Abstract
We investigated the frequency of sleep disturbances and the association between sleep disturbances and glucoregulation in type 2 diabetic patients. The frequency of sleep disturbances in 614 type 2 diabetic patients was investigated using validated sleep questionnaires. There were 381 male and 233 female patients. The mean age was 59.7 ± 11.1 yr; the mean body mass index was 24.9 ± 4.4 kg/m2; the mean HbA1c was 7.8% ± 1.5%; and the mean duration of diabetes was 10.3 ± 8.4 yr. The questionnaires revealed insomnia in 48.2% of the patients while 8.5% reported excessive daytime sleepiness. A total of 49% of the patients was poor sleepers, while 28.5% had depression. Multivariate logistic regression analysis showed that there was no significant association between HbA1c and other sleep disturbances, such as poor sleep, insomnia, and short duration of sleep. Sleep disturbances were very common in patients with type 2 diabetes mellitus, whereas there was no association between poor or short sleep and glucoregulation. Awareness and identifying sleep complaints in such patients are necessary to improve their quality of daily life.
Sleep disturbances and chronic sleep shortage have become very common in modern society. The quality and quantity of sleep patterns are influenced by cultural, social, psychological, environmental, and genetic factors. In recent years, evidence from epidemiological and laboratory studies have shown that short or disturbed sleep is associated with glucose intolerance, insulin resistance, reduced acute insulin response to glucose (1, 2), and an increased risk of developing type 2 diabetes (3-6). Moreover, short or disturbed sleep is associated with cardiovascular disease (7), decreased quality of life, and economic burden (8). Because sleep modulates glucose metabolism and homeostasis, and influences quality of life, identifying sleep problems may be an important factor in treating type 2 diabetes. However, most studies of sleep and type 2 diabetes have focused mainly on obstructive sleep apnea and restless leg syndromes. There are limited studies on various sleep disturbances among those with type 2 diabetes using validated questionnaires.
We investigated the frequency of undiagnosed sleep disturbances not addressed previously and evaluated the association between sleep disturbances and glucoregulation in a population of type 2 diabetic patients using validated sleep questionnaires.
Study subjects were recruited from the outpatient diabetes clinics of two university hospitals in Chuncheon city using recognized questionnaires for assessing common sleep disturbances from January 2011 to April 2011. Participation in the study was offered to 614 consecutive type 2 diabetic patients > 18 yr old. Patients were excluded if any one of the following conditions was present: plasma creatinine levels > 1.4 mg/dL; congestive heart failure; or a major concurrent illness such as cancer, end-stage pulmonary disease, liver disease, severe painful peripheral neuropathy, or alcohol dependency. Anthropometric measurement, plasma fasting and 2 hr-postprandial glucose, and serum HbA1c level from each patient were obtained as well as the patients' clinical information relevant to diabetes and sleep using questionnaires.
Questionnaires for snoring, witnessed apnea, and insomnia as well as the Sleep Disorders Questionnaire Sleep Apnea subscale (SDQ-SA), the Pittsburgh Sleep Quality Index (PSQI), the Korean version of the Epworth Sleepiness Scale (K-ESS), and the Korean version of the Beck Depression Inventory (K-BDI) were applied to all patients. The questionnaires were self-administered and research nurse completed the unanswered questions by asking the patients.
Insomnia was defined as a positive response to at least one of following four questions. They are difficulty in falling asleep, maintaining sleep, early morning waking, and non-restorative sleep occurring at least three times per week over the preceding month (9).
The SDQ-SA uses 12 items to assess sleep apnea, using a cut-off score of ≥36 for males and ≥32 for females. The PSQI is a reliable and powerful screening measure to evaluate sleep quality and disturbances over the preceding month. Questionnaire responses contained seven components, each scored from 0 to 3, and the component scores were summed to provide the PSQI global score (range, 0 to 21), with higher scores indicating worse sleep quality. PSQI global scores ≥5 indicate poor sleepers.
The K-ESS is composed of eight questions on the subject's likelihood of dozing off or falling asleep in various situations that commonly occur in Korean daily life, being scored from 0 to 24. The K-ESS is a validated and widely used subjective measure of excessive daytime sleepiness. High scores indicate a greater likelihood of daytime sleepiness. A K-ESS score of ≥9 was used as a minimal criterion for diagnosis of subjective excessive daytime sleepiness.
The K-BDI is a 21-item, self-rating scale for assessing the experience of symptoms of depression over the preceding week. Each item-response scale ranges from 0 to 3, with higher scores indicating more severe symptoms of depression. The sum score (Beck Score) ranges from 0 to 63 points. The K-BDI is a reliable and well-validated measure for screening for symptoms of depression in adults. A Beck score of ≥16 points indicates clinically relevant depression.
