INTRODUCTION
Iron deficiency (ID) is the most common nutritional deficiency and is a major cause of morbidity and mortality that is responsible for the majority of cases of anemia, ~20% of perinatal and ~10% of maternal mortalities in developing countries (
1). The National Health and Nutrition Examination Survey (NHANES) found that the prevalence of ID in the US females 20-49 yr and children 1-2 yr increased from 11% and 9%, respectively, in 1988-1994 to 14.4% and 15.7%, respectively, in 2002-2004 (
2,
3). ID, with or without anemia, adversely affects cognitive performance, the behavior and physical growth of infants, preschool and school-aged children, decreases immunity, and increases perinatal risks during pregnancy (
4-
6). In addition to the effects on health, ID reduces work capacity and productivity of adolescents and adults of any age, and has a negative impact on overall national socioeconomic development (
6,
7).
Surprisingly, even though ID is one of 10 most common risk factors related to the worldwide disease- and injury-burden (
1), the prevalence for ID is not known for most countries due to the high cost of the biochemical tests required to precisely define an individual's iron status. Due to this, the prevalence of anemia is commonly used as an indirect indicator of ID, based on the assumption that ~50% of all cases of anemia are iron deficient (IDAs). The Korea National Health and Nutrition Examination Survey (KNHANES) is a large-scale, cross-sectional nationwide survey by the Korean Ministry of Health and Welfare. It was first conducted in 1998 and then conducted every 3 yr until the present. Since 1998, the KHANES has identified the prevalence of anemia as 7.4%-9.5% overall, with a prevalence of 2.2%-4.8% in males and 11.9%-16.5% in females (
8). Among participants of the fourth KHANES in 2008 (KHANES IV-2), Kim et al. found that the prevalence of ID in females was 17.2% at 10-14 yr, 24.1% at 15-17 yr, 33.0% at 18-49 yr, and 5.7% at ≥70 yr. In males the prevalence of ID was 8.6% at 10-14 yr, 3.9% at 15-17 yr, and 2.6% at ≥70 yr (
9). This is the only nationwide report of ID in Korean populations. However, a major limitation of this study (
9) is that ID was defined solely by the ferritin level (<15 ng/mL), and there was no analysis of other indicators to assess iron status such as serum iron, total iron-binding capacity and transferrin receptors.
In order to plan interventions to reduce the prevalence of iron deficiency anemia (IDA), particularly in susceptible populations, serum iron and total iron-binding capacity tests were added to KNHANES in 2010 (KNHANES V-1). The goal of the current study was to analyze KHANES V-1 data to accurately determine the prevalence of ID and IDA, identify at-risk groups for IDA and their degree of risk. In addition, we sought to identify novel socioeconomic and nutritional factors for IDA.
RESULTS
Baseline characteristics of the study population
Of a total of 6,758 population, male were 3,041 (45.0%). The distribution of age group was 917 (13.6%) in 10-19 yr, 669 (9.9%) in 20-29 yr, 1,203 (17.8%) in 30-39 yr, 1,133 (16.8%) in 40-49 yr, 1,137 (16.8%) in 50-59 yr, 970 (14.4%) in 60-69 yr, 632 (9.4%) in 70-79 yr, 97 (1.4%) in 80 yr and older. Of 3,717 females, reproductive aged group (15-49 yr) was 1,892 (50.9%). Mean Hb value of current survey population according to age and sex was as follows: 14.0±0.9 in 10-14 yr, 15.2±0.8 in 15-17 yr, 15.5±1.0 in 18-49 yr, 15.2±1.2 in 50-59 yr, 15.2±1.2 in 60-69 yr and 14.3±1.4 in 70 and older for males and 13.4±0.8 in 10-14 yr, 13.1±1.0 in 15-17 yr, 12.8±1.2 in 18-49 yr, 13.2±1.0 in 50-59 yr, 13.2±1.0 in 60-69 yr and 12.9±1.2 in 70 and older for females.
