Abstract
Pulmonary thromboembolism (PTE) is a common clinical condition related to significant mortality. Furthermore, patients with PTE presenting with right heart thrombus show higher mortality due to rapid hemodynamic deterioration. But the optimal treatment of massive PTE is controversial although various methods have been developed and improved. Here, we presented a case of 56-yr-old woman with massive PTE showing hemodynamic collapse, who was successfully treated with extracorporeal membrane oxygenation (ECMO) adjunct to thrombolytic therapy even without thrombectomy. ECMO was useful for resuscitation and stabilization of the cardiopulmonary function. In conclusion, thrombolytic therapy complemented by ECMO may be an effective treatment option for acute massive PTE with hemodynamic instability.
Massive pulmonary thromboembolism (PTE) is a disease associated with poor clinical outcome due to the natural course of the disease frequently presenting with rapid hemodynamic deterioration. Front-line therapy of massive PTE is thrombolysis (1). But the treatment failure still occurs in about 8.2%-20% of patients (2, 3). The surgical embolectomy and catheter-based embolectomy are recommended in various cases. However, the outcome of embolectomy is not always satisfactory (4). Unfortunately, there's no consensus for the management of massive pulmonary thromboembolism.
This case report shows thrombolytic therapy supported by extracorporeal membrane oxygenation (ECMO) was used successfully for treatment of patient with massive PTE who suffered from cardiogenic shock.
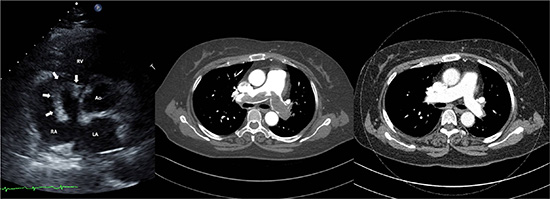
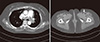
A 56-yr-old woman was transferred to emergency room of our hospital because of suspected PTE on October fifth, 2010. When she arrived, mental state was clear and she complained dyspnea and chest discomfort. Initial systolic blood pressure (BP) was 90mmHg and heart rate was 116 bpm. Chest X-ray revealed no remarkable finding. Transthoracic echocardiography demonstrated decreased contractility of dilated right ventricle (RV) with D-shaped left ventricle on parasternal short axis view (Fig. 1A). Also it showed a huge echogenic mass in dilated pulmonary trunk and a whip-like moving mass in right atrium (RA) (Fig. 1B). The right atrial mass moved through tricuspid valve to right ventricle. Estimated pulmonary artery systolic pressure was about 70 mmHg. Computed tomography (CT) finding also showed heavy thrombus in main pulmonary artery which extended into lobar branches of pulmonary system and deep vein thrombosis of left external iliac vein (Fig. 2).We diagnosed PTE with huge thrombus on RA clinically. Because the patient had stable vital sign, we selected thrombolytic therapy with tissue plasminogen activator (t-PA) infusion (100 mg over 2 hr). After one hour from t-PA infusion, the patient suddenly became unconscious. Her peripheral oxygen saturation was 76%, systolic BP 50 mmHg, and heart rate decreased to 33 bpm. Shortly afterward, the patient arrested and we started cardiopulmonary resuscitation (CPR). During CPR, our team made a critical decision to apply percutaneous cardiopulmonary support (PCPS) system for hemodynamic stabilization before surgical embolectomy. PCPS was inserted via right femoral artery and left femoral vein under fluoroscopic guidance and local anesthesia. The Capiox (Terumo, Tokyo, Japan) emergent bypass system was used. Thereafter, hemodynamic state of patient was stabilized at the PCPS flow rate of 3-3.5 L/min. We revised our plan to continue thrombolytic therapy and anticoagulation with PCPS support in consideration of stable vital sign and high bleeding risk of surgery during thrombolytic therapy. Heparin was administered intravenously and warfarin was overlapped after 5 days. Activated coagulation time was maintained within target range of 150-200 sec and activated partial thromboplastin time (aPTT) was controlled at approximately 80 sec during the PCPS support. She was decannulated sixty-two hours after PCPS insertion, when repeat echocardiography noted that RV function was much improved compared with initial echocardiography and estimated pulmonary artery systolic pressure decreased below 50mmHg even though mass remained on main pulmonary artery.
