Abstract
Occupational diseases may be defined only medically or scientifically, and even then, their definition is not simple. However, compensable occupational diseases involve the additional layer of legal systems and social welfare policies as well. Their multifaceted nature makes determining the work-relatedness of these diseases more complex. Korea has established standards for the recognition of occupational diseases in Schedule 5 of the Enforcement Decree of the Labor Standards Act, and specific criteria for the recognition of occupational diseases are listed in Schedule 3 of the Enforcement Decree of the Industrial Accident Compensation Insurance Act. The new list of compensable occupational diseases comprises 13 articles as an open-ended system. The newly added articles pertain to lymphohematopoietic (Article 5) and infectious diseases (Article 9), as well as diseases of other target organs. Furthermore, the article on liver diseases (Article 8) has been partially revised. The new act has been changed to clarify the meaning as it has been presented in recent research. It is necessary to achieve agreement among concerned parties, including experts from the legal, medical, and social domains to resolve the issues of work-relatedness, causation, notion of aggravation, and so on for preparing a list and a process that are more reasonable.
Occupational diseases (ODs) can be defined only medically or scientifically. However, compensable ODs are within the purview of the legal system and are related to social welfare policies irrespective of the presence of scientific evidence. Therefore, compensable OD lists vary depending on the country and the prevailing social context therein. Korea stipulates OD recognition standards in Schedule 5 of the Enforcement Decree (ED) of the Labor Standards Act (ED-LSA) [1], and specific criteria for OD recognition are listed in Schedule 3 of the Enforcement Decree of the Industrial Accident Compensation Insurance Act (ED-IACIA) [2]. The previous ED-IACIA disease list comprised 23 articles covering diseases related to 4 target organ systems [occupational skin (Article 22), liver (Article 23), cerebro-cardiovascular (Article 1), and vascular and musculoskeletal (Article 2)], 3 comprehensive agents [chemical (Article 7), physical (Article 3), and biological (Article 21)], and 16 single or groups of agents [vibration, benzene, vinyl chloride (VC), etc.] [3]. The new compensation list comprises 13 articles, including Article 13 [other diseases] and is an open-ended system. The newly added articles are related to the respiratory system (Article 3), neurological and mental diseases (Article 4), the lymph and hematopoietic system (Article 5), diseases of the eye and ear (Article 7), and infectious diseases (Article 9). The articles related to skin (Article 6) and liver diseases (Article 8) have been partially revised. A new article on occupational cancers (Article 10) has been added. Most single agents have been integrated into Article 13 (diseases caused by acute intoxication and chemicals) and have been moved to the relevant target organ systems. This article describes the contents of and the reasons for changes related to occupational hematologic, liver, and infectious diseases based on current knowledge, and it includes a few comments outlining the direction of future research and revisions.
The procedure for amending the specific OD recognition criteria in ED-IACIA and ED-LSA was described by Song et al. (4). The authors reviewed the scope of compensable ODs in the LSA (1) and the IACIA (2). To search for newly developed cases, we investigated several sources such as the compensation data of The Korea Workers' Compensation and Welfare Service (COMWEL), Specific Medical Examination for Workers (SME), OD surveillance system, and case reports and investigations from scientific journals (5) and other related websites such as that of the Korea Occupational Safety and Health Agency (KOSHA).
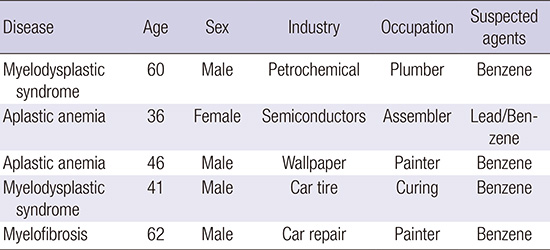
Occupational hematologic diseases include those of blood cell survival (hemoglobin denaturation and hemolysis), metabolism (porphyria), formation (aplasia), morphology and function (preleukemias and leukemias), or coagulation (thrombocytopenia)" [6]. There are various hematologic toxicants such as heavy metals (lead, mercury, etc.) and organic solvents (benzene, toluene, xylene, etc.). However, in this report, the authors deal only with diseases caused by benzene and inorganic lead and its compounds because these are the only two agents described under lymphohematopoietic diseases in Article 5 of ED-IACIA. In addition, the authors exclude lymphohematologic cancers because the category of malignant neoplasms is newly created and is described separately in the ED-IACIA. However, the authors describe myelodysplastic syndrome and aplastic anemia because they regard these not as cancers but as precancerous diseases without metastatic potential. Several cases of these diseases are described in the KOSHA casebook [7] (Table 1).
