Abstract
Testicular torsion is a surgical emergency in the field of urology. Knowledge of the epidemiology and pathophysiology is significant to an urologist. However, the epidemiology of testicular torsion in Korea has not been studied. We performed a nationwide epidemiological study to improve knowledge of the epidemiology of testicular torsion. From 2006-2011, the Korean Urologic Association began the patient registry service. The annual number of patients with testicular torsion from 2006 to 2011 were 225, 250, 271, 277, 345, and 210, respectively. The overall incidence of testicular torsion in males was 1.1 per 100,000; However, the incidence in men less than 25 yr old was 2.9 per 100,000. Adolescents showed the highest incidence. Total testicular salvage rate was 75.7% in this survey. There was no geographic difference of testicular salvage rate. Minimizing the possibility of orchiectomy for testicular torsion is important to improve public awareness to expedite presentation and provider education to improve diagnosis and surgery.
Testicular torsion is a surgical emergency in the field of urology. This condition can cause subfertility or infertility, and psychological trauma in men (1, 2). To prevent ischemic necrosis, treatment should be done as soon as possible. If the testicle can be detorsed within 6 hr, over 90% of patients experience testicular salvage, while success decreases to < 10% after 24 hr (3). Several factors delay treatment and orchiectomy. Patients or their parents hesitate to consult doctors for a genital condition because of lack of medical knowledge. Distance from home to a medical center and the economic status of the patients' family may affect the delaying treatment (4).
Etiology of testicular torsion is known as 'bell clapper' anatomical deformity (5). A family history of testicular torsion has been described as one of the etiology (6). Weather changes may affect the occurrence of testicular torsion (7). Physician's knowledge of the epidemiology and pathophysiology is important. Nationwide studies in the United States and Taiwan reported incidences of testicular torsion in males aged 1-25 yr as 4.5 cases per 100,000 men per year overall, and 3.5 cases per 100,000 men per year in men < 25 yr of age (8, 9). However, information on Koreans is lacking. We performed a nationwide epidemiological study on the epidemiology of testicular torsion in Korean men.
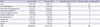
The Korean Urologic Association operated the UroPDS (Urologic Partitioned Data Set) patient registry from 2006 to 2011. All residency training hospitals recorded inpatient information. UroPDS data consists of age, diagnosis, kind of surgery, time of admission and time of discharge. To calculate the incidence rate of testicular torsion in the general population, the total population was cited from the Korean Statistical Information Service. A national census was made in 2010; and the estimated population was determined every year from 2006 to 2011. The average incidence of 6 yr was calculated by dividing the total population of males for the 6 yr by the total number of patients. Testicular salvage rate was calculated in patients who had undergone orchiopexy divided by the total number of patients. Age and regional information was included to analyze the influence of testicular salvage rate. Age group was divided as infancy (< 1 yr), children (1-11 yr), adolescents (12-20 yr), and adults (< 20 yr) (10). The geographic regions were divided into 10 administrative zones. Each urologic residency training hospital was classified by region. Population density was used to reflect urbanization levels (Table 1).
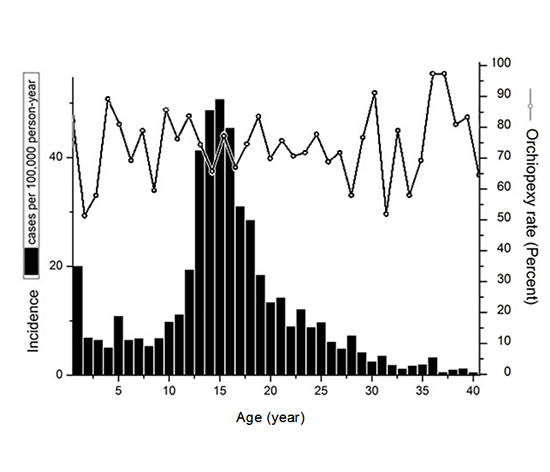
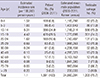
From January 2006 to December 2011, 1,591 cases were included in UroPDS by a keyword search using 'testicular torsion'. By year, the number of patients with testicular torsion from 2006 to 2011 was 225, 254, 272, 280, 346, and 213, respectively. The incidence of testicular torsion in male was 1.1 per 100,000 and 2.9 per 100,000 in males <25 yr old. There were two peaks of incidence at infancy and adolescent. Adolescents were the most frequent incidence age group per 100,000. Incidence rate was decreased after the middle age, the disease can occur at any age (Table 2).
