC, et al. A field efficacy trial of inactivated Hantaan Virus Vaccine (Hantavax(TM)) against hemorrhagic fever with renal syndrome (HFRS) in the endemic areas of Yugoslavia from 1996 to 1998. J Korean Soc Virol. 1999; 29:55–64.
35. Sohn YM, Rho HO, Park MS, Kim JS, Summers PL. Primary humoral immune responses to formalin inactivated hemorrhagic fever with renal syndrome vaccine (Hantavax): consideration of active immunization in South Korea. Yonsei Med J. 2001; 42:278–284.
36. Park K, Kim CS, Moon KT. Protective effectiveness of hantavirus vaccine. Emerg Infect Dis. 2004; 10:2218–2220.
37. Rosenstein NE, Perkins BA, Stephens DS, Lefkowitz L, Cartter ML, Danila R, Cieslak P, Shutt KA, Popovic T, Schuchat A, et al. The changing epidemiology of meningococcal disease in the United States, 1992-1996. J Infect Dis. 1999; 180:1894–1901.
38. Gunzenhauser JD. Communicable Disease Control in Basic Training: Programmatic Aspect. In : Kelley PW, editor. Military Preventive Medicine: Mobilization and Deployment, Vol 1. Washington DC: Borden Institute;2003. p. 145–150.
39. Grabenstein JD, Pittman PR, Greenwood JT, Engler RJ. Immunization to protect the US Armed Forces: heritage, current practice, and prospects. Epidemiol Rev. 2006; 28:3–26.
40. Meningococcal disease and college students. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2000; 49:13–20.
41. Bilukha OO, Rosenstein N. National Center for Infectious Diseases, Centers for Disease Control and Prevention (CDC). Prevention and control of meningococcal disease Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2005; 54:1–21.
42. Shepard CW, Ortega-Sanchez IR, Scott RD 2nd, Rosenstein NE. ABCs Team. Cost-effectiveness of conjugate meningococcal vaccination strategies in the United States. Pediatrics. 2005; 115:1220–1232.
43. Park HS, Chun YI. Vaccination effect on pharyngeal carrier rate of Neis seria meningitidis and its serogroups in Korean Army Recruits. J Korean Mil Med Assoc. 1992; 23:105–115.
44. Rosenstein NE, Perkins BA, Stephens DS, Popovic T, Hughes JM. Meningococcal disease. N Engl J Med. 2001; 344:1378–1388.
45. Sim SH, Heo JY, Kim EC, Choe KW. A case of meningococcal sepsis and meningitis with complement 7 deficiency in a military trainee. Infect Chemother. 2013; 45:94–98.
46. Pazzaglia G, Pasternack M. Recent trends of pneumonia morbidity in US Naval personnel. Mil Med. 1983; 148:647–651.
47. Kim HY. Seven Mortality cases by pneumonia in military recruits during 2004-05 influenza season. Nocutnews. 2005. 09. 22. accessed on 1 September 2014. Available at http://www.nocutnews.co.kr/show.asp?idx=74568.
48. Seng W, Maeng S. Acute Hepatitis A in some brigade. J Korean Mil Med Assoc. 2008; 39:130–135.
49. Han SH, Lee SH, Roh BJ, Shim SC, Cho SC, Sohn JH, Lee DH, Kee CS. An outbreak of hepatitis A in South Korean military personnel: a clinical and epidemiologic study. Korean J Hepatol. 2001; 7:392–400.
50. Kang CI, Choi CM, Park TS, Lee DJ, Oh MD, Choe KW. Incidence and seroprevalence of hepatitis A virus infections among young Korean soldiers. J Korean Med Sci. 2007; 22:546–548.
51. Armed Forces Medical Command. Defense Medical Defense Medical Statics Information System(DMSIS). 2013.
52. Heo JY, Song JY, Noh JY, Seo YB, Kim IS, Choi WS, Kim WJ, Cho GJ, Hwang TG, Cheong HJ. Low level of immunity against hepatitis A among Korean adolescents: vaccination rate and related factors. Am J Infect Control. 2013; 41:e97–e100.
53. Orr N, Klement E, Gillis D, Sela T, Kayouf R, Derazne E, Grotto I, Balicer R, Huerta M, Aviram L, et al. Long-term immunity in young adults after a single dose of inactivated Hepatitis A vaccines. Vaccine. 2006; 24:4328–4332.
54. Weese C, Clark K, Goldman D, Underwood PK. Diseases Controlled Primarily by Vaccination. In : Kelley PW, editor. Military Preventive Medicine: Mobilization and Deployment. Washington, D. C.: Borden Institute, Walter Reed Army Medical Center;2005. p. 1215–1223.
