Abstract
The role of carcinoembryonic antigen (CEA) in pancreatic cancer remains poorly understood. Therefore, this study aimed to determine whether CEA is complementary to carbohydrate antigen 19-9 (CA19-9) in prognosis prediction after pancreatic cancer curative resection. We retrospectively reviewed records of 144 stage II curatively resected pancreatic cancer patients with preoperative and postoperative CEA and CA19-9 levels. Patients with normal preoperative CA19-9 were excluded. R0 resection margin, adjuvant treatment, and absence of angiolymphatic invasion were associated with better overall survival. There was no significant difference in median survival according to preoperative CEA levels. However, patients with normal postoperative CA19-9 (59.8 vs.16.2 months, P < 0.001) and CEA (29.4 vs. 9.3 months, P = 0.001) levels had longer overall survival than those with elevated levels. Among 76 patients with high postoperative CA19-9 levels, a better prognosis was observed in those with normal postoperative CEA levels than in those with elevated levels (19.1 vs. 9.3 months, P = 0.004). Postoperative CEA and CA19-9 levels are valuable prognostic markers in resected pancreatic cancer. Normal postoperative CEA levels indicate longer survival, even in patients with elevated postoperative CA19-9.
Pancreatic cancer is one of the most lethal solid tumors, in which surgical resection is the only potentially curative treatment method. However, only 10% to 20% of all patients receive a curative surgery (1, 2) while most experience recurrence due to occult extra-pancreatic metastasis at the time of diagnosis (3). Therefore, an accurate prediction of patients' prognosis after surgery is critical in preparation for the subsequent therapeutic plan.
Carbohydrate antigen 19-9 (CA19-9), first discovered in 1979 (4, 5), is the only serum biomarker widely accepted as a valuable diagnostic and prognostic marker in pancreatic cancer. Especially, recent studies have suggested that perioperative CA19-9 levels have prognostic impact (6, 7) and that normalization of postoperative CA19-9 levels is a strong prognostic factor in patients with resected pancreatic cancer (7, 8). However, CA19-9 level should be interpreted with caution due to the significance of its false positive and false negative rates.
Carcinoembryonic antigen (CEA), first detected in 1965 (9), has been commonly employed as a biomarker in colorectal cancer. Since elevated CEA level has been reported in more than 60% of patients with pancreatic ductal adenocarcinoma (10), a few studies have investigated its clinical significance in pancreatic cancer (11, 12, 13).
Despite a recent study demonstrating prognostic value of preoperative CEA level in pancreatic cancer (14), clinical value of postoperative CEA level in pancreatic cancer remains unclear. In the present study, we aimed to determine whether CEA has a complementary role to CA19-9 in predicting postoperative prognosis in patients with curatively resected pancreatic cancer.
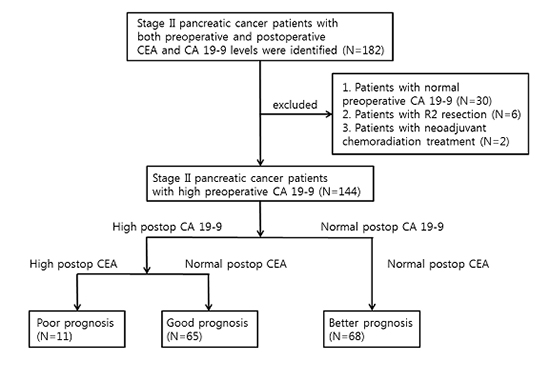
There were 206 pancreatic cancer patients who received curative, not palliative, surgery because of pancreatic ductal adenocarcinoma except other pancreatic tumors at Seoul National University Bundang Hospital from July 2003 to May 2012. Patients with stage II pancreatic cancer were 202 and 33 patients had preoperative normal CA 19-9 levels. There were 166 patients with R0 resection margin (80.6%), 34 patients with R1 resection margin (16.5%), and 6 patients with R2 resection margin (2.9%), respectively. Among 202 stage II pancreatic cancer patients, 182 with both preoperative and postoperative CEA and CA19-9 levels were identified. Within this group of patients, 38 were excluded from the present study due to normal preoperative CA19-9 level (n=30), residual tumor (n=6), and involvement of neoadjuvant chemoradiation therapy (n=2). Therefore, 144 stage II pancreatic cancer patients who received curative resection were eventually included in the present study.