The description of hematologic diseases in Article 5 is new. However, in terms of its content, the description has been reorganized from two chemical agents, i.e., benzene and lead and its compounds (except organic lead), which were described as separate articles in the old ED-IACIA. The new Article 5 describes only these two agents and their hematologic toxicity (Table 2).
Benzene (C6H6), the prototypical aromatic hydrocarbon, is a clear, colorless, volatile liquid with a rather pleasant odor. Benzene is generated in the coal gasification, coke production, petrochemicals, and petroleum-refining industries. Further, toluene, thinners, and other organic solvent-based chemicals can contain benzene as an impurity. Occupational exposure to benzene is known to cause various hematologic abnormalities ranging from anemia to leukemia and other cancerous diseases. There are many reports and sources of lymphohematopoietic cancers [8]. However, reports of non-cancerous or precancerous diseases are rare, although there are a few reports of aplastic anemia, myelodysplastic syndrome, and multiple myeloma [9].
To make legal changes, the article about the role of benzene in blood diseases was reviewed in terms of 1) the reorganization of the law concerning the creation of occupational cancers, 2) the review of the previously described exposure level, and 3) the consideration of non-cancerous diseases due to a non-occupational origin.
Previously, benzene was listed as a toxicant for cases of non-cancerous lymphohematologic (anemia, leukopenia, thrombocytopenia, and pancytopenia), skin (acute or chronic dermatitis), precancerous, and cancerous diseases (leukemia, myelodysplastic syndrome, multiple myeloma, and aplastic anemia) independently. The article stated its acute toxic effects (headache, dizziness, vomiting, etc. due to massive benzene vapor inhalation) (Table 2).
However, as described earlier, the legal system has been changed as follows: the inclusion of occupational cancers (Article 10), reclassification of chemicals into target organ-related diseases, and introduction of the new Article 11 about the acute toxic effects of chemicals. The diseases caused by benzene are classified as skin diseases and cancer due to benzene. Leukemia and multiple myeloma caused by benzene exposure were moved to the occupational cancer section.
Although myelodysplastic syndrome and aplastic anemia can be classified as occupational cancers, the authors regarded them as precancerous or non-cancerous conditions because of their non-metastatic nature. Additionally, the authors changed the Korean nomenclature of "aplastic anemia" to reflect the latest diagnosis. "Acute or chronic dermatitis" was changed to "contact dermatitis", and this clause was moved to the section on skin diseases. As a result, the revises Article 5 describes only non-cancerous (anemia, leukopenia, thrombocytopenia, and pancytopenia) and precancerous hematologic (myelodysplastic syndrome and aplastic anemia) disorders.
The previous clause B of Article 10 lists the cumulative benzene exposure level as an approval criterion. However, it is difficult to determine the exact threshold of the benzene exposure level from the viewpoint of lymphohematopoietic (pre) cancer diseases due mainly to a shortage of scientific evidence. In this regard, thus far, the authors do not have definite scientific, rational evidence or research results to convince scientists or medical doctors. Furthermore, cancer has no threshold theoretically; this means that there is no dose criteria of benzene (other than zero) at which the risk of cancer is non-existent. Moreover, it is very difficult to measure exactly the past cumulative exposure doses for more than 10 yr [10]. Thus, the authors decided that the current level in the law should be retained to ensure that workers are not ineligible for compensation due to decisions based on strict criteria. In addition, the authors considered legal stability and decided to not change the current comprehensive provision. Furthermore, in Korea, compensation has been awarded in several cases of exposure to lower levels of benzene by considering no threshold for occupational cancers. Another change is the change in the cumulative dosage unit from ppm to ppm·year for further clarification. Finally, clause B in Article 5 excludes non-occupational causes.