Prevalence of anemia
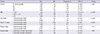
Of the 6,758 study population, 569 were anemic, including 95 males and 474 females. The overall prevalence of anemia in the population ≥10 yr was 7.4% (95% CI, 6.7%-8.1%), with a prevalence of 2.4% (95% CI, 1.6%-3.1%) for males and 12.6% (95% CI, 11.3%-13.9%) for females. The prevalence of anemia according to age and sex was summarized in
Table 1. Relative to age and sex, anemia was least prevalent (0%-1.1%) in males 10-49 yr, but gradually increased to 12.8% by ≥70 yr. Whereas 47.3% of anemic males were ≥70 yr, 61.2% of anemic females were of reproductive age (15-49 yr); 14.4% (95% CI, 12.5%-16.3%), of reproductive-age females were anemic, decreasing by ~half in females 50-69 yr and then increased steadily to 20.7% (95% CI, 15.7%-25.8%) in females ≥70 yr. In adult females, the prevalence of anemia was lowest between 55-59 yr, and highest (24.9%) ≥75 yr. Between 15-54 yr, the prevalence of anemia in females was consistently higher than in males, but there were no gender differences outside of this age range.
Severity and characteristics of anemia
The mean Hb of the 569 anemic individuals was 11.1±1.1 g/dL (range, 6.9-12.9); anemia was mild in 486 (85.4%), moderate in 82 (14.4%), and severe in only 1 (0.2%). The majority (n=421; 74%) were normocytic, 132 (23.2%) were microcytic, and 16 (2.8%) were macrocytic anemia. In the IDA subgroup (see below), mean Hb was 10.6±1.2 (range 6.9-12.9). 130 (45.1%) were microcytic and others were normocytic; and the numbers of patients with mild, moderate, or severe anemia were 210 (72.9%), 77 (26.7%), and 1 (0.3%), respectively.
Prevalence of ID and IDA
The prevalence of ID was 12.1% overall (95% CI, 11.2%-13.0%), with a prevalence of 2.0% (95% CI, 1.3%-2.6%) in males and 22.4% (95% CI, 20.7%-24.2%) in females. The overall prevalence of IDA was 4.3% (95% CI, 3.6%-4.9%), with a prevalence of 0.7% (95% CI, 0.3%-1.0%) in males and 8.0% (95% CI, 6.8%-9.2%) in females. The prevalence of ID and IDA according to age and sex is summarized in
Table 2. The prevalence of ID followed a similar trend to anemia. In males, ID was most common between 10-14 yr and ≥70 yr, IDA prevalence in males was least common between 18-49 yr (0.3%; 95% CI, 0.0%-0.6%). The prevalence of IDA in males increased steadily after age 50 yr, to ~2% between 50-74 yr, and 4% (95% CI, 0.0%-9.7%) ≥75 yr. In females, ID and IDA were most common in the reproductive age group (15-49 yr)-31.4%; 95% CI, 28.9%-33.8%) and 11.5% (95% CI, 9.6%-13.4%), respectively. The prevalence of IDA in females followed a similar trend to anemia, dropping rapidly after age 50 yr, to 5.5% between 50-54 yr, 0.4%-1.3% between 55-74 yr, and then increased to 4.9% in at ≥75 yr. There was no significant gender difference in the prevalence of IDA after age 55 yr.
Proportions of IDA in ID and anemia
In the whole study population, 813 (71 males and 742 females) and 288 (22 males and 266 females) had ID or IDA, respectively. ID does not always lead to anemia: 31.0% of males and 35.8% of female with ID were also anemic. Overall, ~50% of anemias were IDA but there was a marked gender disparity: 56.1% of all anemias in females, and 76.6% in those of reproductive age, were IDA, vs only 23.2% of anemias in males. In females over 50 yr, 52.7% of anemias were IDA between 50-54 yr compared to only 20.0% between 55-59 yr. In the elderly (≥60 yr), only 17.1% of anemias in males and 12.5% in females were IDA.
