INTRODUCTION
Neurological disorders are disorders of the central and peripheral nervous systems. Functional or structural abnormalities in the brain, spinal cord, or other nerves can cause these disorders. The World Health Organization (WHO) determined that neurological disorders affected about one billion people worldwide in 2006 (
1). Although the central nervous system (CNS), which consists of the brain and the spinal cord, is protected by bones and a blood-brain barrier, it is very susceptible to physical and chemical damage. The peripheral nervous system (PNS) including neurons, the neural networks, and nerves is vulnerable to chemical and structural damage. The classification of neurological disorders is given in "Chapter VI: Diseases of the nervous system" of the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) by the WHO (
2). Occupational neurological disorders (ONDs) can be defined as the neurological disorders that are caused or aggravated by occupational exposure including physical and chemical agents.
Mental disorders are defined by a combination of emotions, actions, thoughts, and perceptions. Although the standard criteria are widely used, the definition, assessment, and classification of mental disorders are still variable. Over a third of the people in most countries are estimated to meet the diagnostic criteria for mental disorders (
3). The classification of the mental disorders is given in "Chapter V: Mental and behavioral disorders" of the ICD-10 by the WHO (
2), and the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (or DSM-V since May 2013) by the American Psychiatric Association. Occupational mental disorders (OMDs) can be defined by the mental disorders that are caused or aggravated by occupational exposure including physical agents, chemical agents, and psychological stressors.
The standards for the recognition of occupational diseases (ODs) were originally defined in the Established Rule of the Ministry of Labor (MOL). Then, the standards were moved to and called the Enforcement Rules of the Industrial Accident Compensation Insurance (ER-IACI) Act in 1994. Although the IACI Act was revised several times until 2008, there was not much change when compared to the first version of the ER-IACI Act. Because the standards were based on hazardous agents, clinicians excluding occupational physicians acquainted with disease nomenclature were not familiar with the occupational compensation system. Further, there were no psychiatric diseases in the list of diseases in the standards. These problems made Korean neurologists and psychiatrists feel that the occupational disease compensation was not their work area. The amendment of the Enforcement Decree of IACI Act (ED-IACIA) in 2013 introduced significant changes in the standards for the recognition of ODs including ONDs and OMDs in Korea. In this article, we outline the history of compensable ONDs and OMDs and explain the process of and the major changes introduced by the amendment, and future directions.
DISCUSSION
This amendment of standards for the recognition of ODs is a significant change since its first establishment in 1954. Because of the agent-based approach used in the previous version, clinicians including neurologists and psychiatrists were not familiar with compensable ONDs and OMDs. In the amendment made in 2013, the disease-specific approach using the ICD-10 code was included in ONDs and OMDs. Acute and chronic CNS disorders; toxic neuropathy; peripheral neuropathy; and manganese-related disorders including Parkinsonism, dystonia, and manganese-induced psychosis are examples of these changes. Several neurotoxic agents were included in the amendment. Further, ALS and PTSD were considered for inclusion in the new list. Both these diseases have cases that have been compensated in Korea. Because it is difficult for primary physicians to precisely diagnose ALS and to reach a consensus for the causal relationship between exposure and disease, in the end, ALS was not included in the list. More epidemiologic evidence, sounder evidence for the relationship between ALS and occupational exposure, and more compensated cases are necessary to include this disease in the OD list. In contrast, in the case of PTSD, there is strong evidence of occupational causality and many compensated cases; hence, PTSD was included in the new list. In the meantime, the occupational relationships of various mental disorders such as depression, adjustment disorders, anxiety disorders, panic disorders, and sleep disorders, which have led to increasing public concern, need more research for the inclusion of these disorders in the list.
There have been several specific issues related to exposure concentration and duration. At least 2 yr of exposure is a required condition for chronic encephalopathy due to CS
2. According to EC, the minimum exposure duration of CS
2 for chronic encephalopathy is 10 yr, and its maximum latent period is unclear (
7). Irrespective of the fact that there is little evidence for the effects of a 2-yr CS
2 exposure, the 2-yr exposure condition was retained in the new list. The exposure concentration condition for CS
2 seems high and debatable. The American Conference of Governmental Industrial Hygienists (ACGIH) changed the 8-hr time weighted average threshold limit for CS
2 from 10 ppm to 1 ppm in 2005 (
10). Hence, the concentration level and duration for CS
2 exposure need to be researched. The clause "within 3 months after the cessation of exposure" for trigeminal nerve palsy due to trichloroethylene (TCE) is controversial. According to the EC guide, trigeminal nerve palsy due to TCE needs the minimal exposure duration for several years and the maximal latency period for immediacy (
7). Because there is little evidence for the "within 3 months after cessation of TCE exposure," it could not act as an exclusion criterion; hence, the "3-month" condition was retained in the new list.