Surgical procedures performed in this study involved pancreaticoduodenectomy with or without pyloric resection, distal pancreatectomy, and total pancreatectomy. Regional lymph node dissection was performed in all patients and pathological staging was decided according to the American Joint Committee on Cancer Staging Manual, seventh edition. R0 resection was defined as surgery with cancer-free margin and R1 resection as one with microscopic residual tumor. Because there is still lack of consensus about R0 and R1 resection in pancreatic cancer (15), we included R1 resection in curative resection in this study. In addition, angiolymphatic, venous and perineural invasion as well as pancreatic intraepithelial neoplasia (PanIN) of all specimens were reviewed.
Assessment of tumor marker levels was conducted by certified laboratories at each of the hospitals where patients received surgery. Preoperative CEA and CA19-9 levels were obtained within 1 month immediately prior to surgery while postoperative measurement was performed within 3 months from surgery date. Preoperative and postoperative liver function and CA19-9 levels were also assessed simultaneously. Reference ranges of tumor marker levels were 0-37 U/mL for CA19-9 and 0-5 ng/mL for CEA.
Kaplan-Meier analysis was used to generate survival curves and calculate median survival time. Overall survival according to each of the evaluated clinical characteristics was compared by log-rank test. Among the clinicopathological variables included in univariate Cox proportional hazards regression analysis, those with a two-sided P value of less than 0.15 were chosen for multivariate Cox proportional hazards regression analysis with stepwise selection. A two-sided P value of less than 0.05 was considered statistically significant. All statistical analyses were performed using SPSS statistics 21.0 software for Windows (IBM Corporation, Armonk, NY, USA).
Because of exclusion of 30 patients with normal preoperative CA19-9, we classified the patients according to postoperative tumor markers' level. As a result, the patients were classified into postoperative normal CA19-9 and CEA, high CA19-9 and normal CEA, and high CA19-9 and CEA. Baseline characteristics of the included patients are presented in Table 1. The median age was 64 yr and male patients accounted for 56.9% (82/144) of the patient cohort. The median preoperative and postoperative CA19-9 levels were 556.2 (56-20,000) and 41.3 (5-24,000) U/mL, respectively. A high postoperative CA19-9 level (>37 U/mL) was noted in 76 (52.8%) patients. Similarly, median preoperative and postoperative CEA levels were 2.9 (0.8-50.6) and 1.7 (0.3-21.8) ng/mL, respectively. Elevated preoperative and postoperative CEA levels (>5 ng/mL) were observed in 37 (25.7%) and 11 (7.6%) patients, respectively.
Ninety-six patients (66.7%) received adjuvant therapy that consisted of concurrent chemo-radiation therapy (54 patients, 37.5%), chemotherapy only (41 patients, 28.5%), or radiation therapy only (1 patient, 0.7%). About chemotherapy regimen, gemcitabine was most commonly used (55 patients, 38.2%) and 5-FU/leucovorin or capecitabine were also used as chemotherapy or chemoradiation therapy.
Among variable clinical factors, angiolymphatic and perineural invasion rates were significantly high in patients with normal CA19-9 and CEA levels; however, R1 resection rate was significantly high in patient with high CA19-9 and CEA level. Recurrence occurred in 70.1% of all patients, and the median recurrence-free survival time was 10.1 months. The median overall survival time was 27.1 months, and the 5-yr survival rate was 28.4%. Eventually, median recurrence free survival and overall survival were significantly longer in patients with normal CA19-9 and CEA and those were significantly shorter in patients with high CA19-9 and CEA.
