Abstract
We aimed to investigate that complete revascularization (CR) would be associated with a decreased mortality in patients with multivessel disease (MVD) and reduced left ventricular ejection fraction (LVEF). We enrolled a total of 263 patients with MVD and LVEF <50% who had undergone percutaneous coronary intervention with drug-eluting stent between March 2003 and December 2010. We compared major adverse cardiac and cerebrovascular accident (MACCE) including all-cause death, myocardial infarction, any revascularization, and cerebrovascular accident between CR and incomplete revascularization (IR). CR was achieved in 150 patients. During median follow-up of 40 months, MACCE occurred in 52 (34.7%) patients in the CR group versus 51 (45.1%) patients in the IR group (P=0.06). After a Cox regression model with inverse-probability-of-treatment-weighting using propensity score, the incidence of MACCE of the CR group were lower than those of the IR group (34.7% vs. 45.1%; adjusted hazard ratio [HR], 0.65; 95% confidence interval [CI], 0.44-0.95, P=0.03). The rate of all-cause death was significantly lower in patients with CR than in those with IR (adjusted HR, 0.48; 95% CI, 0.29-0.80, P<0.01). In conclusion, the achievement of CR with drug-eluting stent reduces long-term MACCE in patients with MVD and reduced LVEF.
Several surgical studies have shown that incomplete revascularization (IR) in patients undergoing coronary artery bypass graft surgery carries a worse prognosis with higher rates of mortality, myocardial infarction (MI) and angina (1,2,3). With respect to percutaneous coronary intervention (PCI), previous studies investigating the impact of complete revascularization (CR) in patients with multivessel disease (MVD) have shown the inconsistent results in the bare metal stent era (4,5,6,7,8). In drug-eluting stents (DES) era, majority of reports demonstrated that restenosis had been reduced remarkably and CR improved clinical outcomes than IR (9,10,11). However, long-term follow up study is rare and it has not been clearly determined which revascularization strategy is better, particularly in patients with left ventricular systolic dysfunction. We evaluated the impact of CR on long-term outcomes of PCI with DES implantation in patients with MVD and reduced left ventricular ejection fraction (LVEF).
This was a single-center, observational study comparing the clinical outcomes of CR and IR performed in patients with chronic left ventricular systolic dysfunction. The patients were recruited from the cardiovascular catheterization database of Samsung Medical Center (Seoul, Korea) (12). The database was recorded prospectively by PCI registry research coordinators. Baseline characteristics, angiographic and procedural data, and outcome data was recorded at the time of PCI and clinical follow up data were added regularly. Additional information was obtained from medical records and telephone contacts, if necessary. Consecutive patients who were newly diagnosed as having MVD with LVEF <50% and who had undergone PCI with DES between March 2003 and December 2010 were identified from the registry. Patients who underwent PCI due to acute myocardial infarction, who had single vessel disease or a history of coronary artery bypass graft surgery were excluded.
MVD was defined as coronary lesions with ≥50% diameter stenosis by quantitative coronary analysis in at least two of the three major epicardial coronary arteries or their major branches (13). CR was defined as the absence of ≥70% diameter stenosis in major epicardial coronary arteries or their branches with a diameter ≥2.0 mm after successful PCI (14). The angiographic SYNergy between PCI with TAXus and cardiac surgery (SYNTAX) score was used to assess the complexity of coronary artery disease (13).
Participants were divided into 2 groups according to the completeness of revascularization. The primary outcome was major adverse cardiac and cerebrovascular event (MACCE), a composite of all-cause death, MI, any revascularization, and cerebrovascular accident during follow-up. Secondary outcomes included all-cause death, cardiac death, MI, any revascularization with PCI or coronary artery bypass grafting. All-cause death was defined as any death during or after the index procedure and was considered to be cardiac in origin unless a definite non-cardiac cause could be established. MI was defined as symptoms with new electrocardiographic changes compatible with MI or cardiac markers at least twice the upper limit of normal. Any revascularization was defined as revascularization on either target or non-target vessels.
