Abstract
IgG4-related disease (IgG4-RD) is characterized by a systemic involvement of tumor-like lesions with IgG4-positive plasmacytes. We experienced a case of IgG4-RD developed in a patient with bronchial asthma (BA) and chronic rhinosinusitis (CRS). A 55-yr-old female patient with BA and CRS complained of both eyes and neck swelling as well as a recurrent upper respiratory infection in recent 1 yr. The serum levels of IgG4, creatinine, and pancreatic enzymes were elevated. A biopsy of the submandibular gland showed an abundant infiltration of IgG4-positive plasmacytes. Her symptoms remarkably improved after the treatment of a systemic steroid that has been maintained without recurrence. We report a rare case of IgG4-RD developed in a patient with BA and CRS.
IgG4-related disease (IgG4-RD) is an immune-mediated disease which is newly recognized as a systemic disease. It was initially described there was a relationship between autoimmune pancreatitis and IgG4 molecules in 2001 (1). However, several recent studies have revealed that IgG4 molecules have a relationship not only with the pancreas but also with the salivary gland, lung, liver, stomach, colon, and lymph node (2, 3). IgG4-RD has been reported in almost every organ system and is characterized by the formation of tumor-like lesions, storiform fibrosis and infiltration of IgG4-positive plasmacytes in involved organs. A notable study reported that approximately 44% of patients with autoimmune pancreatitis (AIP) also had allergic diseases (4). However, there have been few reported cases of this disease with comorbid allergic diseases due to the low prevalence of IgG4-RD. We report a first case of IgG4-RD accompanied with bronchial asthma (BA) and chronic rhinosinusitis (CRS) in Korea.
A 55-yr-old female with BA and CRS presented swelling of both eyes and neck aggravated 1 yr ago. The symptoms first developed 10 yr ago with cough, sputum, wheezing, nasal obstruction and rhinorrhea, which had remained with no change in size for 2 yr. She visited a local clinic due to the enlargement of a mass-like lesion 8 yr ago and then started to take 5 mg of prednisolone every other day. The swelling was temporarily reduced with a systemic steroid; however, the mass lesions were again aggravated whenever the steroid was stopped. She suffered from chronic cough with sputum and recurrent upper respiratory infections recent as of 1 yr; in addition, she was diagnosed with bronchial asthma 6 months ago. Her mass lesions were also aggravated in recent 1 yr; subsequently, she visited our hospital (October 2, 2012) for an evaluation of swelling of eyes and neck as well as recurrent respiratory infections. She experienced neither eye pain nor neck pain, did not complain of any visual problems or show systemic symptoms (such as febrile sensation and general weakness). Her asthmatic symptoms were well-controlled after being prescribed an inhaled corticosteroid. She had no previous history of any drug or food allergies. Her physical examination on the first visit revealed bilaterally swollen eyes and enlarged submandibular glands, with a size of 4×5 cm (Fig. 1). The diffuse swelling of both eyes was fairly well-demarcated, nodular and movable. There was no visual field defect or a limitation of ocular movement. The palpable masses of submandibular glands were movable and nodular without tenderness. Other organomegalies (except the lesions of eyes and neck) were not observed. The abdomen was not distended, there was no palpable lymph node, and her breath sound was clear without wheezing. Laboratory findings included a blood eosinophilia of 1,900/µL and elevated levels of erythrocyte sedimentation rate (ESR) 73 mm/hr, serum creatinine 1.6 mg/dL, and pancreatic enzymes (amylase 268 U/L, lipase 713 U/L). Total IgE level and eosinophil cationic protein (ECP) were also elevated (913 KU/L and >200 µg/L respectively). Serum lactate