Lead has been used widely to make statues, jewelry, water pipes, and drinking vessels because of its characteristics, malleability, and low melting point. Groups of workers mainly exposed to the risk of inorganic lead exposure are battery workers, cable makers/splicers, painters, pigment makers, ship burners, solderers, and so on. Inorganic lead is mainly characterized by hematologic, neurologic, renal, and reproductive toxicities. However, the toxicity of organic lead, principally tetraethyl lead (TEL), is limited largely to acute or subacute central nervous system effects.
In the article about blood disorders, the lead-related list has been changed slightly. Lead alloys were deleted because lead alloys can be considered lead compounds. Thus, "lead and its compounds (except organic lead)" was the final wording. Previously, medical conditions caused by lead as an agent included extensor muscle paralysis, chronic renal failure, blood lead level elevation (40 µg/100 mL or more lead in blood), acute toxicity, and anemia (Table 2). Similar to those of benzene, the toxic effects of lead and its compounds were redistributed to other appropriate articles such as neuro-psychological effects and acute toxicity due to chemicals. Thus, the hematological diseases clause lists only anemia caused by inorganic lead and its compounds. In addition, there is an exception list, and few changes have been made to this list. The existing entry is "anemia, but iron-deficiency anemia shall be excluded." The recently changed version of this list is "iron-deficiency anemia or other causes" with the addition of "other causes."
There are various occupational liver diseases such as hepatitis, cirrhosis, and even cancerous diseases caused by occupational conditions or agents. The liver is the target organ of various occupational chemicals such as heavy metals and organic solvents because of its main role in their metabolism and elimination. In addition, occupationally exposed biologic agents (bacterial and viral infections) and physical agents encountered in the workplace involve the hepatic system. The amended article lists toxic hepatitis from chemicals and cirrhosis due to VC. In Korea, viral hepatitis and toxic hepatitis caused by trichloroethylene (TCE) and dimethylformamide (DMF) are well known [11]. Thus, the authors mainly describe chemically induced toxic hepatitis such as that due to TCE and DMF, and liver cirrhosis due to VC. Viral hepatitis is listed separately in Article 9 of infectious diseases. According to COMWEL statistics, 2 cases of viral hepatitis were reported in 2008 but none in 2007 and 2010 [12].
Under the previous law, occupational hepatic disorders included toxic hepatitis, acute hepatitis, fulminant hepatitis, liver abscess, chronic hepatitis, cirrhosis, and primary liver cancer. Liver cancer was moved to the occupational cancers item, and pathogen (bacteria, virus, etc.) infection and superinfection caused occupationally by other types of viral hepatitis were reclassified as infectious diseases. Fulminant hepatitis and abscesses were considered secondary diseases from other toxic or viral hepatitis, so the authors delisted these diseases. Thus, the amended list contains only toxic hepatitis caused by TCE, DMF, etc., and liver cirrhosis due to VC. TCE was moved from the previous agent list, and DMF was added due to the recent cases of toxicity in Korea (Table 3).
TCE is a colorless, non-flammable liquid with a pleasant odor. In the past, TCE was used for vapor degreasing and as a solvent. In Korea, several toxic hepatitis cases [13, 14, 15] were reported to be caused by TCE. Most of these cases are of the Steven-Johnson syndrome or skin problems, as well as abnormal liver functions. A few workers have died due to TCE exposure. Toxic hepatitis occurs in workers exposed to DMF, a colorless, water-soluble liquid with a faint ammonia-like odor. It is used as a solvent, particularly for resins and polar polymers, and for producing synthetic fibers or synthetic leather. Several cases of DMF toxicity have been reported in Korea [16, 17]. Furthermore, chemical hepatitis should first be ruled out over other possible causes such as drugs, alcohol, excess weight, and diabetes. These restrictions are the same as those in the old ED-IACIA.
The list of "cirrhosis" due to VC has been changed from "hepatosplenic syndrome (liver fibrosis, splenomegaly, thrombocytopenia, etc.)." However, the controversy [18, 19, 20] remains despite a few reports that VC probably causes liver fibrosis and cirrhosis [21, 22]. VC probably causes hemangiosarcoma and possibly hepatocellular cancers [23]. The list of "existing liver diseases, caused by occupational accidents or hazardous substances, and their natural progress are more aggravated than expected and the worse is medically accepted" was left unchanged.
