1. Russell A. Ankylosing spondylitis: history. London: Mosby;2007. p. 1–2.
2. Sieper J, Braun J, Rudwaleit M, Boonen A, Zink A. Ankylosing spondylitis: an overview. Ann Rheum Dis. 2002; 61:iii8–iii18.
3. Boonen A, de Vet H, van der Heijde D, van der Linden S. Work status and its determinants among patients with ankylosing spondylitis: a systematic literature review. J Rheumatol. 2001; 28:1056–1062.
4. Glasnović M. Epidemiology of spondylarthritides. Reumatizam. 2011; 58:24–35.
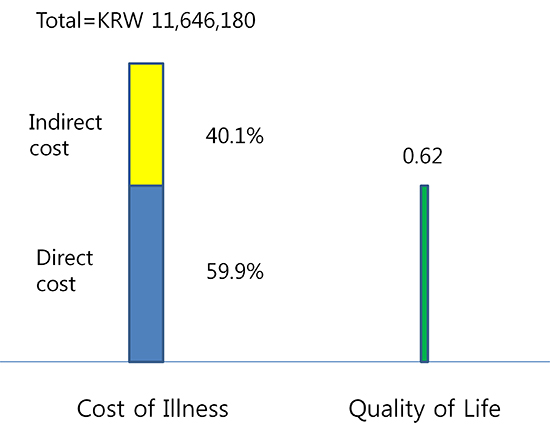
6. Zhu TY, Tam LS, Lee VW, Hwang WW, Li TK, Lee KK, Li EK. Costs and quality of life of patients with ankylosing spondylitis in Hong Kong. Rheumatology (Oxford). 2008; 47:1422–1425.
7. Boonen A, van der Heijde D, Landewé R, Guillemin F, Rutten-van Mölken M, Dougados M, Mielants H, de Vlam K, van der Tempel H, Boesen S, et al. Direct costs of ankylosing spondylitis and its determinants: an analysis among three European countries. Ann Rheum Dis. 2003; 62:732–740.
8. Boonen A, van der Heijde D, Landewé R, Spoorenberg A, Schouten H, Rutten-van Mölken M, Guillemin F, Dougados M, Mielants H, de Vlam K, et al. Work status and productivity costs due to ankylosing spondylitis: comparison of three European countries. Ann Rheum Dis. 2002; 61:429–437.
9. Ward MM. Health-related quality of life in ankylosing spondylitis: a survey of 175 patients. Arthritis Care Res. 1999; 12:247–255.
10. Franke LC, Ament AJ, van de Laar MA, Boonen A, Severens JL. Cost-of-illness of rheumatoid arthritis and ankylosing spondylitis. Clin Exp Rheumatol. 2009; 27:S118–S123.
11. Ara RM, Reynolds AV, Conway P. The cost-effectiveness of etanercept in patients with severe ankylosing spondylitis in the UK. Rheumatology (Oxford). 2007; 46:1338–1344.
12. Bonafede MM, Gandra SR, Watson C, Princic N, Fox KM. Cost per treated patient for etanercept, adalimumab, and infliximab across adult indications: a claims analysis. Adv Ther. 2012; 29:234–248.
13. Louie GH, Reveille JD, Ward MM. Challenges comparing functional limitations in rheumatoid arthritis and ankylosing spondylitis. Clin Exp Rheumatol. 2009; 27:S83–S91.
14. Chorus AM, Miedema HS, Boonen A, van der Linden S. Quality of life and work in patients with rheumatoid arthritis and ankylosing spondylitis of working age. Ann Rheum Dis. 2003; 62:1178–1184.
15. Salaffi F, Carotti M, Gasparini S, Intorcia M, Grassi W. The health-related quality of life in rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis: a comparison with a selected sample of healthy people. Health Qual Life Outcomes. 2009; 7:25.
16. Boonen A, Mau W. The economic burden of disease: comparison between rheumatoid arthritis and ankylosing spondylitis. Clin Exp Rheumatol. 2009; 27:S112–S117.
17. Huscher D, Merkesdal S, Thiele K, Zeidler H, Schneider M, Zink A. German Collaborative Arthritis Centres. Cost of illness in rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis and systemic lupus erythematosus in Germany. Ann Rheum Dis. 2006; 65:1175–1183.
18. Kim TJ, Oh GT, Ju EK, Lee HS, Kim TH, Jun JB, Jung SS, Yu DH, Bae SC. Health-related quality of life in Korean patients with ankylosing spondylitis spndylitis [in Korean]. J Korean Rheum Assoc. 2002; 9:S106–S116.
19. Kim CG, Oh KT, Choe JY, Bae SC. Health-related quality of life Korean patients with rheumatoid arthritis. J Korean Rheum Assoc. 2002; 9:S60–S72.
20. Lee TJ, Park BH, Son HK, Song R, Shin KC, Lee EB, Song YW. Cost of illness and quality of life of patients with rheumatoid arthritis in South Korea. Value Health. 2012; 15:S43–S49.
21. Van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis: a proposal for modification of the New York criteria. Arthritis Rheum. 1984; 27:361–368.
22. Hochberg MC, Chang RW, Dwosh I, Lindsey S, Pincus T, Wolfe F. The American College of Rheumatology 1991 revised criteria for the classification of global functional status in rheumatoid arthritis. Arthritis Rheum. 1992; 35:498–502.
23. Merkesdal S, Ruof J, Huelsemann JL, Schoeffski O, Maetzel A, Mau W, Zeidler H. Development of a matrix of cost domains in economic evaluation of rheumatoid arthritis. J Rheumatol. 2001; 28:657–661.
24. Drummund MF, Sculpher MJ, Torrance GW, O'Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press;2005.
25. Korean Statistical Information Service. accessed on 30 April 2010. Available at
http://www.kosis.kr.
26. Kang EJ, Shin HS, Park HJ, Jo MW, Kim NY. A valuation of health status using EQ-5D. Korean J Health Econ Policy. 2006; 12:19–43.
27. Zink A, Braun J, Listing J, Wollenhaupt J. Disability and handicap in rheumatoid arthritis and ankylosing spondylitis: results from the German rheumatological database: German Collaborative Arthritis Centers. J Rheumatol. 2000; 27:613–622.
28. Kojima M, Kojima T, Ishiguro N, Oguchi T, Oba M, Tsuchiya H, Sugiura F, Furukawa TA, Suzuki S, Tokudome S. Psychosocial factors, disease status, and quality of life in patients with rheumatoid arthritis. J Psychosom Res. 2009; 67:425–431.
29. Alishiri GH, Bayat N, Fathi Ashtiani A, Tavallaii SA, Assari S, Moharamzad Y. Logistic regression models for predicting physical and mental health-related quality of life in rheumatoid arthritis patients. Mod Rheumatol. 2008; 18:601–608.
30. Ariza-Ariza R, Hernández-Cruz B, Navarro-Sarabia F. Physical function and health-related quality of life of Spanish patients with ankylosing spondylitis. Arthritis Rheum. 2003; 49:483–487.
31. Ozdemir O. Quality of life in patients with ankylosing spondylitis: relationships with spinal mobility, disease activity and functional status. Rheumatol Int. 2011; 31:605–610.






 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download