Baseline differences in clinical and angiographic characteristics between groups of patients receiving CR and IR were compared using the Student's t-test or Wilcoxon rank-sum test when applicable for continuous variables and the chi-square test or Fisher's exact test for categorical variables, as appropriate. Survival curves were constructed using Kaplan-Meier estimates and compared with the log-rank test. We adjusted for differences in patient baseline characteristics by using weighted Cox proportional hazards regression models with inverse-probability-of-treatment weighting (IPTW) (15, 16). With the use of this method, weights for patients receiving IR were the inverse of (1-propensity score), and weights for patients receiving CR were the inverse of the propensity score. To stabilize IPTW, IPTW was multiplied by the marginal probability of the group (CR, IR). A full parsimonious model was developed that included treatment effect (CR or IR) and the aforementioned variables. Model discrimination was assessed with C statistics, and model calibration was assessed with Hosmer-Lemeshow statistics. Multivariate analysis using Cox regression proportional hazards model was performed to find predictive factors for all-cause death. All reported P values were 2 sided, and P values <0.05 were considered statistically significant. The Statistical Analysis Software package (SAS version 9.1, SAS Institute, Cary, NC, USA) and the R programing language version 2.15.2 were used for statistical analyses.
From the databases, 402 patients who had undergone PCI for reduced left ventricular systolic function, defined as a LVEF <50%, were identified. Of these patients, a total of 263 patients who met the selection criteria were enrolled. Among the patients, CR was achieved in 150 patients (57.0%). Baseline clinical and angiographic characteristics according to revascularization strategy are shown in Table 1. Patients in the IR group had a higher prevalence of MI history, three vessels disease, chronic total occlusion and high SYNTAX score than patients in the CR group.
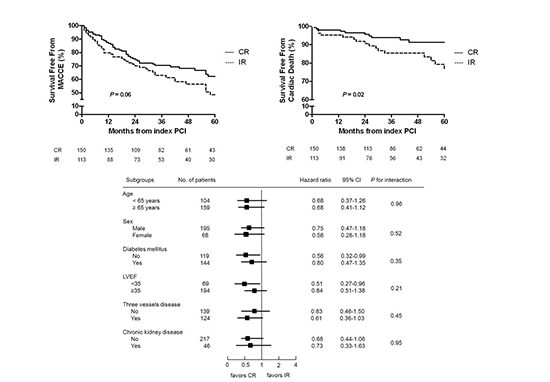
The median follow-up duration was 40 (interquartile range: 20-66) months in all participants. There was no difference of the median follow-up duration between the patients with CR and IR (40 [24-67] months and 35 [17-62] months, P=0.21). MACCE occurred in 52 (34.7%) patients in the CR group versus 51 (45.1%) patients in the IR group (P=0.06). All-cause death occurred in 60 patients (22.8%) during the follow up period. The cumulative clinical outcomes in patients with CR versus IR are listed in Table 2 and shown in Fig. 1. The incidence of all-cause death was significantly lower in patients with CR than in those with IR (17.3% vs. 30.1%, P=0.02). And cardiac death occurred less frequently in patients with CR than in patients with IR (7.3% vs. 17.7%, P=0.01). In the adjusted analysis with IPTW, patients with CR had lower cumulative rates of MACCE (adjusted hazard ratio [HR], 0.65; 95% confidence interval [CI], 0.44-0.95, P=0.028), all-cause death (adjusted HR, 0.48; 95% confidence interval [CI], 0.29-0.80; P=0.004) and cardiac death (adjusted HR, 0.40; 95% CI, 0.18-0.88; P=0.022) (Table 2). However, the cumulative rates of MI, any revascularization, and cerebrovascular accident were not different between two groups.
Among patients with IR, left anterior descending artery was remained as non-perfused vessel in 36 patients (31.9%). And, there was no difference of MACCE (42.9% vs. 50.0%, P=0.56), all-cause death (33.3% vs. 28.6%, P=0.59), and cardiac death (22.2% vs. 15.6%, P=0.40) according to non-perfused vessel (left anterior descending artery or not). Seventy one patients (62.8%) had chronic total occlusion and 64 patients (56.6%) had 3-vessel disease in IR group. And clinical outcomes were not different according to presence of chronic total occlusion and 3-vessel disease.
