INTRODUCTION
The healthcare delivery system in Korea is broken. In particular, the patient referral system does not function well and has almost completely disintegrated. In theory, if a patient wants to see a doctor in a hospital, the patient should receive a referral slip from a physician in a local clinic. However, in reality, Korean people can go to any medical institution, not only clinics in their community but also hospital-level institutions, as their first contact point (
1,
2). In other words, Korean people enjoy full freedom of choice in selecting doctors or hospitals. Additionally, unlike in Western countries, physicians' clinics can possess inpatient facilities and hospitals can operate large-scale outpatient care units (
3,
4). This creates a competitive relationship between local clinics and hospitals, rather than to be collaborative (
4,
5). This competition has been worsening through a "medical arms race" in which physicians' clinics are purchasing expensive medical equipment such as CT and MRI machines while hospitals are markedly enhancing outpatient services (
4,
5). Healthcare utilization has been distorted and primary care weakened because of patients' almost unlimited freedom in choosing doctors, the absence of formal gatekeepers, undifferentiated and often duplicated functions between hospitals and clinics, and excessive competition between various service levels. In regard to this, the Organization for Economic Co-operation and Development (OECD) recently recommended that Korea needs a new strategy for strengthening and invigorating primary care. The recommended system should transition from an acute care centered healthcare system to a system that confronts the specific needs of an ageing population and patients with chronic conditions (
6).
By increasing the coinsurance rate, the Korean Government has made efforts to encourage patients with minor or simple diseases to utilize local clinics in their community instead of using hospitals. For example, the coinsurance rate for using outpatient services at tertiary hospitals has increased from 50% to 60% since July 2009. Also, the outpatient prescription drug coinsurance rates for 52 simple and minor diseases, when managed by tertiary and general hospitals, has increased from 30% to 40% and 50% since October 2011 (
7). However, these policies may result in unintended consequences such as discouraging the utilization of healthcare services among underprivileged individuals or patients who truly require hospital-level healthcare services (
8). Regarding policies to reverse the flow of patients with simple or minor diseases from hospitals to local clinics, hospitals and practicing physicians have exceptionally conflicting points of view. According to the position statement of the Korean Hospital Association (KHA), there are a very limited number of patients utilizing tertiary teaching hospitals for genuinely simple or minor diseases. The KHA asserts that patients using outpatient services in tertiary hospitals are mostly severely ill patients (i.e., cancer patients or elderly patients) and patients with co-morbidities that should be carefully treated and managed at the hospital level. KHA argues that the majority of patients using outpatient clinics in tertiary hospitals are in the course of treatment for severe diseases and therefore, even though some are also receiving services for simple or minor comorbidities, their use of tertiary teaching hospitals should be granted for continuity of care. Also, KHA emphasizes that there are very few patients who have very simple or minor diseases, such as the common cold, utilizing outpatient hospital services. On the other hand, the Korean Medical Practitioners Association (KMPA), representing physicians in local clinics, rebutted the assertion by KHA. KMPA asserted that many outpatients with simple or minor diseases who should be treated in local clinics are utilizing hospital-level institutions, resulting in a distorted healthcare delivery system and wasting expenditure on unnecessary healthcare services.
In order to redirect the flow of patients with simple or minor diseases from hospitals to primary care clinics, the first step is to estimate how many patients unnecessarily utilize hospitals. From the list of 52 simple or minor diseases designated by the Korean Government, the authors decided to begin with chronic diseases such as hypertension (HTN), diabetes mellitus (DM), and hyperlipidemia (HL). Therefore, this study aims to investigate the volume of unnecessarily utilized hospital outpatient services among patients with a single chronic disease and to estimate the total cost resulting from inappropriate utilization.
MATERIALS AND METHODS
Data source
This research used the 2009 National Inpatient Sample (NIS) database published by the Health Insurance Review and Assessment Service (HIRA) in Korea. HIRA carried out reviews on representativeness, reliability and validity of sample data regarding beneficiaries' information about procedures, diagnosis, prescriptions and demographical characteristics (
9). The NIS database is a representative sample of the HIRA claim data, including 13% of the yearly inpatient claims (about 700 thousands inpatients) and 1% of yearly outpatient claims (about 400 thousands outpatients). The 2009 NIS contains a total sample of 27,320,505 claims from outpatient services. Each claim or patient in the database is designed to represent 100 claims or 100 patients.
Operational definitions of chronic disease without complications
In this study, we operationally defined three chronic diseases without complication using the International Classification of Diseases-10th Revision (ICD-10): Hypertension without complications is referred to only by I10; diabetes mellitus without complications is represented by E10, E10.9, E11, E11.9, E13, E13.9, E14, or E14.9; and hyperlipidemia without complications include E78, E78.0, E78.1, E78.2, E78.3, E78.4, or E78.5.