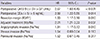
Besides the tumor markers of interest, various other clinico-pathological factors potentially affecting overall survival were analyzed. As a result, preoperative CEA levels were not associated with overall survival. However, normal postoperative CA19-9 and CEA levels were associated with better overall survival (Fig. 1). In addition, R0 resection, adjuvant treatment, and angiolymphatic and venous invasion were significantly associated with overall survival by univariate Cox regression analysis (Table 2). Perineural invasion also showed a trend towards association with overall survival with borderline significance (P=0.055). Among these factors, postoperative CA19-9 and CEA levels, R0 resection, adjuvant treatment, and angiolymphatic invasion were significantly associated with overall survival by multivariate Cox regression analysis (Table 3).
Patients' prognosis was assessed considering both CEA and CA19-9 levels in combination. However, none of the included patients had a normal postoperative CA19-9 level but a high CEA level. Median survival time of those with normal postoperative CEA and CA19-9 levels was excellent at 59.8 months (Fig. 2). Among the 76 patients with high postoperative CA19-9 levels, those with normal postoperative CEA levels had better prognosis than those with high postoperative CEA levels (19.1 months vs. 9.3 months, P=0.004) (Fig. 2).
Although CA19-9 is commonly employed as a serum prognostic biomarker in pancreatic cancer, limitations exist due to its false positivity and negativity reported in some clinical situations (16). Therefore, many researchers have sought to develop a novel biomarker for better prediction of pancreatic cancer prognosis, unfortunately, with little success. Unlike CA19-9, CEA is a far less common biomarker in pancreatic cancer due to its lower sensitivity and specificity reported for pancreatic cancer diagnosis (17, 18). On the other hand, regarding CEA's prognostic role in pancreatic cancer, literature is scarce with only a few available studies showing that high preoperative and postoperative CEA levels (11) or the preoperative CEA level alone was statistically associated with poor prognosis (13, 14, 19). Therefore, we focused on the possibility of CEA as a complementary prognostic biomarker to CA19-9 because elevated CEA levels were reported in up to 60% of patients with pancreatic cancer and it was previously considered a biomarker for the disease prior to the establishment of CA19-9 (17, 20). Our data suggested that postoperative CEA and CA19-9 levels combined may serve as a good prognostic marker in resected pancreatic cancer and that the postoperative CEA level might play a complementary role in the prediction of long-term outcomes in pancreatic cancer patients with elevated postoperative CA19-9 levels.
Recently, the clinical significance of perioperative CA19-9 levels in patients with resectable pancreatic cancer has been established with the preoperative CA19-9 level being correlated with tumor burden (21) and a normal postoperative CA19-9 level indicating a good prognosis, similar to our results (6, 21, 22). However, when patients have high levels of CA19-9 after curative resection, few biomarkers are available to predict long-term prognosis. Therefore, the present study was designed to verify the potential value of CEA in such scenario. In our study, the median survival time in patients with normal postoperative CEA/high CA19-9 levels was twice as long as that in patients with high CEA/high CA19-9 levels. This suggested that CEA might be an adjunctive prognostic indicator in resected pancreatic cancer patients with high postoperative CA19-9 levels. Moreover, it is important to note that the postoperative CEA level could be a valuable prognostic marker in pancreatic cancer patients with high postoperative CA19-9 levels, even after complete resection. To the best of our knowledge, our study is the first report on this topic.
Limitations to the present study include its retrospective design. Therefore, a selection bias of excluding patients without perioperative CEA or CA19-9 data was unavoidable. Moreover, we excluded 30 patients with normal preoperative CA19-9 because there only 3 patients with preoperative high CEA, which is too small to assess the role. In addition, no patient with a high postoperative CEA level and normal postoperative CA19-9 level was included. As a result, we could not demonstrate the discriminative role of CEA in patients with normal postoperative CA19-9 levels.