In multivariate analysis using a Cox regression proportional hazards model adjusting for age ≥65 yr, male sex, diabetes mellitus, chronic kidney disease, unstable angina, LVEF <35%, SYNTAX score and revascularization strategy, IR was an independent predictor for MACCE (adjusted HR, 1.53; 95% CI, 1.02-2.31; P=0.04). In addition to IR, MACCE was significantly associated with LVEF <35% (adjusted HR, 1.94; 95% CI, 1.31-2.87; P<0.01), and unstable angina (adjusted HR, 1.57; 95% CI, 1.05-2.37; P=0.03).
To determine whether the outcomes according to treatment strategy observed in the overall population were consistent, we calculated the unadjusted HR for MACCE in various subgroups (Fig. 2). Although the rate of MACCE for patients without diabetes mellitus and patients with LVEF <35% were significantly higher in the IR group, there were no significant interactions between the revascularization strategy and MACCE among the six subgroups.
We investigated the impact of CR on long-term clinical outcomes after PCI for patients with LVEF <50% in the DES era. The major findings of this study are as follows: 1) CR was associated with lower rates of MACCE all-cause death, and cardiac death with a median follow-up of 40 months. 2) A beneficial association of CR with MACCE was consistent, regardless of the various subgroups.
In real world practice, reasons to avoid interventional treatment in diseased vessels might include serious medical conditions such as severe left ventricular systolic dysfunction, cancer, old age and unsuitable anatomic conditions such as chronic total occlusion or severe vessel complexity (14). Uncertainty of the clinical impact of CR was another reason for deferring revascularization of non-culprit vessels, especially in the bare metal stent era (6, 7). Several studies have found that IR was associated with an increased short and long-term mortality in bare metal stent era (7, 8). However, in patients with left ventricular systolic dysfunction, long-term survival was not different between the CR and IR groups (8). The recent introduction of DES has dramatically reduced the restenosis rate resulting in improvement of long-term clinical outcomes (10, 14). However, limited data is available about the impact of CR on clinical outcomes, especially in patients with left ventricular systolic dysfunction, in the DES era.
In the DES era, large registry data demonstrated that IR was associated with higher mortality than CR at short-term and long-term follow up (14, 17). In the subgroup analysis for patients with LVEF <40%, the rate of mortality or MI in the IR group was not significantly higher than that in the CR group with a mean follow-up of 18.7 months (adjusted HR, 1.29; 95% CI, 0.88-1.89; P=0.20) (14). However, IR for patients with LVEF <40% was associated with significantly greater risk of death in a 5-yr follow up (adjusted HR, 1.31; 95% CI, 1.08-1.60; P=0.007) (17). In the present study, CR significantly reduced MACCE and all-cause death in patients with LVEF <50% with a median follow-up of 40 months. Similar with the results of previous studies, Kaplan-Meier curve for cardiac death showed that the difference of event-free survival between the CR and IR group, gradually increased over the longer follow-up period. Although it is uncertain why CR reduced cardiac death in patients with left ventricular systolic dysfunction, we suspect that improvement of LVEF and antiarrhythmic effect by reduction of ischemic burden after CR could possibly contribute to the decline of mortality in long-term follow up. Actually, in previous study with cardiac magnetic resonance imaging, Kirschbaum et al. (18) demonstrated that LVEF measured by cardiac magnetic resonance imaging improved after CR but did not change after IR in patients with MVD and dysfunctional myocardium. Included patients in their study had dysfunctional myocardium as our participants had left ventricular dysfunction. The increase in LVEF of 4% in CR group in this study was relatively small, but several clinical trials have shown that only 5% increase in LVEF had a significant improvement on prognosis (19). Although LVEF was improved after CR, the difference was not statistically significant between CR and IR group (6.45±11.29% vs. 3.98±11.47%, P=0.13) in this study.
In real world practice, IR groups could have a high incidence of non-cardiac death because physician might prefer to select a conservative revascularization strategy in patients with co-morbidities such as cancer, chronic obstructive pulmonary disease, and a short life expectancy regardless of lesion complexity. However, the association with better outcome of CR strategy was demonstrated in terms of cardiac mortality as well as all-cause mortality and there was no significant difference in respect to non-cardiac death between the CR and IR strategies in the present study. After IPTW with propensity score, the result was consistent. These findings suggest that CR strategy should be considered as a valuable option in the improved benefit of cardiac mortality for high risk subjects with left ventricular systolic dysfunction. A large number of patients with IR had chronic total occlusion or 3-vessel disease in this study and revascularization of chronic total occlusion and drug-eluting balloon for small vessel could increase CR rate and improve clinical outcomes (20, 21). Randomized prospective trial is warranted to demonstrate that CR strategy improve clinical outcomes.