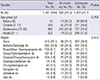
A total of 1,250 patients underwent orchiopexy. Total testicular salvage rate was 75.7% overall and 75.4% for those <25 yr of age. Testicular salvage rate in infancy was 65.9%, which was lower than any other age group, but not statistically significant. Geographic incidence also was not a statistically significant factor (Table 3).
Testicular torsion is a well known emergency in urology and can occur at any age. Our study shows that the incidence was 2.9 cases per 100,000 person years of males <25 yr of age and 1.1 cases per 100,000 person years at all ages. The incidence of testicular torsion in males 1-25 yr of age has been reported as 4.5 cases per 100,000 male subjects per year in the United States (8). A US study indicated that the estimated yearly incidence of testicular torsion for males <18 yr of age was 3.8 per 100,000 (4). Another nationwide study in Taiwan reported 3.5 cases per 100,000 person years for males <25 yr of age (9). An incidence of 1.4 cases per 100,000 men was reported in Brazil (11). Several other studies reported a similar incidence rate. Two peaks of incidence were reported when plotted by age group. (4). We found a similar incidence by with peaks in infancy and adolescence. Both peaks were the time of appearance of primary and secondary sex characteristics. It may reflect the clinical distinction between extravaginal torsion in newborns and infants and children (12). Many nationwide studies have been on the basis of the statistcs of the country and are classified based on International Classification of Disease (ICD). With these methods, there is a possibility of miscoding if symptoms are similar with testicular torsion. For example, miscoding can occur when diagnosis changes after scrotal exploration. In the case of the UroPDS data, a doctor needed to enter the data directly after final diagnosis. This has an advantage of minimizing error.
Immediate surgical correction could save testicular damage in patient with testicular torsion. Most testicular torsion patients visit a hospital presenting with scrotal pain, swelling, and erythema (13). Surgeons will determine whether to remove the testicle. As a general rule, the decision depends on testicular color when a physician detorses the testis in the surgical field. A continuous black color, which means irreversible necrosis, is the most indicative of the need for testicle removal. Delayed diagnosis and treatment can increase the rate of testicular removal. In this study, total testicular salvage rate was 75.7% in Korea (14). In the United States, four studies reported testicular torsion and testicular salvage rate. Cost et al. (14) reported a 68.1% salvage rate from patients aged 1-17 yr old and Zhao et al. (4) reported 58.1% salvage rate in patients <18 yr of age. Mansbach et al. (8) reported a 66.6% salvage rate in patients ≤25 yr of age. Cummings et al. (15) studied testicular salvage rate by ages of 17-20 and 21-34 yr. The salvage rate differed with 70.3%, of testes salvaged in the younger group versus only 41% in the older group. In Taiwan, Huang et al. (9) reported a rate of 74.4% in patients <25 yr of age. The testicular salvage rate is better in Korea than other countries a little. This means that diagnosis and treatment was quick. Testicular salvage in torsion depends on timely presentation, diagnosis, and surgical intervention. In other time sensitive disease, such as appendicitis and myocardial infarction, efforts to improve outcomes have traditionally focused on public awareness to expedite presentation and provider education to hasten diagnosis (16, 17). Rate of testicular salvage will be increased in a similar way. Notably, there is similar testis salvage rate between rural and urban area in Korea. In the US, Zhao et al. (4) reported that age, insurance type, and living area influence testicular salvage rate. This better salvage rate in Korea is presumed to be due to the result of small size of territory, dense distribution of hospitals, and National Health Insurance of Korea (NHI). The NHI system initially offered plans with low premiums, low benefits, and low doctors' fees to contribute to eliminating inequities based on socioeconomic status. This approach improved access to medical services, eliminated gaps between urban and rural areas and between different classes with respect to the use of services (18). In the future, Korean urologists will likely decline due to decreased urology residents in Korea, so similar longitudinal study design will be interesting in the future.
The study had some limitations. First, the data source of UroPDS is not covering the whole population. All patients' data were recorded by surgeons directly in UroPDS. Only training hospitals were included in UroPDS program. There is a possibility of data loss due to record omission. Thus, the actual incidence rate would be a little higher than our results. But emergent surgery of pediatric testicular torsion is difficult at non-training hospital. In fact, the incidence is not far from foreign country. Second, the geographic districts were divided by hospital address. This variable is involved to evaluate influence of medical accessibility but it is hard to reflect each patient's medical accessibility.