Influence of menstruation, pregnancy and lactation on ID and IDA
Of all 3,679 females, 3,641 answered questionaires about menstruation, pregnancy and lactation: 1,974 were pre-menopausal; 80 had physiological amenorrhea due to either pregnancy (n =33) or lactation (n=47); 1,538 were post-menopausal or had non-physiological amenorrhea; and 87 were pre-menarcheal females. In current study population, the median ages of menarche and menopause were 14 yr (range 8-28) and 50 yr (range 15-63), respectively. In pre-menarcheal females, 16.4% had ID without anemia. Of the 1,974 premenopausal females, the prevalence of ID or IDA was 32.1% and 11.5%, respectively. Interestingly, only 11.4% and 9.6% of lactating females had either ID or IDA, respectively, whereas 60% of pregnant females had ID vs 25.7% with IDA. Of females in menopause or with non-physiological amenorrhea, 5.3% had ID and 1.7% had IDA (
Table 3).
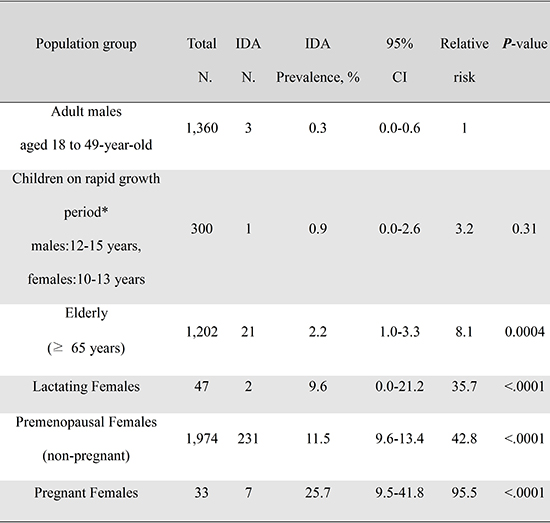
Relative risk of IDA in vulnerable populations
Five vulnerable populations for IDA were selected according to age, gender and physiological state: children during the rapid growth period (12-15 yr in boys; 10-13 yr in girls), adults ≥65 yr, lactating females, premenopausal females, and pregnant females. Compared to the prevalence of IDA in adult males 18-49 yr, the relative risks of IDA in these groups were 3.2, 8.1, 35.7, 42.8, and 95.5, respectively (
Table 4). The group of children during the rapid growth period, which excluded post-menarcheal females, did not have statistically significant risk of IDA.
Prevalence of IDA according to socioeconomic and nutritional factors
Univariate analysis of IDA prevalence in adults (≥19 yr, n=5,906) relative to socioeconomic and nutritional factors showed that IDA was associated with low income, underweight, insufficient dietary iron or vitamin C intake (according to the recommended nutritional intake) (
Table 5). Regarding income, 5.5% of the lowest quartile (Q1) had IDA, vs only 3.2% of top earners (Q4). The prevalence of IDA was 2-4 times higher (11%) in underweight individuals, vs 4.8% and 3.0% for those with normal or obese BMIs, respectively. 7.4% and 2.9% of those taking insufficient or adequate iron intake, respectively, had IDA; similarly, 5.8% and 0.7% of those with insufficient or adequate vitamin C intake, respectively. There were no associations between IDA and protein or total energy intake.
DISCUSSION
Anemia is a public health problem with mild significance in Korean population, according to the WHO proposed classification on the basis of prevalence (
6). The KNHANES estimates indicate that the prevalence of anemia in Koreans is relatively constant (7.4%-8.5%), although KNHANES IV-1 in 2009 reported a prevalence of 9.5% (
8). Based on the WHO Vitamin and Mineral Nutrition Information System for 1993-2005, the national prevalence of anemia vary from 9.1%, 25.6%, and 42.7% in nations with high-, medium- and low-developmental status, respectively (
12). In highly developed countries, anemia is most common in pregnant females (15.5%), females of reproductive age (13.7%; 15-49 yr), children ≤4 yr (12.6%), and adults ≥60 yr (12.2%) (
12).
In KNHANES V-1, the prevalence of anemia during pregnancy was significantly higher than previously reported for developed countries: 38.5% vs 15.5%-22.7%, respectively (
6,
12). Although our survey included only 33 pregnant females, our estimate is in accord with other studies (
13,
14) showing that ~30% of Korean pregnant females are anemic, indicating that anemia remains an import health concern in this population.