55. Choi YH, Kim BN. Measle-Mumps-Rubella. Korean Society of Infectious Diseases. Vaccination for adult. 2nd ed. Seoul: M.I.P;2012. p. 236–253.
56. Park Y, Lee H, Lee Y, Hwang J, Kim K, Kim J. Seroprevalence of Mumps and Seroconversion Rate after MMR Vaccination in ROK Army. Koean J Mil Med Assoc. 2012; 43:29–34.
57. Anderson RM, May RM. Vaccination and herd immunity to infectious diseases. Nature. 1985; 318:323–329.
58. Gobet A, Mayet A, Journaux L, Dia A, Aigle L, Dubrous P, Michel R. Mumps among highly vaccinated people: investigation of an outbreak in a French Military Parachuting Unit, 2013. J Infect. 2014; 68:101–102.
59. Park DW, Nam MH, Kim JY, Kim HJ, Sohn JW, Cho Y, Song KJ, Kim MJ. Mumps outbreak in a highly vaccinated school population: assessment of secondary vaccine failure using IgG avidity measurements. Vaccine. 2007; 25:4665–4670.
60. Dayan GH, Quinlisk MP, Parker AA, Barskey AE, Harris ML, Schwartz JM, Hunt K, Finley CG, Leschinsky DP, O'Keefe AL, et al. Recent resurgence of mumps in the United States. N Engl J Med. 2008; 358:1580–1589.
61. Dayan GH, Rubin S. Mumps outbreaks in vaccinated populations: are available mumps vaccines effective enough to prevent outbreaks? Clin Infect Dis. 2008; 47:1458–1467.
62. John HD. Acute Respiratory Disease Among New Recruits. Am J Public Health Nations Health. 1946; 36:439–450.
63. Heo JY, Lee JE, Kim HK, Choe KW. Acute lower respiratory tract infections in soldiers, South Korea, April 2011-March 2012. Emerg Infect Dis. 2014; 20:875–877.
64. Hoke CH Jr, Snyder CE Jr. History of the restoration of adenovirus type 4 and type 7 vaccine, live oral (Adenovirus Vaccine) in the context of the Department of Defense acquisition system. Vaccine. 2013; 31:1623–1632.
65. Potter RN, Cantrell JA, Mallak CT, Gaydos JC. Adenovirus-associated deaths in US military during postvaccination period, 1999-2010. Emerg Infect Dis. 2012; 18:507–509.
66. Gray GC, Goswami PR, Malasig MD, Hawksworth AW, Trump DH, Ryan MA, Schnurr DP. Adult adenovirus infections: loss of orphaned vaccines precipitates military respiratory disease epidemics. For the Adenovirus Surveillance Group. Clin Infect Dis. 2000; 31:663–670.
67. Malarkey MA, Baylor NW. March 16, 2011 Approval Letter - Adenovirus Type 4 and Type 7 Vaccine, Live, Oral. Silver Spring: US Food and Drug Administration;accessed on 1 September 2014. Available at http://www.fda.gov/biologicsbloodvaccines/vaccines/approvedproducts/ucm247511.htm.
68. Heo JY, Kim HK, Cha YJ, Lee JE, Shim YS, Choe KW. A clinical features of severe adenovirus pneumonia among members of the Korea Military: a case series. Infect Chemother. 2012; 44:372–376.
69. Choe YJ, Park YJ, Jung C, Bae GR, Lee DH. National pertussis surveillance in South Korea 1955-2011: epidemiological and clinical trends. Int J Infect Dis. 2012; 16:e850–e854.
70. Armed Forces Health Surveillance Center (AFHSC). Pertussis diagnoses among service members and other beneficiaries of the U.S. Military Health System, January 2005-June 2012. MSMR. 2012; 19:14–17.
71. Grabenstein JD, Nevin RL. Mass immunization programs: principles and standards. Curr Top Microbiol Immunol. 2006; 304:31–51.
72. Chung EH. Vaccine allergies. Clin Exp Vaccine Res. 2014; 3:50–57.
73. Korea Centers for Disease Control and Prevention. Evaluation of national immunization registry, 2002-2010. accessed on 1 September 2014. Available at http://www.cdc.go.kr/CDC/info/CdcKrInfo0301.jsp?menuIds=HOME001-MNU1132-MNU1138-MNU0037-MNU1380&cid=12634.
74. Linkins RW. Immunization registries: progress and challenges in reaching the 2010 national objective. J Public Health Manag Pract. 2001; 7:67–74.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download