This study had several limitations. The nonrandomized nature of the registry data could have resulted in selection bias. In particular, the decision to pursue CR was dependent on interventionist's opinion. Chronic total occlusion and complexity of coronary artery lesion seemed to be causes of IR and contributors to adverse outcomes (13, 21). Patients who underwent IR in our study had more chronic total occlusion and higher SYNTAX scores. Although we performed the IPTW to adjust for these potential confounding factors, we could not correct for all unmeasured variables. And, this study has low statistical power to conclude that CR reduces long-term mortality than IR. In addition, the majority of PCI in this registry was guided by quantitative coronary angiography, not by physiologic study like fractional flow reserve. And, viability of IR vessel was not analyzed because most patients did not performed viability test such as magnetic resonance imaging or dobutamine stress echocardiography. It was difficult to investigate the impact of functional CR on clinical outcomes. Finally, our results must be interpreted with caution, considering the relatively small size and single center experience. Therefore, large well designed prospective study is needed to establish the benefit of CR in patients with reduced LVEF.
In conclusion, the achievement of CR with DES could significantly improve long-term prognosis in patients with MVD and left ventricular systolic dysfunction compared with IR strategy. Accordingly, greater consideration should be given to achieve CR in patients with left ventricular systolic dysfunction. This study supports that left ventricular systolic dysfunction could not be a reason for deferring revascularization.
Figures and Tables
Fig. 1
Kaplan-Meier curves for outcome in patients with complete versus incomplete revascularization. Kaplan-Meier curves for (A) MACCE, and (B) cardiac death in patients with CR (solid line) versus IR (dashed line). CR, complete revascularization; IR, incomplete revascularization; MACCE, major adverse cardiac and cerebrovascular event; PCI, percutaneous coronary intervention.

Fig. 2
Comparative unadjusted HRs of treatment strategy for MACCE. CR, complete revascularization; IR, incomplete revascularization; LVEF, left ventricular ejection fraction; MACCE, major adverse cardiac and cerebrovascular event.

References
1. Bell MR, Gersh BJ, Schaff HV, Holmes DR Jr, Fisher LD, Alderman EL, Myers WO, Parsons LS, Reeder GS. Effect of completeness of revascularization on long-term outcome of patients with three-vessel disease undergoing coronary artery bypass surgery. A report from the Coronary Artery Surgery Study (CASS) Registry. Circulation. 1992; 86:446–457.
2. Scott R, Blackstone EH, McCarthy PM, Lytle BW, Loop FD, White JA, Cosgrove DM. Isolated bypass grafting of the left internal thoracic artery to the left anterior descending coronary artery: late consequences of incomplete revascularization. J Thorac Cardiovasc Surg. 2000; 120:173–184.
3. Bangalore S. Complete revascularization in contemporary practice. Circ Cardiovasc Interv. 2013; 6:5–7.
4. van den Brand MJ, Rensing BJ, Morel MA, Foley DP, de Valk V, Breeman A, Suryapranata H, Haalebos MM, Wijns W, Wellens F, et al. The effect of completeness of revascularization on event-free survival at one year in the ARTS trial. J Am Coll Cardiol. 2002; 39:559–564.
5. Ijsselmuiden AJ, Ezechiels J, Westendorp IC, Tijssen JG, Kiemeneij F, Slagboom T, van der Wieken R, Tangelder G, Serruys PW, Laarman G. Complete versus culprit vessel percutaneous coronary intervention in multivessel disease: a randomized comparison. Am Heart J. 2004; 148:467–474.
6. McLellan CS, Ghali WA, Labinaz M, Davis RB, Galbraith PD, Southern DA, Shrive FM, Knudtson ML. Association between completeness of percutaneous coronary revascularization and postprocedure outcomes. Am Heart J. 2005; 150:800–806.