dehydrogenase (LDH, 113 U/L) level, liver function test and cardiac enzymes were within the normal range. Chest radiography and electrocardiogram showed no specific findings. To evaluate her asthmatic status, we performed a methacholine challenge test and the result was positive: provocative concentration causing a 20% fall in FEV1 (PC20), 0.86 mg/mL; FEV1/FVC, 64.57%; FEV1, 1.78 L; FEV1% predicted, 64.9%. A skin prick test (SPT) to all of the common inhalant allergens (Bencard, Bradford, UK) showed negative responses. We checked the serum levels of total IgG and IgG subclasses suspecting an IgG subclass deficiency due to an increased susceptibility to upper respiratory infection. The levels were markedly elevated: serum total IgG, 4,486 mg/dL (normal: 916-1,796 mg/dL); IgG1, 11,102.9 mg/L (normal: 3,824.0-9,286.0 mg/L); IgG2, 17,958.0 mg/L (normal: 2,418.0-7,003.0 mg/L); IgG4, 2,106.4 mg/L (normal: 39.2-864.0). Therefore, we suspected IgG4-RD on the basis of the mass lesions and elevated IgG4 level. Considering the possibility of systemic involvement of IgG4-RD, we performed multiple computed tomography (CT) scans of the neck, chest, and abdomen to establish the extent of the disease and to find any subclinical diseases. Neck CT imaging disclosed hypertrophies of extraocular muscles and the bilateral enlargements of lacrimal, submandibular and sublingual glands as well as mucoperiosteal thickening of maxillary and ethmoidal sinus indicating CRS (Fig. 2). Chest CT imaging study revealed that both lungs were diffusely involved with bilateral hilar lymph nodes, peribronchovascular bundle thickening, multifocal centrilobular opacities and interlobular septal thickening (Fig. 2). Irregular low density lesions of both kidneys and multifocal strictures as well as an irregular dilatation of the pancreatic duct were noted in the abdominal CT scan (Fig. 3). The right submandibular gland was biopsied to obtain a key pathological finding of IgG4-RD. The pathological features showed an abundant infiltration of IgG4-positive plasmacytes around the lymphoid follicles and glandular tissues. Cartwheel-like fibrosis (which is strongly indicative of IgG4-RD) was also noted (Fig. 4). Finally, we could confirm the diagnosis of IgG4-RD according to the criteria in 2011 (5, 6). We started a systemic steroid therapy with methylprednisolone 0.4 mg/kg/d. The nasal and asthmatic symptoms of the patient substantially improved and the elevated serum creatinine and pancreatic enzyme level was normalized at 2 weeks of follow-up. The masses significantly diminished with the treatment of a systemic steroid, which has been maintained with no recurrence. We performed follow-up measurements of lung function test 2 months later. Her FEV1% had improved to 103.8% predictive (2.82 L) compared to her initial FEV1 level (64.9% predictive, 1.78 L).
We describe a rare case diagnosed with IgG4-RD that involves multiple systemic organs including extraocular muscles, lacrimal and salivary glands, lung, lymph node, kidneys and pancreas, accompanied with BA and CRS. IgG4-RD usually develops subacutely and most patients are not constitutionally ill despite multiple systemic involvement; subsequently, it comes to clinical attention due to tumorous swellings or organ damage. However, it is frequently discovered incidentally through radiographic findings or pathologic specimens. The diagnosis of IgG4-RD is still debated, with significant discussions over the establishment of proper diagnostic criteria. Histopathological analysis of biopsy tissues remains fundamental in the diagnosis of IgG4-RD. After the identification of the typical pathological features, we conclusively diagnosed the patient with IgG4-RD according to diagnostic criteria suggested by Okazaki et al. (5, 6); based on mass lesions in multiple organs, elevated serum IgG4 level (more than 135 mg/dL) and typical histopathological findings (5, 6).
