Abstract
This study evaluated the outcomes of off-pump coronary artery bypass surgery (OPCAB) with severe left ventricular dysfunction using composite bilateral internal thoracic artery grafting. From January 2001 to December 2008, 1,842 patients underwent primary isolated OPCAB with composite bilateral internal thoracic artery grafting. A total of 131 of these patients were diagnosed with a severely depressed preoperative left ventricle ejection fraction (LVEF) (≤0.35). These patient outcomes were compared with the outcomes of 830 patients that had mildly or moderately depressed LVEF (0.36 to 0.59) and 881 patients with normal LVEF (>0.6). The early mortality for patients with severe LVEF was 2.3%. The 3-yr and 7-yr survival rate for patients with severe LV dysfunction was 86.0% and 82.8%, respectively. Multivariate analysis showed that severe LV dysfunction EF increased the risk of all-cause death (P=0.012; hazard ratio [HR],2.14; 95% confidence interval [CI],1.19-3.88) and the risk of cardiac-related death (P=0.008; HR,3.38; 95% CI, 1.37-8.341). The study identified positive surgical outcomes of OPCAB, although severe LVEF was associated with two-fold increase in mortality risk compared with patients who had normal LVEF.
Coronary artery bypass surgery in patients with severe left ventricular (LV) dysfunction remains challenging to cardiac surgeons. However, advances in surgical technique and stabilizing instruments have allowed off-pump coronary artery bypass surgery (OPCAB) to be an effective alternative to conventional cardiopulmonary bypass-supported grafting, even in patients with left ventricular dysfunction (1, 2). In addition, bilateral internal thoracic arterial grafting outcomes have been reported to be better than those of single internal thoracic arterial grafting (3, 4). Although OPCAB with bilateral internal thoracic arterial grafting can be an effective strategy for patients with severe left ventricular dysfunction, little is known about the outcomes of this strategy.
The purpose of this study was to compare the outcomes of patients with severe left ventricular dysfunction who underwent OPCAB and bilateral internal thoracic arterial grafting to those of patients with impaired and normal left ventricular function.
From January 2001 to December 2008, 2,684 patients underwent isolated coronary artery bypass grafting (CABG) at Samsung Medical Center in Seoul, Korea. Among these patients, 1,842 (68.6%) underwent OPCAB with composite bilateral internal thoracic arterial grafting and were retrospectively reviewed. Patients that required emergent operation or a concomitant valve or other major cardiac operation were excluded from the study.
A standard midline sternotomy incision was used to expose the heart. The internal thoracic arteries were prepared by skeletonization with sharp dissection and branch clipping, and the OPCAB technique used in this study was described previously (5). The technique applied a continuous running 8-0 Prolene suture (Ethicon, Piscataway, NJ, USA) to all anastomoses with the exception of the proximal aorta anastomosis, which was constructed with a 6-0 Prolene continuous suture (Ethicon).
Our strategy was to revascularize the lesion that received distal blood flow from collateral branch because severe obstruction at proximal site firstly. However, in most cases, the majority of the procedures first anastomosed the left internal thoracic artery to the left anterior descending artery and its branches, then the right internal thoracic artery was anastomosed to the circumflex artery, and the right coronary artery was revascularized (Fig. 1). The proximal anastomosis on the aorta was constructed after completion of the distal anastomosis on the right coronary artery. All of the patients received left coronary artery bypasses with composite bilateral internal thoracic artery grafts. However, the right coronary arteries were bypassed with the distal extension of right internal thoracic artery grafts in 666 patients, in-situ right gastroepiploic arterial grafts in 418 patients, saphenous venous grafts in 286 patients and radial arterial grafts in 38 patients (Fig. 2).