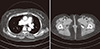
In sequence, ventilator was weaned and she transferred to general ward. General condition of the patient was improved gradually and she discharged without complication. After discharge, warfarin was continued at target international normalized ratio (INR) of 3. One month later from discharge, we followed up chest CT. The CT showed thrombus on main pulmonary artery and deep vein thrombus of left external iliac artery were clearly disappeared (Fig. 3). For two years follow up, she has been doing well without any complication and recurrence of thromboembolism.
Pulmonary thromboembolism with floating right heart thrombus is uncommon but reported mortality rate is over 44% (5, 6). The presence of right heart thrombus considerably increases the mortality rate compared to the presence of pulmonary thromboembolism alone (7). Despite the risk is high, the optimal treatment of pulmonary thromboembolism with right ventricular thrombus remains controversial.
Thrombolysis is the preferred primary therapeutic option, but the result is poor when pulmonary thromboembolism progresses rapidly (8). Surgical embolectomy can be another treatment option. However, mortality of surgical embolectomy in hemodynamically unstable patientis still high even though recent data have shown improved outcome (In-hospital mortality is 25% to 100% in patient with preoperative arrest) (9). Percutaneous catheter-directed thrombolysis or catheter thrombectomy is another treatment option (10, 11). Although these procedures are potentially effective, they take more time to apply and show poor outcome in patient with cardiovascular collapse (12). Pulmonary thromboembolism progresses to cardiogenic shock and cardiac arrest due to right ventricular failure (9). In this situation, ECMO may be able to play a key role for emergent circulatory and respiratory support.
The first heart-lung machine is developed by Gibbon for treatment of patient with pulmonary thromboembolism (13). And it has evolved into PCPS, a kind of ECMO. PCPS is commonly used in urgent situations because it can be inserted quickly and easily (14). In massive pulmonary thromboembolism, PCPS decompresses the acutely overloaded right ventricle and improves oxygenation (15). PCPS also can provide mechanical support when hypoxia has continued after thrombolysis because of increased lung vascular permeability with reperfusion injury (16). PCPS is considered an appropriate method for supporting hemodynamic circulatory collapse during thrombolysis.
Inoue et al. (17) reported a case that PCPS was used as adjunct to thrombolytic therapy for patient who has massive pulmonary thromboembolism with RV thrombus. This case, like our case, showed satisfactory clinical outcome and the patient has been well in follow-up period. Some article and case report suggest surgical embolectomy is preferred in hemodynamic unstable patient (18, 19). But there are no comparative trials of thrombolysis and surgery for massive pulmonary thromboembolism. A report documented that thrombolysis is an alternative to embolectomy because it has been shown that the risk of death or recurrent PTE decreased by 55% (20). In our opinion, outcome of the paper may be improved if thrombolysis would be complemented by ECMO.
In presented case, we suggest that thrombolysis complemented by ECMO could be a successful treatment option for the patients who have massive PTE with circulatory collapse even without surgical embolectomy.
Figures and Tables
Fig. 1
Initial transthoracic echocardiography (TTE) image. (A) D-shape of LV on parasternal short axis view. (B) Free-floating, whip-like right atrial (RA) mass (arrow) suggesting thrombus. RA, right atrium; LV, left ventricle; LA, left atrium; Ao, aorta.

References
1. Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, Nelson ME, Wells PS, Gould MK, Dentali F, et al. American College of Chest Physicians. Antithrombotic therapy for VTE disease: Antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2012; 141:e419S–e494S.
2. Charbonnier B, Meyer G, Stern M, Sors H, Brochier ML. Thrombolytic treatment of acute pulmonary embolism. Herz. 1989; 14:157–171.