There are several theories that suggest the pathogenic mechanism of IgG4-RD. IgG4-RD is associated with potential triggers of IgG4-RD; autoimmunity, molecular mimicry, and bacterial infection (7). Potential triggers activate immune reactions in affected organs in which Th2-cell responses are predominant and augment the expression of Th2-related cytokines such as interleukin (IL)-4, IL-5, IL-10, and IL-13 (7, 8, 9). These cytokines induce serum eosinophilia, elevated IgE and IgG4 level, and contribute to numerous inflammatory and IgG4-positive cell infiltrations within the affected organs. In contrast to classic autoimmune conditions, regulatory T cells responsible with IL-10 and transforming growth factor-β (TGF-β) expression are also activated (10). Overexpressed TGF-β may stimulate fibroblasts and subsequently cause organ fibrosis (11). The pathogenic and immunologic mechanisms of IgG4-RD are unclear; however, these mechanisms are considered to contribute to the clinical, laboratory, and pathologic features of IgG4-RD.
This case is meaningful because it is a first case report of IgG4-RD in patients suffering from chronic BA and CRS in Korea. The patient experienced recurrent aggravations of mass lesions simultaneously with aggravation of her asthmatic symptoms and wheezing. The symptoms were initially thought to be recurrent respiratory infections on suspicion of an IgG subclass deficiency with BA. However, after diagnosing her with IgG4-RD, it is thought that lung involvement of IgG4-RD caused and aggravated the respiratory symptoms simultaneously with the mass lesions. It is unclear how often pulmonary involvement is present with IgG4-RD although some patients initially present respiratory symptoms such as cough, dyspnea, sputum, hemoptysis or chest discomfort (12, 13). Her mass lesions also developed with CRS symptoms such as rhinorrhea and nasal obstruction and her symptoms waxed and waned together with steroid therapy.
A previous study reported that about 44% of patients with AIP had allergic diseases (4). There were 20 patients who had present and/or past history of allergic diseases composed of allergic rhinitis, atopic dermatitis, BA, and drug allergies (4). It also showed that the peripheral eosinophil count and serum IgE level were significantly higher in AIP patients with allergic aspects versus those without allergic aspects (4). Several other reports deal with eosinophilia in IgG4-RD. For example, a survey of AIP in Japan showed peripheral eosinophilia (>500 cells/µL) existed in 21% of AIP patients (14). Another study reported that 21% of AIP patients showed moderate eosinophilic infiltration histologically in the pancreas (15). Eosinophilia and allergic manifestations of IgG4-RD are closely related because overexpressed cytokines caused by Th2 cell activation (such as IL-4, IL-5, IL-10, and IL-13) promote the production of IgG4 antibodies as well as serum eosinophilia and IgE production that result in eosinophilic infiltration and allergic manifestations (4, 7, 16). The responsiveness of eosinophilia and allergic manifestations is unclear since there are no randomized controlled trials dealing with the treatment of IgG4-RD. Therefore, further studies concerning these questions are required.
In conclusion, this is the first report of a Korean patient diagnosed with IgG4-RD comorbid with BA and CRS who was successfully treated with a systemic steroid.
Figures and Tables
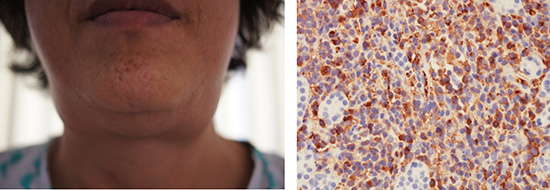
Fig. 1
Clinical manifestations of IgG4-related disease in the patient. (A) Facial photograph of the patient shows bilateral periorbital swelling. (B) Facial photograph of the patient shows bilateral enlargement of the submandibular glands and neck.

Fig. 2
Computed tomography (CT) images of the patient. (A) Chest CT image shows bilateral hilar lymphadenopathy (arrowheads). (B) Chest CT image shows peribronchovascular bundle thickening, centrilobular opacities and interlobular septal thickening.

Fig. 3
Computed tomography (CT) images of the patient. (A) Neck CT image shows diffuse enlargement of the sublingual (arrows) and submandibular (arrowheads) glands. (B) Abdominal CT image shows multifocal strictures and dilatations of the pancreatic duct in the pancreas body (arrows) and multifocal low attenuation of both kidneys (arrowheads).