An early event was defined as an event that occurred within the first 30 days after the operation, and a late event refers to all occurrences after the designated 30 postoperative days. Cardiac death included in-hospital mortality, cardiogenic death, and sudden death. A cardiac event was defined as a cardiac death, myocardial infarction, heart failure, reintervention, return of angina, and sudden death. The left ventricular ejection fraction (LVEF) was stratified according to the following designations: severely impaired (0.35 or less), impaired (0.36 to 0.59), and normal (0.6 or more). Preoperative renal dysfunction was defined as a preoperative serum creatinine level greater than or equal to 1.5 mg/dL. Postoperative atrial fibrillation was defined as a new atrial fibrillation that lasted more than 2 hr and was documented with an electrocardiogram. Myocardial infarction was defined by new Q waves in electrocardiogram or a peak creatine kinase-MB level greater than 50 ng/mL. A postoperative stroke was defined as a central neurologic deficit that persisted for more than 72 hr and was confirmed by computed tomography or magnetic resonance imaging. Follow-up information was obtained either by direct patient contact or through a telephone questionnaire.
Patient survival was ascertained by National Death Index information provided to our institution by the Korea Statistics Promotion Institute for use in medical research. Late follow-up was available for 96.6% of the surviving patients, and the mean follow-up duration was 50.1±26.2 (maximum 107) months.
Continuous variables are reported as the mean±standard deviation. Categorical data were analyzed using the chi-square statistic and with Fisher's exact test where appropriate. Univariate variables with a P value less than or equal to 0.2 were included in a multivariate logistic regression analysis for operative mortality. The Kaplan-Meier method was used to calculate freedom from overall death, freedom from cardiac death and freedom from cardiac events. All statistical analyses were performed using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA).
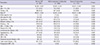
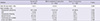
The preoperative patient characteristics are summarized in Table 1. Patients with severe LV dysfunction showed higher incidence of NYHA or CCS class IV, onset of acute myocardial infarction within 14 days. Also more cases were diagnosed with triple vessels disease and needed preoperative intra-aortic balloon pump (IABP) in severe LV dysfunction group. Three patients diagnosed with severely impaired LVEF died within 30 days (2.3%). The causes of death were multi-organ failure due to low cardiac output in one patient and small bowel infarction in the other two patients. One patient (0.1%) was from the normal LVEF group and the other two patients (0.2%) who died were in the mild to moderate LV dysfunction patient group. The mortality rate in severely impaired LVEF patients was significantly higher than those in the impaired and normal LVEF patient groups (P=0.004). The incidences of new arrhythmia and neurologic complication were significantly higher in the severely impaired LVEF patients (P<0.001). Deep sternal wound infection occurred in 13 patients (0.7%), and an increased risk of deep sternal wound infection was found in patients with history of myocardial infarction (2.3%) or a postoperative cerebrovascular accident (5.4%). The results did not indicate a statistical difference between patients with diabetes and patients who underwent reoperation due to bleeding (Table 2). However, the independent predictors of 30 day mortality included reoperation for bleeding (hazard ratio [HR] 26.17, P=0.013) and postoperative neurologic complication (HR 21.02, P<0.001).
There were 19 late deaths, including eight cardiac deaths and 11 non-cardiac deaths in the severely impaired LVEF patient group. The causes of non-cardiac deaths included cancer in four patients, cerebral hemorrhage in three patients, stroke in one patient and other causes in three patients.
The survival rate at 3 and 7 yr was 86.0% and 82.8%, respectively (Fig. 1A), freedom from cardiac death was 93.2% and 92.0% (Fig. 1B), and freedom from cardiac event was 84.6% and 78.9% (Fig. 1C), respectively, in the severely impaired LVEF patient group.
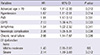
The risk of all-cause mortality attributable to severe left ventricular dysfunction, when adjusted for all covariates, increased two-fold compared with normal LVEF patients (HR, 2.14; 95% C, 1.19-3.88; P=0.012). Although this was not the case for patients with moderately impaired LVEF (HR ,1.40; 95% CI, 0.95-2.06; P=0.090).
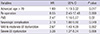
The multivariate Cox proportional hazard model revealed that other independent predictors of overall mortality were old age, hypertension, peripheral vascular disease, chronic renal failure, postoperative new arrhythmia, neurologic complication and chronic obstructive pulmonary disease (Table 3). The risk of all-cause mortality increased significantly for patients with severely impaired LVEF compared to patients with impaired LVEF (P=0.017). The independent predictors of cardiac-death free survival were impaired LVEF, severely impaired LVEF, old age, reoperation for bleeding, neurologic complication and peripheral vascular disease (Table 4). Additionally, impaired LVEF, severely impaired LVEF and NYHA class IV were independent predictors of cardiac event-free survival (Fig. 3).