Patient selection process
The authors decided to apply strict standards to identify the volume of unnecessarily utilized outpatient services in hospitals among patients with a single chronic disease. Using the 2009 NIS 20 table (the dataset containing general information about claim cases), 4,808,695 claims were selected which did not have a history of a hospital admission in 2009. Secondly, the NIS 20 table with the extracted claims was merged with the NIS 40 table (the dataset containing all the diagnostic codes for each claim) to clearly display the corresponding ICD-10 diagnostic codes. Thirdly, 1,608,166 claims that included any diagnostic codes for hypertension, diabetes mellitus, and hyperlipidemia were selected from the 4,808,695 claims. Fourthly, bundled claims (a medical institution can submit a single file of merged claims, called "bundled claims") were divided into the single, original claims. There were 1,698,197 cases of single claims. Finally, 579,809 cases were selected based on the above operationally defined ICD-10 codes regarding hypertension without complication, diabetes without complication and hyperlipidemia without complication. This resulted in 88,842 patients stratified by type of medical institution. That is, the study population included 579,809 claims for 88,842 patients and represented a total, nation-wide population of 57,980,900 claims and 8,884,200 patients because each one claim or patient was designed to represent 100 claims or 100 patients in the 2009 NIS database. This study used the denominators of 57,980,900 claims and 8,884,200 patients (
Fig. 1).
Data analysis
In order to assess the necessity of utilizing hospital outpatient services by patients with a single chronic disease without complication, the authors employed the Charlson Comorbidity Index (CCI), which contains the following 17 conditions or diseases: AIDS/HIV (B20.x-B22.x), cerebrovascular disease (I69.x), congestive heart failure (I50.x), chronic pulmonary disease (J41.x-J47.x, J60.x-J66.x), dementia (F00.x-F02.x), diabetes without chronic complication (E10, E10.9, E11, E11.9, E13, E13.9, E14, E14.9), diabetes with chronic complication (E10.2-E10.4, E11.2-E11.4, E13.2-E13.4, E14.2-E14.4), hemiplegia or paraplegia (G81.x, G82.0-G82.2), mild liver disease (K70.3, K71.7, K73.x, K74.3-K74.6), moderate or severe liver disease (K72.1, K72.9, K76.6, K76.7), any malignancy, including leukemia and lymphoma (C00.x-C26.x, C30.x-C34.x, C37.x-C41.x, C45.x-C58.x, C88.3, C88.7, C88.9, C90.0, C90.1, C91.x-C93.x, C94.0-C94.3, C94.5, C94.7, C95.x, C96.x) metastatic solid tumor (C77.x-C79.x), myocardial infarction (I25.2), peripheral vascular disease (I71.x, I73.9, Z95.8, Z95.9), peptic ulcer disease (K25.4-K25.7, K26.4-K26.7, K27.4-K27.7, K28.4-K28.7), rheumatologic disease (M05.x, M06.0, M32.x, M33.2, M34.x, M35.3), and renal disease (N18.x) (
10). The CCI is a well validated and commonly used risk adjustment tool. CCI is a composite score calculated by summating the weighted relative risks of 1-yr mortality of the 17 conditions (
11). The authors agreed that if a patient has a single chronic disease without complication and a CCI score greater than 1, the hospital visit would be considered "necessary hospital outpatient utilization". That is, in the case of a CCI score of 0 (no comorbidity with the above 17 conditions), a patient visit to a hospital level institution would be defined as "unnecessary hospital outpatient utilization".
We analyzed outpatient utilization for three chronic conditions without complication, operationally defined based on ICD-10. If a patient had multiple chronic conditions (i.e., a patient had HTN and DM), the case was excluded from the analysis. Therefore, the analyses were performed based on each single chronic disease without complication (HTN, DM, and HL), according to CCI (score=0 vs. score >=1) and type of medical institution (tertiary hospital, general hospital, hospital, and clinic). The analyses were conducted using claim based datasets, therefore the unit of analysis was a claim for each outpatient visit. Each single chronic disease had a different number of claims: HTN (205,411 claims), DM (25,507 claims), and HL (49,304 claims), respectively.