Occupational infections are diseases caused by work-associated exposure to microbial agents, including bacteria, viruses, fungi, and parasites. An infection is distinguished as an OD by some aspect of work that involves contact with a biologically active organism. Occupational infection can occur following contact with infected persons or surfaces, as in the case of healthcare workers; with infected animal or human tissue, secretions, or excretions, as in the case of laboratory workers; with asymptomatic or unknown contagious humans, as may happen during business travel; or with infected animals, as in the case of agriculture [24]. The amended list contains minor changes, although the category of infected diseases was newly added.
In Korea, the known at-risk populations are workers from healthcare, agriculture, forestry, fishery, and others, and "According to annual reports published from 1999 to 2007, 55,120 cases of work-related illnesses, including 10,619 cases of OD and 44,501 cases of work-related disorders, were documented. Occupational infection (851 cases, including 22 deaths) comprised 8.0% of all ODs and 1.5% of work-related illnesses in this period. Occupational infection was found to be the third most common OD" [25]. The proportion of infectious diseases was 11.7% (2008), 17.3% (2010), and 14.2% (2012) of all ODs (26) (Table 4). The considered anthropods mainly include tsutsugamushi, and viral hepatitis was reported in 5 cases in 2008, 13 cases in 2010, and 4 cases in (2012) [12].
Infectious diseases have various biological causes and affect a number of target organs; they occur in many industries or occupations. In Korea, the at-risk populations are workers from healthcare, agriculture, forestry, fishery, and others [25], and these industries are not very different from those in other countries. The amended list has minor changes, although the category of target organs was newly introduced. In the case of viral hepatitis, healthcare workers are particularly at risk for HBV and HCV infections. The reported cases occurred in nurses, doctors, and pathology technicians in Korea, and the main cause of occurrence was accidental needlestick injuries [11].
In the recent legal system, infectious diseases as well as the corresponding target organ systems such as lung, neuropsychologic, and occupational cancer systems were introduced. However, in terms of the contents, very few changes were made. As a result, the list of occupational infections is mostly similar to the old Article 21 describing diseases caused by pathogens (Table 5). The previous Article 21 contains the descriptions of pathogen contact, sufficient latent period, and pathogen confirmation, but it has been deleted because the regulations might be strict.
Second, the strict classification defining "B. Infection for non-healthcare workers" has been changed too. Diseases such as leptospirosis and tsutsugamushi could occur in healthcare workers as well; thus, the classification was deleted for simplifying the described regulations. However, the previously listed diseases have been retained. Third, the authors added a list of laboratory workers or other workers who are at a high risk of infection from directly dealing with or being exposed to pathogens because of their occupation.
Two minor changes should be addressed. Epidemic hemorrhagic fever has been replaced with "hemorrhagic fever with renal syndrome," the official term used by Korea Centers for Disease Control and Prevention. Furthermore, the Korean names of anthrax and legionella have been changed for the same reason. Because of the new classification system that includes organ systems, it is necessary to understand that the old article on skin disease (Article 22) and one item of chemical agents (Article 7) included pathogen-containing items, and these items are described in the article on diseases of the skin or other appropriate organs.
Various types of chemicals such as organic solvents and heavy metals have been used in the manufacturing industry. OD could occur under various working conditions if psychosocial and ergonomic risk factors, as well as harmful or hazardous materials, are considered. The diseases are reported through various methods such as "compensation by the IACI," special health examination, and OD surveillance [5]. One of main issues would be to determine work-relatedness from the medical and legal perspectives.
Above all, in the process of assessing work-relatedness, causation could be the basic and essential point [27]. The causal problem is one of the main issues in philosophy since ancient Greece. In the medical or public health area, epidemiology mainly deals with causation or causality issues. Greenland deals with various causation-related issues such as skepticism about observational studies, relationship association with causation, confounding and effect modification, causes, Popperian philosophy in epidemiology, and advancements in theoretical and quantitative methods [28]. Above all, the core of these issues will be the "Can we determine the causation? If yes, then how?" The uncertainty of scientific evidence will continue, and the legal adaptation of scientific evidences could be an even more complex problem [29].
