1. Riggs B, Melton LJ 3rd. Involutional osteoporosis. N Engl J Med. 1986; 314:1676.
2. Melton LJ 3rd. Epidemiology of spinal osteoporosis. Spine (Phila Pa 1976). 1997; 22:2S.
3. Rowe SM, Chung JY, Yoon TR, Lee JJ, BBae BH, Choi J. An epidomiological study of hip fracture: A comparison between 1991 and 2001. Korean J Bone Metab. 2003; 10:109.
4. Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine (Phila Pa 1976). 2000; 25:923–928.
5. Patel U, Skingle S, Campbell GA, Crisp AJ, Boyle IT. Clinical profile of acute vertebral compression fractures in osteoporosis. Br J Rheumatol. 1991; 30:418–421.
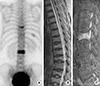
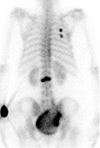
6. Jun DS, Shin WJ, Kim KH. The usefulness of bone scan in the osteoporotic vertebral compression fracture patients treated with kyphoplasty. J Korean Soc Spine Surg. 2008; 15:18–22.
7. Jones G, Nguyen T, Sambrook PN, Kelly PJ, Gilbert C, Eisman JA. Symptomatic fracture incidence in elderly men and women: the Dubbo Osteoporosis Epidemiology Study (DOES). Osteoporos Int. 1994; 4:277–282.
8. Barrett-Connor E, Nielson CM, Orwoll E, Bauer DC, Cauley JA. Epidemiology of rib fractures in older men: Osteoporotic Fractures in Men (MrOS) prospective cohort study. BMJ. 2010; 340:c1069.
9. Freedman BA, Potter BK, Nesti LJ, Giuliani JR, Hampton C, Kuklo TR. Osteoporosis and vertebral compression fractures-continued missed opportunities. Spine J. 2008; 8:756–762.
10. Maynard AS, Jensen ME, Schweickert PA, Marx WF, Short JG, Kallmes DF. Value of bone scan imaging in predicting pain relief from percutaneous vertebroplasty in osteoporotic vertebral fractures. AJNR Am J Neuroradiol. 2000; 21:1807–1812.
11. Sontag A, Krege JH. First fractures among postmenopausal women with osteoporosis. J Bone Miner Metab. 2010; 28:485–488.
12. Siris ES, Brenneman SK, Barrett-Connor E, Miller PD, Sajjan S, Berger ML, Chen YT. The effect of age and bone mineral density on the absolute, excess, and relative risk of fracture in postmenopausal women aged 50-99: results from the National Osteoporosis Risk Assessment (NORA). Osteoporos Int. 2006; 17:565–574.
13. DeLuca SA, Rhea JT, O'Malley TO. Radiographic evaluation of rib fractures. AJR Am J Roentgenol. 1982; 138:91–92.
14. Nevitt MC, Cummings SR, Browner WS, Seeley DG, Cauley JA, Vogt TM, Black DM. The accuracy of self-report of fractures in elderly women: evidence from a prospective study. Am J Epidemiol. 1992; 135:490–499.
15. Hurley ME, Keye GD, Hamilton S. Is ultrasound really helpful in the detection of rib fractures? Injury. 2004; 35:562–566.
16. Batillas J, Vasilas A, Pizzi WF, Gokcebay T. Bone scanning in the detection of occult fractures. J Trauma. 1981; 21:564–569.
17. Ludwig H, Kumpan W, Sinzinger H. Radiography and bone scintigraphy in multiple myeloma: a comparative analysis. Br J Radiol. 1982; 55:173–181.
18. Spiegl UJ, Beisse R, Hauck S, Grillhösl A, Bühren V. Value of MRI imaging prior to a kyphoplasty for osteoporotic insufficiency fractures. Eur Spine J. 2009; 18:1287–1292.
19. Delmas PD, van de Langerijt L, Watts NB, Eastell R, Genant H, Grauer A, Cahall DL. Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res. 2005; 20:557–563.
20. Sterling JC, Webb RF Jr, Meyers MC, Calvo RD. False negative bone scan in a female runner. Med Sci Sports Exerc. 1993; 25:179–185.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download