We analyzed the utilization pattern and healthcare expenditure according to type of institution and CCI. Total annual healthcare costs and annual average costs per visit were also analyzed by type of institution and CCI. Healthcare costs (or expenditure) were analyzed by total claim costs; costs reimbursed from the National Health Insurance Service in Korea (NHIS); and out-of-pocket (OOP) money paid by a beneficiary. All costs are presented in United States dollars (USD), with an exchange rate of 1 USD equal to 1,164.5 Korean won (average annual rate in 2009). In order to identify the difference in outpatient utilization by the type of healthcare institution and the CCI score, chi-square for trend tests were performed. ANOVA and Tukey's B (ad hoc test) test were conducted to identity the differences in annual average healthcare costs by type of healthcare institution and CCI score. Lastly, we simulated the change of healthcare expenditure in terms of total claim costs, the burden of NHIS, and OOP if patients with a CCI score of 0 who are utilizing hospital level institutions were redirected to clinics by 10%, 20%, 50%, and 100%. All the analyses were completed using SAS, version 9.2 (SAS Institute, Inc., Cary, NC, USA) and SPSS 20 (IBM Corporation, Armonk, NY, USA). All statistical tests were two-sided and a P value <0.05 was considered statistically significant.
Ethics statement
This study was exempted from the approval by the institutional review board of Seoul National University Boramae Medical Center (IRB No. 07-2013-2).
DISCUSSION
In most European countries, the roles and functions between hospital level institutions and local clinics are clearly designated. Thus, the relationship between hospitals and local clinics is collaborative, not competitive. For example, it is common for doctors in local clinics and hospitals to refer patients to each other, based on the patients' needs (
6,
12). In contrast, the level of competition between hospitals and clinics in Korea is very high because of the undifferentiated roles and functions among each type of healthcare institution. Hospitals and clinics take great measures to increase the number of individuals who use their services; by even inviting patients with simple diseases to their institution. However, as noted previously, KHA denies the fact that hospitals are currently seeing patients with minor diseases while doctors with private clinics dispute this fact and argue that hospitals are taking away their patients. Neither institution is able to come to an agreement, and for this reason, it is important to investigate the reality of how many patients with a single chronic disease without complications are currently utilizing hospitals.
To investigate this matter we adopted a strict methodological approach in order for both institutions and clinics to accept the results. This was done by excluding all patients who had a history of any type of hospital admission in 2009 from the analysis and by considering the comorbidity by CCI score. For example, a patient with hypertension without complication who had an admission in 2009 would have been excluded, thus only patients with a CCI score of 0 were included. Such an approach could prompt debates because we excluded all patients with an admission history and only included patients with a CCI score of 0. Nevertheless, the reason we took such a radical and conservative approach, despite the risk of underestimating of the amount of unnecessary hospital outpatient utilization, was to encourage agreement from hospital level institutions.
Remarkable results were drawn from this research. Approximately 85% of patients with HTN and HL without complications and over 90% of patients with DM without complications unnecessarily utilized outpatient services at hospital level institutions. Although we used a methodology that was more favorable toward the hospital level institutions, the results clearly indicate the problem that patients who should be seen in clinics are actually being seen in hospitals. In another respect, this result could be interpreted as hospitals taking away 18.7% of HTN patients, 18.6% of DM patients and 31.6% of HL patients from clinics (number of visits with a CCI score of 0 using hospital type medical institutions divided by the total number of visits with a CCI score of 0) (
Table 1). Thus, these patients should have visited local clinics. When we converted to number of claims the following results were shown: 3,261 thousands of HTN patients, 438 thousands of DM patients and 1,310 thousands of HL patients. The estimated number of HTN patients without complications was 17,447 thousands and 18.7% (3,261 thousands) of the patients were treated by hospitals; the estimated number of DM patients without complications was 2,353 thousands and 18.6% (438 thousands) of these patients were treated by hospitals; and the estimated number of HTN patients without complications was 4,142 thousands and 31.6% (1,310 thousands) were treated by hospitals. Thus, the local clinic physicians' assertions that the hospital is taking away their patients could be true.
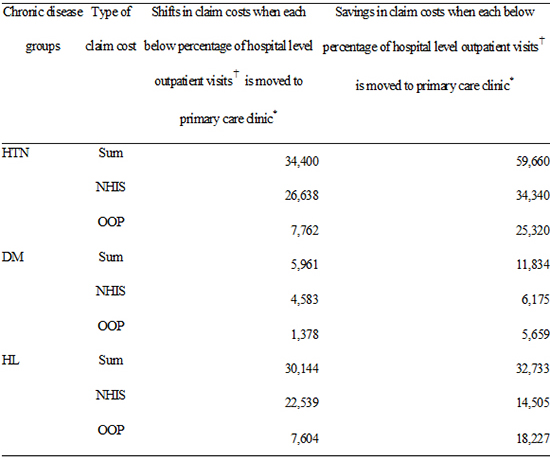
The seriousness of this matter was further supported when the volume of unnecessary hospital outpatient utilization claims were converted to monetary values. The healthcare expenditures due to unnecessary hospital outpatient utilization were estimated at: 94,058 thousands USD for HTN (38.6% of total expenditure); 17,795 thousands USD for DM (40.6% of total expenditure) and 62,876 thousands USD for HL (49.1% of total expenditure). However, these numbers may be an underestimation as the methodology we used was very conservative and radical, therefore these results may be larger in reality. When based on the number of claims, hospitals accounted for 18.7% (HTN), 18.6% (DM) and 31.6% (HL), but on the other hand, when based on the cost of claims; hospitals received 38.0% (HTN), 40.6% (DM) and 49.1% (HL). This phenomenon results from the average cost disparity between the different types of healthcare institutions. For example, payment to the clinic for treatment of HTN is 10.5 USD, however, if the same patient is treated in the tertiary hospital, the payment is 4.5 times higher, for a total of 47.1 USD. Similarly, payment for the treatment of DM in the clinic is 13.6 USD but the payment is 5.5 times more, 74.5 USD, if a patient is treated in the tertiary hospital. The payment for HL in the clinic is 23.0 USD, but the payment is 2.8 times more, 64.4 USD, if the patient is treated in the tertiary hospital (
Table 2).