The results are reported as mean±standard deviation or percentage. Statistical analysis was performed using SPSS software (version 19.0; SPSS Inc., Chicago, IL, USA). Values of P<0.05 were considered significant. Multivariate logistic regression analysis with the stepwise forward method was used to evaluate independent variables. Poor sleep was set as the dependent variable.
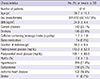
The baseline clinical characteristics of the patients are presented in Table 1. There were 381 male (62.1%) and 233 (37.9%) female patients. The patients had a mean age of 59.7±11.1 yr and a mean body mass index (BMI) of 24.9±3.4 kg/m2. The mean HbA1c level was 7.8%±1.5% and the mean duration of diabetes was 10.3±8.4 yr, with 51.8% concurrently having hypertension. Fifty-four (8.8%) subjects were taking sleep medication.
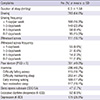
Table 2 showed the frequency of sleep complaints. The mean duration of sleep was 6.3±1.6 hr per day. Snoring occurred in 64% of the patients and 15.5% snored 6-7 days per week. Witnessed apnea was observed in 18.1% of the study population. Insomnia occurred in 48.2% of the patients, being more prevalent in women than in men (57.1% vs 42.8%, P=0.001). Difficulty in falling asleep and sleep maintenance was reported by 18.7% and 41.2% of insomniac patients, respectively, both being more common in women than in men (24.3% vs 15.6%, P<0.001 and 50.4% vs 36.2%, P=0.014, respectively).
The SDQ-SA score was 26.3±6.2 for men and 22.4±5.7 for women, with sleep apnea reported for 7.7% of the subjects. The mean K-ESS score was 4.8±1.6. Excessive daytime sleepiness (K-ESS≥9) occurred in 52 patients (8.5%). The mean global PSQI was 5.4±3.5 and 301 patients (49.0%) had a global PSQI score≥5, indicating a poor sleeper. The mean K-BDI score was 12.6±9.2 and depression (K-BDI≥16) was observed in 175 (28.5%) of the patients.
Being a poor sleeper (PSQI score≥5) was associated with the female sex, longer duration of diabetes, shorter duration of sleep, the presence of self-reported snoring, insomnia, restless leg syndrome, excessive daytime sleepiness, and depression. There was a significant correlation between the global PSQI score and the duration of diabetes (r=0.131, p=0.002). A duration of diabetes≥10 yr was associated with a higher global PSQI score compared to a duration of <10 yr (5.82 vs 4.98, p=0.004, Fig. 1). The highest quartile of duration of diabetes was associated with a greater frequency of insomnia, poor sleepers (PSQI score), and depression (Beck score) compared to the lowest quartile of duration of diabetes.
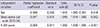
Multivariate logistic regression analysis, including age, sex, sleep apnea score (SDQ-SA), K-BDI score, and the duration of diabetes showed that the female sex (OR, 1.62; 95% CI, 1.09-2.39, p=0.016), the sleep apnea score (SDQ-SA) (OR, 1.05; 95% CI, 1.02-1.09, p=0.003), and the K-BDI score (OR, 1.06; 95% CI, 1.04-1.09, P<0.001) were independent risk factors for poor sleep in these patients (Table 3).
There were direct correlations between postprandial glucose and the duration of diabetes (r=0.096, P=0.046) and the sleep apnea score (SDQ-SA) (r=0.100, P=0.032). However, there was no correlation between HbA1c and sleep duration. There was no significant association between HbA1c values and other sleep disturbances, including poor sleep, insomnia, and the duration of sleep in a multivariate regression models.
We found that sleep disturbances were very common in type 2 diabetic patients. To the best of our knowledge, this study is the largest sample-sized survey to investigate various sleep complaints of type 2 diabetic patients using validated sleep questionnaires. There are few reports on sleep problems among type 2 diabetics other than sleep apnea and restless leg syndromes. In the present study, approximately half of the patients had insomnia or poor sleep, suggesting an overall poor quality of life in type 2 diabetes patients.