In conclusion, postoperative CEA and CA19-9 levels serve as valuable prognostic biomarkers in pancreatic cancer patients receiving curative surgery. In addition, the normal postoperative CEA level could play a role in discriminating patient's prognosis, even in those with elevated postoperative CA19-9 levels.
Figures and Tables
 | Fig. 1Kaplan-Meier analysis of overall survival according to postoperative carbohydrate antigen 19-9 (CA19-9) and carcinoembryonic antigen (CEA) levels. (A) The postoperative CA19-9 level is significantly associated with overall survival in patients with curatively resected stage II pancreatic cancer. The median overall survival time was 59.8 months in patients with normal CA19-9 levels and 16.2 months in those with high CA19-9 levels. (B) The postoperative CEA level is also significantly associated with overall survival in patients with curatively resected stage II pancreatic cancer. The median overall survival time in patients with normal and high CEA levels was 29.4 and 9.3 months, respectively. |
 | Fig. 2Kaplan-Meier analysis of overall survival according to postoperative levels of both carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9 (CA19-9). The median survival of patients with normal postoperative CEA and CA19-9 levels was excellent at 59.8 months. Among the 76 patients with high postoperative CA19-9 levels, those with normal postoperative CEA levels had better overall survival than those with high CEA levels (19.1 [normal CEA/high CA19-9] vs. 9.3 months [high CEA/highCA19-9]) (*P < 0.001; †P = 0.004). |
Table 1
Baseline characteristics of patients

Table 2
Univariate Cox regression analysis of overall survival
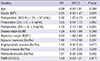
Table 3
Multivariate Cox regression analysis of overall survival
ACKNOWLEDGMENTS
The authors thank Division of Statistics in Medical Research Collaborating Center at Seoul National University Bundang Hospital for statistical analyses.
References
1. Sener SF, Fremgen A, Menck HR, Winchester DP. Pancreatic cancer: a report of treatment and survival trends for 100,313 patients diagnosed from 1985-1995, using the National Cancer Database. J Am Coll Surg. 1999; 189:1–7.
2. Conlon KC, Klimstra DS, Brennan MF. Long-term survival after curative resection for pancreatic ductal adenocarcinoma. Clinicopathologic analysis of 5-year survivors. Ann Surg. 1996; 223:273–279.
3. Butturini G, Stocken DD, Wente MN, Jeekel H, Klinkenbijl JH, Bakkevold KE, Takada T, Amano H, Dervenis C, Bassi C, et al. Pancreatic Cancer Meta-Analysis Group. Influence of resection margins and treatment on survival in patients with pancreatic cancer: meta-analysis of randomized controlled trials. Arch Surg. 2008; 143:75–83.
4. Koprowski H, Steplewski Z, Mitchell K, Herlyn M, Herlyn D, Fuhrer P. Colorectal carcinoma antigens detected by hybridoma antibodies. Somatic Cell Genet. 1979; 5:957–971.
5. Koprowski H, Herlyn M, Steplewski Z, Sears HF. Specific antigen in serum of patients with colon carcinoma. Science. 1981; 212:53–55.
6. Hata S, Sakamoto Y, Yamamoto Y, Nara S, Esaki M, Shimada K, Kosuge T. Prognostic impact of postoperative serum CA 19-9 levels in patients with resectable pancreatic cancer. Ann Surg Oncol. 2012; 19:636–641.
7. Humphris JL, Chang DK, Johns AL, Scarlett CJ, Pajic M, Jones MD, Colvin EK, Nagrial A, Chin VT, Chantrill LA, et al. NSW Pancreatic Cancer Network. The prognostic and predictive value of serum CA19.9 in pancreatic cancer. Ann Oncol. 2012; 23:1713–1722.