The size and volume of extra costs were calculated and the authors further calculated how much could be saved when redirecting patient flow from hospitals to primary care. In theory, these savings would be equal to the additional healthcare costs associated with unnecessary hospital outpatient utilization. This could be calculated by subtracting the estimated cost of all patients utilizing primary care from the total health care costs generated by unnecessary hospital outpatient utilization. The authors found that a significant amount of inefficient healthcare costs were being spent on unnecessary hospital outpatient utilization: 59,660 thousands USD for HTN (NHIS, 34,340 thousands USD; OOP, 25,320 thousands USD), 11,834 thousands USD for DM (NHIS, 6,175 thousands USD; OOP, 5,659 thousands USD) and 32,733 thousands USD for HL (NHIS, 14,505 thousands USD; OOP, 18,227 thousands USD).
This research only focused on 3 diseases from the list of 52 simple or minor diseases designated by the Korean Government, therefore the total amount of unnecessary healthcare costs would be much higher if all 52 diseases were investigated. Additionally, it is definitive that the numbers calculated are an underestimation as these healthcare costs do not included the costs not covered by health insurance. For example, if a patient goes to a tertiary hospital and designates a certain doctor because they are well-known, the patient will pay 100% of the doctor's consultation fee, meaning that the burden will be on the patient. Therefore, in reality, there is an existence of hidden costs which is not being reported to the NHIS.
What efforts should be conducted to improve Korea's broken healthcare system? Unfortunately, this cannot be solved easily because the healthcare delivery system is distorted and the intertwined interests of stakeholders complicates the situation. However, the Korean Government is trying to implement policies to improve the patient flow from hospitals to clinics (
7). Firstly, the Government designated the 52 simple or minor diseases and recommended that patients in this category see a clinic level physician, if possible. Secondly, patients in this category who choose to go to tertiary hospitals or general hospitals are required to pay the increased co-insurance rate, including the medical fee (increased from 50% to 60%) and prescription fee (increased from 30% to 50%, in the case of tertiary hospitals). Thirdly, in April 2012, the Government launched the 'Chronic Disease Management Programme for Primary Care.' Under this program, the Government reduced their co-insurance rates to 20% from 30% for patients with HTN or DM who receive continuous care from a primary clinic and also provides incentives to doctors who participate in the programme (
7). Even though the Government has implemented these policies with good will, certain unintended consequences can occur. For example, it is reasonable a patient with both cancer and HTN would be followed simultaneously for both conditions by the same hospital doctor. However, in this case, the patient would pay more because the co-insurance rate to treat HTN by a hospital doctor has increased. These are the types of cases that hospitals argue they are not taking away clinics' patients who have single or minor diseases however, as noted above, physicians who have private clinics do not agree with this. Therefore one of the main purposes of this study was to identify the current problem with the 52 diseases category and make a protocol to clearly define the category by excluding patients with an admission history and patients with a CCI score of more than 1 to clearly define the term 'simple or minor diseases'. The motivation for this research was to find a new way of selecting patients who should be in the category of simple or minor diseases. Clinics' physicians could be dissatisfied with this method due to the strictness of categorizing patients but hospitals will not be able to easily deny the validity of this research.
All stakeholders cannot deny the principle that simple or minor diseases should be treated in the primary care setting. However, the reality in Korea is that hospitals and clinics are competing over the possession of patients, which is evidence of the broken healthcare delivery system. This research found that approximately 85% of hospital utilizations were unnecessary, resulting in significant, inefficient healthcare costs and burdening both the NHIS and patients. Therefore, the Korean Government should revise the current 52 simple or minor diseases' category in order to reflect reality and find a compromise to stakeholder concerns. Also, the Government should investigate how many patients with each of the 52 single or minor diseases utilize hospitals. Furthermore, a more sophisticated policy should be prepared to reverse the patient flow from hospitals to the primary care setting.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download