Abstract
Paraphilia is a psychiatric disease that has been difficult to cure. However, recently developed therapeutic methods hold promise. The patient was a 20-yr-old male with chief complaints of continuous masturbation, genital exposure, and aggressive behavior that started 2 yr ago. We administered leuprorelin 3.6 mg intramuscular injection per month, a depot gonadotrophin-releasing hormone analogue, to this patient who a severe mentally retardation with paraphilia. The clinical global impression (CGI)-severity, CGI-improvement and aberrant behavior checklist were performed. After one month, we observed significant improvement in symptoms, such as decreases of abnormal sexual behavior and sexual desire. The GnRH analogues are suggested to be used as an alternative or supplementary therapeutic method for sexual offenders after clinical studies.
In the late 19th century, Freud suggested that the cause of sexual perversion involves biological and developmental factors, as well as psychoanalytic factors (1). In recent years, researchers defined paraphilia as the addictive, impulsive, and compulsive expression of excessive sexual desire (2). The term 'sexual deviation' was first used in the Diagnostic and Statistical Manual of Mental Disorders (DSM)-I, and it was regarded as the subcategory of sociopathic personality disorder. The term 'paraphilia' was first used in the DSM-III. According to the criterion of DSM-IV-TR, paraphilia is described as "recurrent, intense sexually arousing fantasies, sexual urges, or behaviors generally involving 1) nonhuman objects, 2) the suffering or humiliation of oneself or one's partner, or 3) children or other nonconsenting persons that occur over a period of at least 6 months". These symptoms cause serious problems and damage in social, occupational, or other important functions. In the DSM-IV-TR, paraphilia is classified as gender identity disorder, and is divided into eight categories (exhibitionism, fetishism, frotteurism, pedophilia, transvestism, voyeurism, sexual sadism, and sexual masochism). The prevalence rate of paraphilia has been indirectly estimated through sexual crime reports. In France, 14% of the prisoners were reported to be sexual offenders (3). In 1998 in England, 11% of the prison population had an experience of sexual offence. In the United States, 17% of adolescent prisoners were reportedly sexual offenders.
There are various therapeutic methods for sexual offenders, such as psychoanalytic psychotherapy, cognitive behavior therapy (e.g., aversion therapy), surgical castration, and drug treatment for reducing sexual desire. However, the opinion that punishment on the offenders is needed for public safety could conflict with the opinion that the most clinically effective therapeutic method needs to be selected (4). Drugs used for the treatment of paraphilia include SSRI (selective serotonin reuptake inhibitors), cyproterone acetate, medroxyprogesterone, and GnRH (gonadoprophin releasing hormone) analogues. Among them, GnRH analogues are artificially synthesized agents of natural decapeptide GnRH, which is a hormone produced in the cell bodies of hypothalamic neurons and which is secreted directly into the hypophyseal portal system. GnRH analogues induce the downregulation of gonadotroph cells, the suppression of progesterone secretion, and the mild suppression of follicle-stimulating hormone (5). GnRH analogues are drugs mostly used as selective medicine for central precocious puberty. GnRH analogues stimulate and enhance the GnRH receptors of hypophysis in the initial stage, but later gradually suppress the receptors, consequently downregulating the GnRH receptors and desensitizing hypophyseal responses to GnRH (5, 6). Three representative commercial drugs of GnRH analogues are goserelin (3.75 mg and 11.25 mg), triptorelin (3.75 mg and 11.25 mg), which was recently approved in Europe for the treatment of male patients with severe sexual abnormality, and leuprorelin. Among them, leuprorelin (leuprolide acetate 3.75 mg and 11.25 mg), which is one of the luteinizing hormone releasing hormone (LHRH) analogue depot agents, has also been used as a selective treatment for central precocious puberty. Leuprorelin has clinical effects on obstetric and gynecologic diseases, such as endometriosis, and urologic diseases like prostate cancer as well as precocious puberty. Also, GnRH analogues have recently been reported to have clinical effects on paraphilia with abnormal sexual behavior (7, 8). Few studies have investigated the effects of GnRH agents on patients with paraphilia. This is because finding subjects with paraphilia is difficult due to reluctance to be identified or their refusal to have hormone therapy. On the other hand, long-acting GnRH depot agents are advantageous for children and adolescents who have poor compliance, or special patients who refuse drug administration. However, the disadvantage of the depot agents is that there are not enough study results regarding safety and effects, when compared to oral drugs (9, 10, 11, 12, 13).