Sleep disturbances may have a harmful effect on glucose regulation. In previous studies, sleep deprivation impaired glucose metabolism and insulin sensitivities in healthy subjects (1, 10, 11) suggesting a potential association between sleep disturbances and impaired glucose metabolism, as assessed by HbA1c. Decreased slow-wave sleep, which normally occurs in poor sleepers or the elderly, may be correlated with a decrease in insulin sensitivity and glucose metabolism (12). Type 2 diabetic patients have a significantly decreased amount of slow-wave sleep compared to non-diabetic subjects, suggesting that sleep may affect glucoregulation in type 2 diabetic patients (13). In a previous study on 4,870 type 2 diabetics, Sleep duration was shown to have U-shaped associations with the HbA1c levels in type 2 diabetic patients, independent of potential confounders (14). However, on the contrary to the previous reports, our study failed to show the association. There is no association between HbA1c levels and sleep disturbances or between HbA1c and sleep duration. The reason of no association was not clarified and a community-based study with large population is needed.
In a previous report on 58 type 2 diabetic patients, the rate of insomnia was 50% (15). In that study, the mean age was 57.2 yr and sleep maintenance complaints were reported by 40% of patients. Our insomnia study reinforces previous results that insomnia is very common and that difficulty in sleep maintenance is a major complaint of type 2 diabetic patients with insomnia. In the general Korean population, nearly one in five (17%) report having insomnia at least three times per week (16). Insomnia is very common in type 2 diabetic subjects compared to the general Korean population. However, in our study population, the use of sleep medication for insomnia (8.8%) was relatively low considering the high rate of insomnia. Therefore, we suggest that the awareness and identification of insomnia in type 2 diabetes is insufficient in Korea.
In the present study, 49% of type 2 diabetic patients were poor sleepers according to the PSQI score. In a small cross-sectional study of 50 type 2 diabetics, 48% were poor sleepers based on the PSQI score (17). A study of 784 Korean type 2 diabetic patients reported that 38.4% had poor sleep quality using a PSQI score >5 (18). Another study showed that 69% of Indian patients had a global PSQI score ≥5, indicating that they were "poor sleepers"(19).
In our study, female sex, the sleep apnea score (SDQ-SA), and depression were independent predictors of poor sleepers. In a correlation analysis, longer duration of diabetes was associated with poor sleep quality, whereas in a multivariate logistic regression analysis we did not find an association between the duration of diabetes and poor sleepers.
In the general population, obstructive sleep apnea is 3%-7% for men and 0.8%-5% for women (20-22). In the present study, snoring occurred in 64% and witnessed apnea was present in 18.1% of the study population. Sleep apnea symptoms were reported in 7.7% of the subjects. Obstructive sleep apnea is very common in type 2 diabetic patients, independent of the BMI (23, 24). The prevalence of obstructive sleep apnea in patients with type 2 diabetes was from 58% to 86% and severity of obstructive sleep apnea is associated with glucose control (23). We used the SDQ-SA to assess sleep apnea and found that the rate was relatively low compared to previous studies (23, 24). However, habitual snoring (frequency≥4 days per week) was reported at 24.9%, suggesting a high probability of undetected sleep apnea. A recent study showed that many type 2 diabetic patients with obstructive sleep apnea had no clinical symptoms of this condition, suggesting possible under-diagnosis (24).
We also found that excessive daytime sleepiness occurred in 8.5% of the patients. There are limited data regarding daytime sleepiness in type 2 diabetes in the literature. In one study, the frequency of daytime sleepiness in type 2 diabetes was 20.5% using the Epworth Sleepiness Scale (ESS) questionnaire, with no significant difference from the normal glucose tolerance group (24). However, the study population was limited to 84 type 2 diabetic patients aged 61-63 yr old, who were all born in 1935. Because sleep disturbances increase with age, a wide age distribution and more subjects in our study may explain the different results (8.5% vs 20.5%).
Our study has some limitations. First, we have no accurate measures of sleep apnea (lack of polysomnography) and sleep duration (lack of actinography). Second, it is not a community-based study, with a relatively small sample size. We recruited type 2 diabetic patients attending the diabetic clinics in two university hospitals. A large community-based study is needed to better characterize the sleep disturbances of type 2 diabetic patients. Third, this study lacked any comparison with the general population. Fourth, we did not check for medication use, such as ACE inhibitors, statins, and beta-blockers that may affect sleep characteristics. Fifth, there was no assessment of hypoglycemia/diabetic polyneuropathy, which may affect sleep quality or duration of sleep.
We found that sleep disturbances were very common in patients with type 2 diabetes mellitus. Diabetologists have traditionally paid little attention to sleep problems in such patients, which may significantly affect the quality of life. Identifying and treating the sleep complaints of type 2 diabetic patients is necessary to improve their quality of daily life. Further study of the relationship between diabetes and sleep disturbances is required.
Figures and Tables
References
1. Buxton OM, Pavlova M, Reid EW, Wang W, Simonson DC, Adler GK. Sleep restriction for 1 week reduces insulin sensitivity in healthy men. Diabetes. 2010; 59:2126–2133.