In conclusion, this nationwide study addresses an important clinical issue. The incidence of testicular torsion in males aged <26 yr was 2.9 cases per 100,000 men per year. Approximately 75.7% patients with testicular torsion finally received orchiopexy in Korea. To minimize the possibility of orchiectomy for testicular torsion, it is important to improve public awareness to expedite presentation and provider education to hasten diagnosis and surgery.
References
1. Reyes JG, Farias JG, Henríquez-Olavarrieta S, Madrid E, Parraga M, Zepeda AB, Moreno RD. The hypoxic testicle: physiology and pathophysiology. Oxid Med Cell Longev. 2012; 2012:929285.
2. Bodiwala D, Summerton DJ, Terry TR. Testicular prostheses: development and modern usage. Ann R Coll Surg Engl. 2007; 89:349–353.
3. Sessions AE, Rabinowitz R, Hulbert WC, Goldstein MM, Mevorach RA. Testicular torsion: direction, degree, duration and disinformation. J Urol. 2003; 169:663–665.
4. Zhao LC, Lautz TB, Meeks JJ, Maizels M. Pediatric testicular torsion epidemiology using a national database: incidence, risk of orchiectomy and possible measures toward improving the quality of care. J Urol. 2011; 186:2009–2013.
5. Caesar RE, Kaplan GW. Incidence of the bell-clapper deformity in an autopsy series. Urology. 1994; 44:114–116.
6. Cubillos J, Palmer JS, Friedman SC, Freyle J, Lowe FC, Palmer LS. Familial testicular torsion. J Urol. 2011; 185:2469–2472.
7. Chen JS, Lin YM, Yang WH. Diurnal temperature change is associated with testicular torsion: a nationwide, population based study in Taiwan. J Urol. 2013; 190:228–232.
8. Mansbach JM, Forbes P, Peters C. Testicular torsion and risk factors for orchiectomy. Arch Pediatr Adolesc Med. 2005; 159:1167–1171.
9. Huang WY, Chen YF, Chang HC, Yang TK, Hsieh JT, Huang KH. The incidence rate and characteristics in patients with testicular torsion: a nationwide, population-based study. Acta Paediatr. 2013; 102:e363–e367.
10. Feigelman S. Overview and Assessment of Variability. In : Kliegman R, Stanton B, St Geme JW, Schor N, Behrman R, editors. Nelson textbook of pediatrics. 19th ed. Philadephia, PA: Saunders;2011. p. 26.
11. Korkes F, Cabral PR, Alves CD, Savioli ML, Pompeo AC. Testicular torsion and weather conditions: analysis of 21,289 cases in Brazil. Int Braz J Urol. 2012; 38:222–228. discussion 8-9.
12. Mano R, Livne PM, Nevo A, Sivan B, Ben-Meir D. Testicular torsion in the first year of life: characteristics and treatment outcome. Urology. 2013; 82:1132–1137.
13. Boettcher M, Krebs T, Bergholz R, Wenke K, Aronson D, Reinshagen K. Clinical and sonographic features predict testicular torsion in children: a prospective study. BJU Int. 2013; 112:1201–1206.
14. Cost NG, Bush NC, Barber TD, Huang R, Baker LA. Pediatric testicular torsion: demographics of national orchiopexy versus orchiectomy rates. J Urol. 2011; 185:2459–2463.
15. Cummings JM, Boullier JA, Sekhon D, Bose K. Adult testicular torsion. J Urol. 2002; 167:2109–2110.
16. Ponsky TA, Huang ZJ, Kittle K, Eichelberger MR, Gilbert JC, Brody F, Newman KD. Hospital- and patient-level characteristics and the risk of appendiceal rupture and negative appendectomy in children. JAMA. 2004; 292:1977–1982.
17. Garceau P, Déry JP, Lachance P, Grenier S, Rodés-Cabau J, Barbeau G, Bertrand OF, Gleeton O, Larose E, Nguyen CM, et al. Treatment delays in patients undergoing primary percutaneous coronary intervention for ST elevation myocardial infarction at the Quebec Heart and Lung Institute. Can J Cardiol. 2007; 23:53B–57B.
18. Kim KH, Park EC, Hahm MI. The gap between physicians and the public in satisfaction with the National Health Insurance system in Korea. J Korean Med Sci. 2012; 27:579–585.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download