Fig. 4
Histopathological features in a biopsy of the submandibular gland of the patient. The tissue specimen from the right submandibular gland shows dense lymphoplasma cell infiltration and typical storiform fibrosis (arrowheads) (A, H&E, ×20) and IgG4-positive plasmacytes (B, immunohistostain, ×40).
References
1. Hamano H, Kawa S, Horiuchi A, Unno H, Furuya N, Akamatsu T, Fukushima M, Nikaido T, Nakayama K, Usuda N, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001; 344:732–738.
2. Kamisawa T, Egawa N, Nakajima H. Autoimmune pancreatitis is a systemic autoimmune disease. Am J Gastroenterol. 2003; 98:2811–2812.
3. Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, Okamoto A, Egawa N, Nakajima H. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003; 38:982–984.
4. Kamisawa T, Anjiki H, Egawa N, Kubota N. Allergic manifestations in autoimmune pancreatitis. Eur J Gastroenterol Hepatol. 2009; 21:1136–1139.
5. Okazaki K, Uchida K, Koyabu M, Miyoshi H, Takaoka M. Recent advances in the concept and diagnosis of autoimmune pancreatitis and IgG4-related disease. J Gastroenterol. 2011; 46:277–288.
6. Okazaki K, Uchida K, Miyoshi H, Ikeura T, Takaoka M, Nishio A. Recent concepts of autoimmune pancreatitis and IgG4-related disease. Clin Rev Allergy Immunol. 2011; 41:126–138.
7. Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012; 366:539–551.
8. Kanari H, Kagami S, Kashiwakuma D, Oya Y, Furuta S, Ikeda K, Suto A, Suzuki K, Hirose K, Watanabe N, et al. Role of Th2 cells in IgG4-related lacrimal gland enlargement. Int Arch Allergy Immunol. 2010; 152:47–53.
9. Miyake K, Moriyama M, Aizawa K, Nagano S, Inoue Y, Sadanaga A, Nakashima H, Nakamura S. Peripheral CD4+ T cells showing a Th2 phenotype in a patient with Mikulicz's disease associated with lymphadenopathy and pleural effusion. Mod Rheumatol. 2008; 18:86–90.
10. Zen Y, Fujii T, Harada K, Kawano M, Yamada K, Takahira M, Nakanuma Y. Th2 and regulatory immune reactions are increased in immunoglobin G4-related sclerosing pancreatitis and cholangitis. Hepatology. 2007; 45:1538–1546.
11. Detlefsen S, Sipos B, Zhao J, Drewes AM, Klöppel G. Autoimmune pancreatitis: expression and cellular source of profibrotic cytokines and their receptors. Am J Surg Pathol. 2008; 32:986–995.
12. Zen Y, Nakanuma Y. IgG4-related disease: a cross-sectional study of 114 cases. Am J Surg Pathol. 2010; 34:1812–1819.
13. Ryu JH, Sekiguchi H, Yi ES. Pulmonary manifestations of immunoglobulin G4-related sclerosing disease. Eur Respir J. 2012; 39:180–186.
14. Nishimori I, Suda K, Oi I, Ogawa M. Autoimmune pancreatitis. Nihon Shokakibyo Gakkai Zasshi. 2000; 97:1355–1363.
15. Abraham SC, Leach S, Yeo CJ, Cameron JL, Murakata LA, Boitnott JK, Albores-Saavedra J, Hruban RH. Eosinophilic pancreatitis and increased eosinophils in the pancreas. Am J Surg Pathol. 2003; 27:334–342.
16. Kim YM, Kim YS, Jeon SG, Kim YK. Immunopathogenesis of allergic asthma: more than the Th2 hypothesis. Allergy Asthma Immunol Res. 2013; 5:189–196.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download