3. Meneveau N, Seronde MF, Blonde MC, Legalery P, Didier-Petit K, Briand F, Caulfield F, Schiele F, Bernard Y, Bassand JP. Management of unsuccessful thrombolysis in acute massive pulmonary embolism. Chest. 2006; 129:1043–1050.
4. Stein PD, Matta F. Case fatality rate with pulmonary embolectomy for acute pulmonary embolism. Am J Med. 2012; 125:471–477.
5. Chartier L, Bera J, Delomez M, Asseman P, Beregi JP, Bauchart JJ, Warembourg H, Thery C. Free-floating thrombi in the right heart: Diagnosis, management, and prognostic indexes in 38 consecutive patients. Circulation. 1999; 99:2779–2783.
6. Torbicki A, Galie N, Covezzoli A, Rossi E, De Rosa M, Goldhaber SZ. ICOPER Study Group. Right heart thrombi in pulmonary embolism: Results from the international cooperative pulmonary embolism registry. J Am Coll Cardiol. 2003; 41:2245–2251.
7. Rose PS, Punjabi NM, Pearse DB. Treatment of right heart thromboemboli. Chest. 2002; 121:806–814.
8. Goldhaber SZ. Thrombolysis for pulmonary embolism. N Engl J Med. 2002; 347:1131–1132.
9. He C, Von Segesser LK, Kappetein PA, Mestres CA, Smith JA, Choong CK. Acute pulmonary embolectomy. Eur J Cardiothorac Surg. 2013; 43:1087–1095.
10. Weinberg L, Kay C, Liskaser F, Jones D, Tay S, Jaffe S, Seevanayagam S, Doolan L. Successful treatment of peripartum massive pulmonary embolism with extracorporeal membrane oxygenation and catheter-directed pulmonary thrombolytic therapy. Anaesth Intensive Care. 2011; 39:486–491.
11. Griffith KE, Jenkins E, Haft J. Treatment of massive pulmonary embolism utilizing a multidisciplinary approach: A case study. Perfusion. 2009; 24:169–172.
12. Margheri M, Vittori G, Vecchio S, Chechi T, Falchetti E, Spaziani G, Giuliani G, Rovelli S, Consoli L, BiondiZoccai GG. Early and long-term clinical results of AngioJet rheolytic thrombectomy in patients with acute pulmonary embolism. Am J Cardiol. 2008; 101:252–258.
13. GIBBON JH Jr. Application of a mechanical heart and lung apparatus to cardiac surgery. Minn Med. 1954; 37:171–185. passim
14. von Segesser LK. Cardiopulmonary support and extracorporeal membrane oxygenation for cardiac assist. Ann Thorac Surg. 1999; 68:672–677.
15. Maggio P, Hemmila M, Haft J, Bartlett R. Extracorporeal life support for massive pulmonary embolism. J Trauma. 2007; 62:570–576.
16. Kawahito K, Murata S, Adachi H, Ino T, Fuse K. Resuscitation and circulatory support using extracorporeal membrane oxygenation for fulminant pulmonary embolism. Artif Organs. 2000; 24:427–430.
17. Inoue T, Oka H, Oku H. Percutaneous cardiopulmonary support for the treatment of right ventricular thrombus. Perfusion. 2002; 17:73–75.
18. Takahashi H, Okada K, Matsumori M, Kano H, Kitagawa A, Okita Y. Aggressive surgical treatment of acute pulmonary embolism with circulatory collapse. Ann Thorac Surg. 2012; 94:785–791.
19. Hisatomi K, Yamada T, Onohara D. Surgical embolectomy of a floating right heart thrombus and acute massive pulmonary embolism: Report of a case. Ann Thorac Cardiovasc Surg. 2013; 19:316–319.
20. Büller HR, Agnelli G, Hull RD, Hyers TM, Prins MH, Raskob GE. Antithrombotic therapy for venous thromboembolic disease: The seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest. 2004; 126:401S–428S.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download