Unlike normal developmental persons, mentally retarded persons with paraphilia are not able to express symptoms and difficulties by themselves. Thus, medical help is essential, and an individualized approach is necessary (11). While studies on the drug treatment of paraphilia have been conducted elsewhere, in Korea until recently only one case report by our research team with regard to the study for the clinical effect of GnRH depot agents on paraphilia was available (13).
We administered leuprorelin, a GnRH depot agent, to a severely mentally retarded patient with intractable paraphilia for 6 months, who had shown little symptom improvement despite continuous drug treatment, and later observed significant decreases of sexual desire and behavioral symptoms. This case report is the first such report in Korea. A review of the pertinent literature concerning mental retardation with paraphilia is also presented.
The patient was a 20-yr-old male who visited the outpatient clinic of Dankook University Hospital on 31 October 2012 with chief complaints of continuous masturbation, genital exposure, and aggressive behavior toward family members that started 2 yr ago. The patient was diagnosed with paraphilia (category: sexual exhibitionism and frotteurism) and severe mental retardation by a child psychiatrist based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Text Revision Edition (DSM-IV-TR) (2), and was hospitalized for 4 weeks to have psychotherapy and drug treatment (clomipramine 50 mg and paroxetine CR 37.5 mg). The patient was diagnosed with autistic disorder and severe mental retardation at the age of 5 at a child psychiatric clinic, and then attended a special school without undue problems. Self-injurious behaviors or aggressive attitudes were seldom observed, since the patient had a rather gentle personality. In the patient's elementary school and middle school years, self-injurious behavior began. At that time, fluoxetine 10-20 mg was administered for about a month at a neuropsychiatry clinic, which produced an improvement.
From August 2011, the patient spent much time alone at home as the patient's father had to nurse the patient's grandmother. For 2 months, the patient was locked up in home during the daytime. The patient's aunt, who lived nearby, visited and prepared a daily meal for the patient. The patient seldom masturbated before. However, as the patient spent more time alone, he gradually became obsessed with masturbation, and masturbated dozens of times a day. Sexual exposure with no sexual shame also increased gradually. At the same time, the patient showed increased aggression, such as suddenly hitting family members with hands or throwing objects. Based on the father's observation, pubic hair and muscles were noticeably developed in the patient's body shape. In February 2012, the patient displayed an aggressive attitude toward the aunt and father who were living together, in addition to masturbation symptoms. The father took the patient to a hospital, and the patient started to take valproate and olanzapine (5 mg). The symptoms were improved after about 3 months of treatment. The patient attended another hospital due to a matter of residence, where, considering side effects, olanzapine was changed to aripiprazole. Symptoms were significantly exacerbated. The patient again attended the outpatient clinic of the original hospital, and the aripiprazole was discontinued and olanzapine 7.5 mg begun. There was a weight gain of more than 10 kg, and the patient's weight exceeded 100 kg. The patient was hospitalized in a psychiatric hospital for 4 weeks with the chief complaints of continuous masturbation from morning until night, sexual exposure, excessive sexual desire, and aggressive behavior toward his father. Symptoms did not improve and the frequency of masturbation increased. Therefore, with a guardian's request, the patient visited the outpatient clinic of our hospital to have hormone therapy intended to reduce sexual desire.