Another issue is the estimation of the (cumulative) exposure level in the case of benzene-induced myelodysplastic syndrome or aplastic anemia. These pre- or non-cancerous diseases are mainly related to cancers and other ODs. Chemical carcinogenesis involves several issues: the carcinogen, latency of individual cancers, exposure estimation, etc. [9]. This is far more complex for cases of cancer than those of accident and acute intoxication. In particular, it is very difficult to estimate the past cumulative exposure dose despite the suggestion of several solutions to this end.
Currently, the causation relationship between VC and cirrhosis remains a controversial topic of debate [18, 19, 20]. The causal relationship between VC and hepatocelluar cancers, too, remains [23]. Further research is necessary in the medical or scientific areas, but other considerations are needed to include these ODs in the list of legally compensable diseases in Korea. Legal compensation warrants the consideration of a greater number of variables such as interests and conflicts of related parties, social welfare and its related economic status, and scientific evidence.
Fourth is the "aggravation" issue. It deals with our consideration of the term aggravation in "their natural progress is more aggravated than expected and the worse is medically accepted" in Article 8, Liver diseases. We need to know precisely the natural course of these diseases. However, the natural courses of individual diseases remain unclear. The issue complexifies when considering other variables such as age, sex, genetic factors, occupationally exposed materials, and different patient exposure patterns in individual cases. Moreover, aggravation could imply a causal consequence due to the shortening of the induction period [30], and ED-IACIA contains this premise.
As mentioned earlier, the entire process of determining work-relatedness includes various concepts from legal, epidemiological, and medical specialties. However, most medical doctors have almost no opportunity to acquire such knowledge and training. Therefore, a systematic training process on the medical, epidemiologic, even legal aspects of compensation was demanded for securing at least the validity of approval and consistency.
Figures and Tables
Table 2
The old and the new comparison for lymphohematopoietic disease (not official, and partially translated)

Table 3
The old and the new comparison for the liver disease (not official, and partially translated)

References
1. Enforcement Decree of the Labor Standards Act of the Republic of Korea, Presidential Decree No. 24652, (28 June 2013), Seoul, 2013. accessed on 27 December 2013. Available at http://www.lawnb.com/lawinfo/contents_view.asp?cid=20FE34414D0A4563A8507112C4D62FB6|0|K.
2. Enforcement Decree of the Industrial Accident Compensation Insurance Act of the Republic of Korea, Presidential Decree No. 24651 (18 June 2013), Seoul, 2013. accessed on 27 December 2013. Available at http://www.lawnb.com/lawinfo/contents_view.asp?cid=4375FD37B4024C389F28EC2C889B1560|0|K.
3. Enforcement Decree of the Industrial Accident Compensation Insurance Act of the Republic of Korea, Presidential Decree No. 22101 (26 Mar 2010), Seoul, 2013. Available at http://www.lawnb.com/lawinfo/link_view.asp?cid=AA14082DC565417CA4872C0592886932|N.
4. Song J, Kim I, Choi BS. The scope and specific criteria of compensation for occupational diseases in Korea. J Korean Med Sci. 2014; 29:S32–S39.
5. Kang SK, Kim EA. Occupational diseases in Korea. J Korean Med Sci. 2010; 25:S4–S12.
6. Navarro WH, Rugo HS. Occupational Hematology. In : Ladou J, editor. Current occupational & environmental medicine. 4th ed. California: McGraw-Hill;2007. p. 208–223.
7. Park JS. Occupational diseases' casebook-2011. Incheon, Korea: Occupational Safety and Health Research Institute, Korea Occupational Safety and Health Agency;2012. accessed on 1 December 2013. Available at http://safedu.org/pds1/23678.
8. Kim EA, Lee WJ, Son MA, Kang SK. Occupational lymphohematopoietic Cancer in Korea. J Korean Med Sci. 2010; 25:S99–S104.
9. Kang SK, Ahn YS, Chung HK. Occupational cancer in Korea in the 1990s. Korean J Occup Environ Med. 2001; 13:351–359.
10. Kim JW. Development on specialists' guide book for medical examination and diagnosis of occupational diseases: occupational cancers. Incheon, Korea: Occupational Safety and Health Research Institute, Korea Occupational Safety and Health Agency;2012. 186–221. accessed on 1 December 2013. Available at http://oshri.kosha.or.kr/bridge?menuId=901.