Early postoperative echocardiography was performed on all patients prior to discharge, with the exception of patients who died in the hospital. Early mean LVEF improvement was 4.5±9.5% in patients with severe LV dysfunction (131 patients, P<0.001). Late mean LVEF improvement was 7.8±11.2% on late echocardiography, which was performed 29.4±25.6 months after surgery in 109 patients with severe LV dysfunction (P<0.001). Severe LV dysfunction patients showed improvement in LV dysfunction at last follow up.
Surgical revascularization in severe left ventricular dysfunction remains challenging for cardiac surgeons. Extracorporeal circulation can activate inflammatory mediators, which can affect the preservation of interventricular septal movement and exacerbate myocardial damage in compromised LV (6).
A recent study reported that revascularization with a drug-eluting stent implantation offered comparable outcomes to coronary artery bypass surgery in patients with severe left ventricular dysfunction (7). However, the study did not describe the application of a bilateral internal thoracic graft. Herz et al. (8) reported that surgical revascularization with the bilateral internal thoracic artery indicated better midterm clinical outcomes than a drug-eluting stent, but Jegaden et al. (9) reported that the extended use of arterial grafts could significantly affect the long-term myocardial recovery. The study by Jegaden et al. also reported that the postoperative LVEF improvement was less than 1% in patients with bilateral internal thoracic arterial grafting and concluded that the extended use of arterial grafts was not correlated with significant myocardial recovery. In our study, there was significant LVEF improvement on early echocardiography. The study by Jegaden et al. did not describe the internal thoracic artery harvesting technique and involved conventional coronary artery bypass surgery. The technique in this study harvested skeletonized internal thoracic arterial grafts because the free blood flow from the skeletonized internal thoracic artery has been reported to be almost twice as high as that from a non-skeletonized artery (10). Based on these results, higher free blood flow from skeletonized internal thoracic arterial grafts with OPCAB to avoid global ischemic damage to the myocardium may prove to be beneficial for early myocardial recovery.
There are few reports about long-term survival of patients with severe left ventricular dysfunction that have undergone OPCAB. Goldstein et al. (1) concluded that multi-vessel off-pump revascularization in patients with severe left ventricular dysfunction is a safe and effective alternative to conventional grafting. However, their study did not report any long-term results. In this study, the actuarial survival for severe left ventricular dysfunction was 86.0% and 82.8% at 3 and 7 yr, respectively, and these findings are comparable to other recent studies. For example, Endo et al. (4) reported a 67.4% survival rate after eight years in patients with a preoperative LVEF of 40% or less with the use of bilateral internal thoracic arterial grafts. Ahmed et al. (11) reported 69% and 48% survival at 5 and 10 yr, respectively, in a study of 162 patients with severe left ventricular dysfunction that underwent conventional coronary artery bypass surgery. The study by Ahmed et al. defined severe left ventricular dysfunction as a preoperative LVEF of 30% or less. In our study, the survival rate of patients with a preoperative LVEF of 35% or less was 82.8% five years after the procedure. In addition, the 30-day mortality of patients in this study with severe left ventricular dysfunction was 2.3%, which is comparable to other recent reports (12, 13).
Harvesting the bilateral internal thoracic arteries is generally a major risk factor for sternal infection, especially in patients with diabetes mellitus. Pevni et al. (14) reported that independent risk predictors for deep sternal infection included chronic obstructive pulmonary disease, repeated operations, and diabetic mellitus regardless of insulin dependence. However, some authors reported that bilateral internal thoracic artery harvesting in patients with diabetic mellitus was not associated with an increase in the rate of deep wound infections (15, 16). In this study, we harvested the bilateral internal thoracic arteries with the skeletonizing technique and determined that deep sternal wound infections presented in 13 of the patients (0.7%). Statistically, an increased risk of deep sternal infection was associated with previous myocardial infarction and a postoperative cerebrovascular accident. In addition, the multivariable logistic regression analysis results did not indicate that diabetes was associated with nor was an independent predictor of deep sternal wound infection.