Although the amendment has many improvements, the work-relatedness evaluation (WRE) for ONDs and OMDs is not easy. Because ONDs have no specific pathognomonic feature for exposure to hazardous agents, WRE is not easy. The following might help clinicians to evaluate work-relatedness (
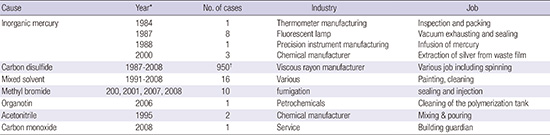
5): a sufficiently intense or prolonged exposure to chemicals; an appropriate neurologic syndrome based on knowledge about the putative chemical; evolution of symptoms and signs over a compatible temporal course; and exclusion of other neurologic disorders that may account for a similar syndrome. When clinicians diagnose several specific conditions such as a diffuse lesion of the gray matter of the brain, brain atropy, lesion in globus pallidus, demyelinating encephalopathy, and bilateral peripheral neuropathy, ONDs could be suspected. Further, epidemics of neurological or mental disorders are signs of OD. There were three cases of mercury poisoning in a waste treatment company in 2000 (
11). The workers involved used to extract silver with inorganic mercury. All workers had peripheral neuritis and abnormal findings on magnetic resonance imaging (MRI). One showed symptoms of hallucination and delirium and was diagnosed with brief reactive psychosis. Eight cases of peripheral neuropathy were found at an LCD manufacturer in 2005 (
12). All female workers cleaned LCD frames and were exposed to n-hexane. Clinicians should not exclude ONDs when they do not find abnormal findings with the usual diagnostic tools and even when there are no abnormal findings in radiological tests, neurological exams, and nerve conduction tests. Although chronic organic solvent intoxication causes abnormal emotions and behaviors, there might not be abnormal findings in traditional tests. In this case, neurobehavioral tests and psychological evaluations might be helpful. Biological monitoring for specific agents or metabolite tests of blood or urine are helpful when clinicians suspect ONDs due to specific agents. In such a case, the half-life of these agents should be considered. Because the half-life of organic solvents is usually less than one day, biological samples from the workplace might be helpful. While cadmium in blood has a very long half-life, mercury or manganese has a short half-life. The blood concentration for lead or mercury after several days from the cessation of exposure is not helpful for WRE. The interpretation of exposure monitoring such as the ambient air concentration of specific agents needs caution. Environmental monitoring results of usual and regular tasks are correlated with real exposure. However, the environmental monitoring for unusual and irregular tasks might not reveal real exposure. There were outbreaks of methyl bromide intoxication among fumigation workers who infused pesticide into containers containing agricultural goods (
13). The airborne concentration of methyl bromide in 10 cases ranged from an undetected level to 28.8 ppm. The number of non-working days was very small.
Based on scientific evidence and causality, the ILO list, EC schedule, and compensated cases in Korea were reviewed to revise the previous standards for the recognition of ODs in Korea. The disease-based approach using ICD-10 was added in the previous standards, which was an agent-specific approach. Amended compensable OMDs and ONDs in Korea are acute CNS disorders, chronic CNS disorders, chronic toxic neuropathy, peripheral neuropathy, manganese-related disorders, and PTSD. Several agents including TCE, benzene, vinyl chloride, organotin, methyl bromide, and CO were newly included in the list of acute CNS disorders. TCE, lead, and mercury were newly included in the list of chronic CNS disorders. Mercury, TCE, methyl n-butyl ketone, acrylamide, and arsenic were newly included in the list of peripheral neuropathies. PTSD was newly included as an OMD. This amendment makes the standard more comprehensive and practical. However, this amendment could not perfectly reflect recent scientific progress and social concerns. Ongoing effort, research, and expert consensus are needed to further improve the standard.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download