11. Kim HR, Kim TW. Occupational hepatic disorders in Korea. J Korean Med Sci. 2010; 25:S36–S40.
12. Statistics of Korea. Industrial accident cause statistics. accessed on 1 December 2013. Available at http://kosis.kr/common/meta_onedepth.jsp?vwcd=MT_OTITLE&listid=380_38001.
13. Chae HB, Kim JA, Lee KS, Park SM, Yoon TY, Yoon SJ. A case of hepatitis after occupational exposure of trichloroethylene. Korean J Hepatol. 1999; 5:59–64.
14. Hong DP, Kim JS, Kim SH, Kim JM, Lee ES. A case of toxic erythema, toxic hepatitis and exfoliative dermatitis due to trichloroethylene. Korean J Dermatol. 1985; 23:785–789.
15. Lee SW, Kim EA, Kim DS, Koh DH, Kang SK, Kim BK, Kim MK. Exposure level of trichloroethylene in Stevens-Johnson syndrome due to occupational exposure: 3 case reports and a review of other cases. Korean J Occup Environ Med. 2008; 20:132–146.
16. Kang SK, Jang JY, Rhee KY, Chung HK. A study on the liver dysfunction due to dimethylformamide. Korean J Occup Environ Med. 1991; 3:58–64.
17. Kim SK, Lee SJ, Chung KC. A suspicious case of dimethylformamide induced fulminant hepatitis in synthetic leather workers. Korean J Occup Environ Med. 1995; 7:186–190.
18. Frullanti E, La Vecchia C, Boffetta P, Zocchetti C. Vinyl chloride exposure and cirrhosis: a systematic review and meta-analysis. Dig Liver Dis. 2012; 44:775–779.
19. Mastrangelo G, Cegolon L, Fadda E, Fedeli U. Comment to "Vinyl chloride exposure and cirrhosis: a systematic review and meta-analysis". Dig Liver Dis. 2013; 45:701–702.
20. Frullanti E, La Vecchia C, Boffetta P, Zocchetti C. Authors' reply: Comment to "Vinyl chloride exposure and cirrhosis: a systematic review and meta-analysis". Dig Liver Dis. 2013; 45:702.
21. Maroni M, Mocci F, Visentin S, Preti G, Fanetti AC. Periportal fibrosis and other liver ultrasonography findings in vinyl chloride workers. Occup Environ Med. 2003; 60:60–65.
22. Hsiao TJ, Wang JD, Yang PM, Yang PC, Cheng TJ. Liver fibrosis in asymptomatic polyvinyl chloride workers. J Occup Environ Med. 2004; 46:962–966.
23. Creech JL Jr, Johnson MN. Angiosarcoma of liver in the manufacture of polyvinyl chloride. J Occup Med. 1974; 16:150–151.
24. Takahashi K, Fujimoto G. Occupational Infections. In : Ladou J, editor. Current occupational & environmental medicine. 4th ed. California: McGraw-Hill;2007. p. 262–279.
25. Chung YK, Ahn YS, Jeong JS. Occupational infection in Korea. J Korean Med Sci. 2010; 25:S53–S61.
26. Park JS. The report on work-related accident cause summary (occupational diseases) in 2012. Incheon, Korea: Occupational Safety and Health Research Institute, Korea Occupational Safety and Health Agency;2013. p. 47–72.
27. Kim JW. Epidemiology and causation. Kosin Med J. 2013; 28:87–97.
28. Greenland S. Evolution of epidemiologic ideas: annotated readings on concepts and methods. 1st ed. Massachusetts: Epidemiology Resources Inc;1987.
29. Michaels D. Scientific evidence and public policy. Am J Public Health. 2005; 95:S5–S7.
30. Rothman KJ, Greenland S, Poole C, Lash TL. Causation and causal inference. In : Rothman KJ, Lash TL, Greenland S, editors. Modern epidemiology. 3rd ed. Philadelphia: Lippincott Williams & Wilkins;2012. p. 5–31.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download