Numerous patients with severe left ventricular dysfunction experienced troublesome ventricular arrhythmia after surgery. Currently, the application of an intra-aortic balloon pump, magnesium and amiodarone are effective for patients with ventricular arrhythmia (17).
This study identified several independent predictors of late survival which included chronic renal failure, peripheral vascular disease, chronic obstructive pulmonary disease, neurologic complication, postoperative new arrhythmia, postoperative renal failure, hypertension and old age. Previous studies have documented the importance of renal impairment in patient outcomes, especially in patients with left ventricular dysfunction (18).
In addition, a few studies have reported the independent predictors of long-term survival of patients with severe left ventricular dysfunction coronary artery disease. Ahmed et al. (11) reported that old age, emergency, mitral competence, smoking, respiratory disease, diabetes, postoperative renal failure, pleural effusion, left internal thoracic artery impairment, cerebrovascular disease and prolonged intubation were independent risk factors for an increased long-term mortality risk. In addition, Filsoufi et al. (19) reported that reoperation, peripheral vascular disease, congestive symptoms and being female were independent predictors of long-term survival in patients with an LVEF less than 30%. However, all covariates in this study were included in a multivariable Cox proportional hazard model without univariate analysis.
There were several limitations to this present study. First, this study had a retrospective and non-random design. Second, the authors did not routinely perform invasive coronary angiography and therefore could not evaluate the patency of all grafts. Third, the follow-up duration could be insufficient to evaluate the long-term outcomes of coronary revascularization; therefore, additional research studies are needed to address these aspects of the study design.
In conclusion, the results of this study indicated that OPCAB using composite bilateral internal thoracic artery grafts in patients with severe left ventricular dysfunction had outcomes comparable to or better than those reported after other surgical strategies. The analysis indicates that OPCAB using composite bilateral internal thoracic artery grafts could be used as safe and effective strategy for patients with severe left ventricular dysfunction.
Figures and Tables
Fig. 1
A photograph of the operative field showing the exposure aided by a stabilizing device and the internal thoracic artery composite grafts after completion of all anastomosis (20).

Fig. 2
Different strategies for grafting the right coronary artery or its branches: (A) with the right internal thoracic artery as a part of the Y-composite graft (n = 666), (B) with the in situ right gastroepiploic artery (n = 418), (C) with a saphenous vein aorto-coronary graft (n = 286).

Fig. 3
Survival curves according to left ventricular function: (A) overall survival, (B) survival free from cardiac death, (C) survival free from cardiac events.

References
1. Goldstein DJ, Beauford RB, Luk B, Karanam R, Prendergast T, Sardari F, Burns P, Saunders C. Multivessel off-pump revascularization in patients with severe left ventricular dysfunction. Eur J Cardiothorac Surg. 2003; 24:72–80.
2. Pande S, Agarwal SK, Kundu A, Kale N, Chaudhary A, Dhir U. Off-pump coronary artery bypass in severe left ventricular dysfunction. Asian Cardiovasc Thorac Ann. 2009; 17:54–58.
3. Lytle BW, Blackstone EH, Sabik JF, Houghtaling P, Loop FD, Cosgrove DM. The effect of bilateral internal thoracic artery grafting on survival during 20 postoperative years. Ann Thorac Surg. 2004; 78:2005–2012.
4. Endo M, Nishida H, Tomizawa Y, Kasanuki H. Benefit of bilateral over single internal mammary artery grafts for multiple coronary artery bypass grafting. Circulation. 2001; 104:2164–2170.
5. Kim WS, Lee J, Lee YT, Sung K, Yang JH, Jun TG, Park PW. Total arterial revascularization in triple-vessel disease with off-pump and aortic no-touch technique. Ann Thorac Surg. 2008; 86:1861–1865.