2. Schmid SM, Hallschmid M, Jauch-Chara K, Bandorf N, Born J, Schultes B. Sleep loss alters basal metabolic hormone secretion and modulates the dynamic counterregulatory response to hypoglycemia. J Clin Endocrinol Metab. 2007; 92:3044–3051.
3. Beihl DA, Liese AD, Haffner SM. Sleep duration as a risk factor for incident type 2 diabetes in a multiethnic cohort. Ann Epidemiol. 2009; 19:351–357.
4. Chao CY, Wu JS, Yang YC, Shih CC, Wang RH, Lu FH, Chang CJ. Sleep duration is a potential risk factor for newly diagnosed type 2 diabetes mellitus. Metabolism. 2011; 60:799–804.
5. Chaput JP, Després JP, Bouchard C, Astrup A, Tremblay A. Sleep duration as a risk factor for the development of type 2 diabetes or impaired glucose tolerance: analyses of the Quebec Family Study. Sleep Med. 2009; 10:919–924.
6. Tuomilehto H, Peltonen M, Partinen M, Lavigne G, Eriksson JG, Herder C, Aunola S, Keinänen-Kiukaanniemi S, Ilanne-Parikka P, Uusitupa M, et al. Sleep duration, lifestyle intervention, and incidence of type 2 diabetes in impaired glucose tolerance: the Finnish Diabetes Prevention Study. Diabetes Care. 2009; 32:1965–1971.
7. Hoevenaar-Blom MP, Spijkerman AM, Kromhout D, van den Berg JF, Verschuren WM. Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: the MORGEN Study. Sleep. 2011; 34:1487–1492.
8. Skaer TL, Sclar DA. Economic implications of sleep disorders. Pharmacoeconomics. 2010; 28:1015–1023.
9. Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002; 6:97–111.
10. Taub LF, Redeker NS. Sleep disorders, glucose regulation, and type 2 diabetes. Biol Res Nurs. 2008; 9:231–243.
11. Donga E, van Dijk M, van Dijk JG, Biermasz NR, Lammers GJ, van Kralingen KW, Corssmit EP, Romijn JA. A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. J Clin Endocrinol Metab. 2010; 95:2963–2968.
12. Spiegel K, Tasali E, Leproult R, Van Cauter E. Effects of poor and short sleep on glucose metabolism and obesity risk. Nat Rev Endocrinol. 2009; 5:253–261.
13. Pallayova M, Donic V, Gresova S, Peregrim I, Tomori Z. Do differences in sleep architecture exist between persons with type 2 diabetes and nondiabetic controls? J Diabetes Sci Technol. 2010; 4:344–352.
14. Ohkuma T, Fujii H, Iwase M, Kikuchi Y, Ogata S, Idewaki Y, Ide H, Doi Y, Hirakawa Y, Nakamura U, et al. Impact of sleep duration on obesity and the glycemic level in patients with type 2 diabetes: the Fukuoka Diabetes Registry. Diabetes Care. 2013; 36:611–617.
15. Skomro RP, Ludwig S, Salamon E, Kryger MH. Sleep complaints and restless legs syndrome in adult type 2 diabetics. Sleep Med. 2001; 2:417–422.
16. Ohayon MM, Hong SC. Prevalence of insomnia and associated factors in South Korea. J Psychosom Res. 2002; 53:593–600.
17. Cunha MC, Zanetti ML, Hass VJ. Sleep quality in type 2 diabetics. Rev Lat Am Enfermagem. 2008; 16:850–855.
18. Shim U, Lee H, Oh JY, Sung YA. Sleep disorder and cardiovascular risk factors among patients with type 2 diabetes mellitus. Korean J Intern Med. 2011; 26:277–284.
19. Rajendran A, Parthsarathy S, Tamilselvan B, Seshadri KG, Shuaib M. Prevalence and correlates of disordered sleep in Southeast Asian indians with type 2 diabetes. Diabetes Metab J. 2012; 36:70–76.
20. Davies RJ, Stradling JR. The epidemiology of sleep apnoea. Thorax. 1996; 51:S65–S70.
21. Lurie A. Obstructive sleep apnea in adults: epidemiology, clinical presentation, and treatment options. Adv Cardiol. 2011; 46:1–42.
22. Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993; 328:1230–1235.
23. Pamidi S, Tasali E. Obstructive sleep apnea and type 2 diabetes: is there a link? Front Neurol. 2012; 3:126.
24. Schober AK, Neurath MF, Harsch IA. Prevalence of sleep apnoea in diabetic patients. Clin Respir J. 2011; 5:165–172.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download