7. Hannan EL, Racz M, Holmes DR, King SB 3rd, Walford G, Ambrose JA, Sharma S, Katz S, Clark LT, Jones RH. Impact of completeness of percutaneous coronary intervention revascularization on long-term outcomes in the stent era. Circulation. 2006; 113:2406–2412.
8. Wu C, Dyer AM, King SB 3rd, Walford G, Holmes DR Jr, Stamato NJ, Venditti FJ, Sharma SK, Fergus I, Jacobs AK, et al. Impact of incomplete revascularization on long-term mortality after coronary stenting. Circ Cardiovasc Interv. 2011; 4:413–421.
9. Lehmann R, Fichtlscherer S, Schächinger V, Held L, Hobler C, Baier G, Zeiher AM, Spyridopoulos I. Complete revascularization in patients undergoing multivessel PCI is an independent predictor of improved long-term survival. J Interv Cardiol. 2010; 23:256–263.
10. Kim YH, Park DW, Lee JY, Kim WJ, Yun SC, Ahn JM, Song HG, Oh JH, Park JS, Kang SJ, et al. Impact of angiographic complete revascularization after drug-eluting stent implantation or coronary artery bypass graft surgery for multivessel coronary artery disease. Circulation. 2011; 123:2373–2381.
11. Head SJ, Mack MJ, Holmes DR Jr, Mohr FW, Morice MC, Serruys PW, Kappetein AP. Incidence, predictors and outcomes of incomplete revascularization after percutaneous coronary intervention and coronary artery bypass grafting: a subgroup analysis of 3-year SYNTAX data. Eur J Cardiothorac Surg. 2012; 41:535–541.
12. Song YB, Lee SY, Hahn JY, Choi SH, Choi JH, Lee SH, Hong KP, Park JE, Gwon HC. Complete versus incomplete revascularization for treatment of multivessel coronary artery disease in the drug-eluting stent era. Heart Vessels. 2012; 27:433–442.
13. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009; 360:961–972.
14. Hannan EL, Wu C, Walford G, Holmes DR, Jones RH, Sharma S, King SB 3rd. Incomplete revascularization in the era of drug-eluting stents: impact on adverse outcomes. JACC Cardiovasc Interv. 2009; 2:17–25.
15. Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000; 11:550–560.
16. Heinze G, Jüni P. An overview of the objectives of and the approaches to propensity score analyses. Eur Heart J. 2011; 32:1704–1708.
17. Wu C, Dyer AM, Walford G, Holmes DR Jr, King SB 3rd, Stamato NJ, Sharma S, Jacobs AK, Venditti FJ, Hannan EL. Incomplete revascularization is associated with greater risk of long-term mortality after stenting in the era of first generation drug-eluting stents. Am J Cardiol. 2013; 112:775–781.
18. Kirschbaum SW, Springeling T, Boersma E, Moelker A, van der Giessen WJ, Serruys PW, de Feyter PJ, van Geuns RJ. Complete percutaneous revascularization for multivessel disease in patients with impaired left ventricular function: pre- and post-procedural evaluation by cardiac magnetic resonance imaging. JACC Cardiovasc Interv. 2010; 3:392–400.
19. Reffelmann T, Könemann S, Kloner RA. Promise of blood- and bone marrow-derived stem cell transplantation for functional cardiac repair: putting it in perspective with existing therapy. J Am Coll Cardiol. 2009; 53:305–308.
20. Latib A, Colombo A, Castriota F, Micari A, Cremonesi A, De Felice F, Marchese A, Tespili M, Presbitero P, Sgueglia GA, et al. A randomized multicenter study comparing a paclitaxel drug-eluting balloon with a paclitaxel-eluting stent in small coronary vessels: the BELLO (Balloon Elution and Late Loss Optimization) study. J Am Coll Cardiol. 2012; 60:2473–2480.
21. Valenti R, Migliorini A, Signorini U, Vergara R, Parodi G, Carrabba N, Cerisano G, Antoniucci D. Impact of complete revascularization with percutaneous coronary intervention on survival in patients with at least one chronic total occlusion. Eur Heart J. 2008; 29:2336–2342.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download