8. Motoi F, Rikiyama T, Katayose Y, Egawa S, Unno M. Retrospective evaluation of the influence of postoperative tumor marker status on survival and patterns of recurrence after surgery for pancreatic cancer based on RECIST guidelines. Ann Surg Oncol. 2011; 18:371–379.
9. Gold P, Freedman SO. Specific carcinoembryonic antigens of the human digestive system. J Exp Med. 1965; 122:467–481.
10. Satake K, Kanazawa G, Kho I, Chung Y, Umeyama K. Evaluation of serum pancreatic enzymes, carbohydrate antigen 19-9, and carcinoembryonic antigen in various pancreatic diseases. Am J Gastroenterol. 1985; 80:630–636.
11. Yasue M, Sakamoto J, Teramukai S, Morimoto T, Yasui K, Kuno N, Kurimoto K, Ohashi Y. Prognostic values of preoperative and postoperative CEA and CA19.9 levels in pancreatic cancer. Pancreas. 1994; 9:735–740.
12. Zamcheck N. The present status of carcinoembryonic antigen (CEA) in diagnosis, detection of recurrence, prognosis and evaluation of therapy of colonic and pancreatic cancer. Clin Gastroenterol. 1976; 5:625–638.
13. Ni XG, Bai XF, Mao YL, Shao YF, Wu JX, Shan Y, Wang CF, Wang J, Tian YT, Liu Q, et al. The clinical value of serum CEA, CA19-9, and CA242 in the diagnosis and prognosis of pancreatic cancer. Eur J Surg Oncol. 2005; 31:164–169.
14. Distler M, Rückert F, Hunger M, Kersting S, Pilarsky C, Saeger HD, Grützmann R. Evaluation of survival in patients after pancreatic head resection for ductal adenocarcinoma. BMC Surg. 2013; 13:12.
15. Schlitter AM, Esposito I. Definition of microscopic tumor clearance (r0) in pancreatic cancer resections. Cancers (Basel). 2010; 2:2001–2010.
16. Kim BJ, Lee KT, Moon TG, Kang P, Lee JK, Kim JJ, Rhee JC. How do we interpret an elevated carbohydrate antigen 19-9 level in asymptomatic subjects? Dig Liver Dis. 2009; 41:364–369.
17. Podolsky DK. Serologic markers in the diagnosis and management of pancreatic carcinoma. World J Surg. 1984; 8:822–830.
18. Herlyn M, Sears HF, Steplewski Z, Koprowski H. Monoclonal antibody detection of a circulating tumor-associated antigen. I. Presence of antigen in sera of patients with colorectal, gastric, and pancreatic carcinoma. J Clin Immunol. 1982; 2:135–140.
19. Tsavaris N, Kosmas C, Papadoniou N, Kopterides P, Tsigritis K, Dokou A, Sarantonis J, Skopelitis H, Tzivras M, Gennatas K, et al. CEA and CA-19.9 serum tumor markers as prognostic factors in patients with locally advanced (unresectable) or metastatic pancreatic adenocarcinoma: a retrospective analysis. J Chemother. 2009; 21:673–680.
20. Lundin J, Roberts PJ, Kuusela P, Haglund C. The prognostic value of preoperative serum levels of CA 19-9 and CEA in patients with pancreatic cancer. Br J Cancer. 1994; 69:515–519.
21. Ferrone CR, Finkelstein DM, Thayer SP, Muzikansky A, Fernandez-delCastillo C, Warshaw AL. Perioperative CA19-9 levels can predict stage and survival in patients with resectable pancreatic adenocarcinoma. J Clin Oncol. 2006; 24:2897–2902.
22. Montgomery RC, Hoffman JP, Riley LB, Rogatko A, Ridge JA, Eisenberg BL. Prediction of recurrence and survival by post-resection CA 19-9 values in patients with adenocarcinoma of the pancreas. Ann Surg Oncol. 1997; 4:551–556.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download