6. Akins CW, Boucher CA, Pohost GM. Preservation of interventricular septal function in patients having coronary artery bypass grafts without cardiopulmonary bypass. Am Heart J. 1984; 107:304–309.
7. Gioia G, Matthai W, Gillin K, Dralle J, Benassi A, Gioia MF, White J. Revascularization in severe left ventricular dysfunction: outcome comparison of drug-eluting stent implantation versus coronary artery by-pass grafting. Catheter Cardiovasc Interv. 2007; 70:26–33.
8. Herz I, Moshkovitz Y, Loberman D, Uretzky G, Braunstein R, Hendler A, Zivi E, Ben-Gal Y, Mohr R. Drug-eluting stents versus bilateral internal thoracic grafting for multivessel coronary disease. Ann Thorac Surg. 2005; 80:2086–2090.
9. Jegaden O, Bontemps L, de Gevigney G, Eker A, Montagna P, Chatel C, Itti R, Mikaeloff P. Does the extended use of arterial grafts compromise the myocardial recovery after coronary artery bypass grafting in left ventricular dysfunction? Eur J Cardiothorac Surg. 1998; 14:353–359.
10. Deja MA, Woś S, Gołba KS, Zurek P, Domaradzki W, Bachowski R, Spyt TJ. Intraoperative and laboratory evaluation of skeletonized versus pedicled internal thoracic artery. Ann Thorac Surg. 1999; 68:2164–2168.
11. Ahmed WA, Tully PJ, Baker RA, Knight JL. Survival after isolated coronary artery bypass grafting in patients with severe left ventricular dysfunction. Ann Thorac Surg. 2009; 87:1106–1112.
12. Jones RH, Velazquez EJ, Michler RE, Sopko G, Oh JK, O'Connor CM, Hill JA, Menicanti L, Sadowski Z, Desvigne-Nickens P, et al. Coronary bypass surgery with or without surgical ventricular reconstruction. N Engl J Med. 2009; 360:1705–1717.
13. Nardi P, Pellegrino A, Scafuri A, Colella D, Bassano C, Polisca P, Chiariello L. Long-term outcome of coronary artery bypass grafting in patients with left ventricular dysfunction. Ann Thorac Surg. 2009; 87:1401–1407.
14. Pevni D, Uretzky G, Mohr A, Braunstein R, Kramer A, Paz Y, Shapira I, Mohr R. Routine use of bilateral skeletonized internal thoracic artery grafting: long-term results. Circulation. 2008; 118:705–712.
15. Agrifoglio M, Trezzi M, Barili F, Dainese L, Cheema FH, Topkara VK, Ghislandi C, Parolari A, Polvani G, Alamanni F, et al. Double vs single internal thoracic artery harvesting in diabetic patients: role in perioperative infection rate. J Cardiothorac Surg. 2008; 3:35.
16. Momin AU, Deshpande R, Potts J, El-Gamel A, Marrinan MT, Omigie J, Desai JB. Incidence of sternal infection in diabetic patients undergoing bilateral internal thoracic artery grafting. Ann Thorac Surg. 2005; 80:1765–1772.
17. Gupta S, Pressman GS, Fiqueredo VM. Incidence of, predictors for, and mortality associated with malignant ventricular arrhythmias in non-ST elevation myocardial infarction patients. Coron Artery Dis. 2010; 21:460–465.
18. Hillis GS, Zehr KJ, Williams AW, Schaff HV, Orzulak TA, Daly RC, Mullany CJ, Rodeheffer RJ, Oh JK. Outcome of patients with low ejection fraction undergoing coronary artery bypass grafting: renal function and mortality after 3.8 years. Circulation. 2006; 114:I414–I419.
19. Filsoufi F, Rahmanian PB, Castillo JG, Chikwe J, Kini AS, Adams DH. Results and predictors of early and late outcome of coronary artery bypass grafting in patients with severely depressed left ventricular function. Ann Thorac Surg. 2007; 84:808–816.
20. Lee YT, Park KH. Characteristic and harvesting technique of bypass conduits: concise coronary artery bypass. 1st ed. Seoul: Korea Medical Book Publicher;2008. p. 50–51.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download