Because ID is the major risk factor for anemia, especially in vulnerable populations, precise estimates of the prevalence of ID and IDA are required to plan effective strategies for anemia control. KNHANES V-1, which is based on a stratified, multistage-design random sample of non-institutionalized Korean civilians, has provided the most accurate and representative estimates of the prevalence of ID and IDA. KNHANES V-1 defined ID using serum ferritin and transferrin saturation, followed by statistical analysis after weighting adjustments for each participant. The overall prevalence of ID and IDA were 12.1% and 4.3%, respectively. Although anemia and IDA were not significant health problems for males, children during the rapid growth phase and the elderly were susceptible to ID, a prevalence of 5% and more. Compared with adult males aged 18-49 yr with no risk factors in terms of iron requirement or physiology, the relative risk of IDA was 3.2-fold higher in children during the rapid growth period, without statistical significance, but 8.1-fold higher in adults ≥65 yr. In developed countries, it is important to identify possible gastrointestinal pathologies in individuals with ID but without physiological risk factors, especially the elderly. In our study, of the 21 IDA cases ≥65 yr, 40% had adequate iron intake, which suggests the possibility of pathologic cases. Unfortunately, tests such as stool occult blood test and endoscopic gastrointestinal examination were not conducted in KNHANES.
In all females, 22.4% and 8.0% were ID and IDA, respectively; however, 60% of pregnant females were ID and 25.7% had IDA- a 95.5-fold increase in risk compared to adult males aged 18-49 yr. Eighty percent of pregnant females with anemia had insufficient dietary iron intake, i.e. <24 mg/day, and the compliance of this group to iron supplementation is generally low due to gastrointestinal side effects of the iron supplement. During lactation, only 9.5% of females have IDA, whereas 11.5% of non-pregnant and non-lactating premenopausal females have IDA, which may indicate that lactational amenorrhea compensates for the iron loss via breast milk.
In addition to age, gender and physiological state, socioeconomic and nutritional status were also significant risk factors for IDA: low socioeconomic status, underweight, iron- or vitamin C-poor diets were all associated with IDA.
There were some limitations to our study. First, preschool-aged children, especially toddlers, are vulnerable to IDA but were not included; thus, we may have underestimated the overall prevalence. Second, the KNHANES study design did not include analysis of acute phase proteins such as C-reactive protein (CRP) and α-1 acid glycoprotein (AGP), which would have helped to interpret the data on serum ferritin. Using the same threshold of ferritin to define ID in populations with underlying inflammation or infection would underestimate the prevalence of ID and IDA. Third, ID cannot be defined from a single test result, and our definition by ferritin or transferrin saturation may either over- and under-estimate ID. The specificity of ferritin analysis for ID is reduced by inflammation or infection, and transferrin saturation is highly variable. Other possible indices also have limitations. Erythrocyte protoporphyrin is not a useful marker during infection, and is also complex and costly to measure. Although serum transferrin receptors are not significantly affected by inflammation, infection, age, gender or pregnancy, there is neither a uniform protocol for analysis nor a consensus on a reference range (
6,
15). Although a combination of multiple indices increases the accuracy of an ID diagnosis, resource availability and the cost of a population-based survey need to be considered. Finally, the volume of menstrual bleeding is a major factor for IDA in premenopausal females, but was not included in the KNHANES study. Due to this, it was not possible to analyze the value of socioeconomic and nutritional factors as independent risk factors for IDA in premenopausal females.
However, it is worth noting that our study is the first nationwide analysis of the prevalence of ID and IDA in Koreans, as defined by serum iron and iron-binding capacity and can provide important basic information for planning national health policy to reduce IDA, particularly in susceptible populations. In conclusion, this study based on KNHANES V-1 data revealed that the prevalence of IDA in the Korean population aged ≥10 yr is 0.7% in males and 8.0% in females. Reproductive age females, especially pregnant females, and elderly are high risk groups for IDA. In addition, socioeconomic and nutritional status such as low income, underweight, iron- or vitamin C-poor diets are also significant risk factors for IDA. For populations with defined risk factors in terms of age, gender, physiological state and socioeconomic and nutritional status, national health policy to reduce IDA is needed.














 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download