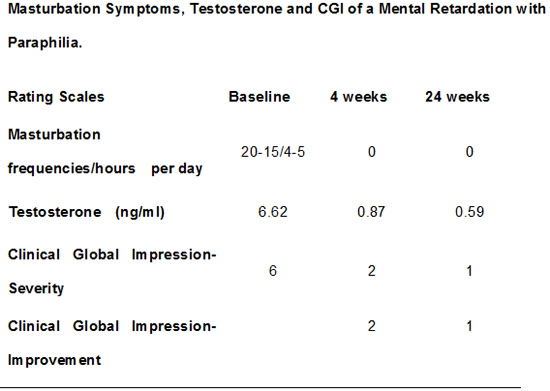
The patient again visited the outpatient clinic of our hospital. Despite continuous drug treatment and psychotherapy, paraphilic symptoms were not improved. If the patient's symptoms continue, there seemed to be a high possibility of being imprisoned as an offender. Therefore, the therapist considered hormone injection therapy, which is a more active therapeutic method. The therapist explained the studies on the injection of GnRH depot agents to the patient and guardian, and obtained prior consent. Also, the use of GnRH depot agents for paraphilia was approved by the patient's father. A basic physical examination for the patient was performed including medical history evaluation, blood test, and electrocardiogram. To compare the effects before and after the treatment, the clinical global impression-severity (CGI-S) (14), clinical global impression-improvement (CGI-I) and aberrant behavior checklist (ABC) (15) were performed. The ABC is a symptom checklist for assessing problem behaviors in individuals aged 6 to 54 with mental retardation. There are 58 items and five subscales. In addition, survey evaluation was conducted for the patient's parent regarding the pregnancy and early childhood of the patient, developmental history, and anamnesis. General psychological evaluation including an intelligence test was also conducted by a clinical psychologist. During hospitalization, the therapist administered leuprorelin depot 3.6 mg once. After discharge from the hospital, the same agent was administered once a month by subcutaneous injection. For the drug treatment, paroxetine 60 mg, valproate 1,000 mg, and olanzapine 5 mg were administered during this period. When the patient revisited after discharge from the hospital, the frequency of masturbation and sexual exposure was markedly decreased, and the aggressive attitude was also noticeably decreased. ABC, CGI-S, CGI-I were measured during hospitalization, 4 weeks after the drug administration, and 24 weeks after the drug administration, respectively. The masturbation frequencies and time decreased from 15-20/4-5 hr to 0/0 hr. The CGI-S score changed from 6 points to 2 points and 1 points with time and the CGI-I score showed 2 points after 4 weeks and 1 points after 24 weeks. The ABC scores did not show significant improvements. The testosterone level was 6.62 ng/mL during hospitalization, decreased to 0.87 ng/mL at 4 weeks, and decreased further to 0.59 at 6 months (Table 1). A weight gain occurred as the side effect of leuprorelin depot 3.6 mg administration. The patient's appearance became seemingly more gentle, and there was no other side effect complaint. As for the risk of osteoporosis, and no problems were found when examined by an orthopedist.
This is the first reported clinical use of Leuprolide for MR with paraphilia in Korea. The best treatment for paraphilia is to ememploy psychotherapy and drug treatment together (16). However, depending on the severity of disease, there may be cases in which an active therapeutic method should be applied from the initial stage. The World Federation of Societies of Biological Psychiatry has suggested various therapeutic approaches depending on the severity of paraphilia (16). In this case study, offences were continuously observed since the patient's paraphilic behavior was very severe, and there was a possibility of being imprisoned as an offender. Also, as education or persuasion was hard due to severe mental retardation, the guardian requested an active and fast treatment. Therefore, the therapist directly applied the guideline of level 5, which administers GnRH agonists, without going through levels 3 and 4, which administer cyproterone acetate or medroxyprogesterone following the levels that employ psychotherapy and antidepressant drug administration.
A previous case study (10, 11) reported that when triptorelin was administered to 6 patients with paraphilia for 7 yr, every abnormal sexual behavior disappeared in 5 patients. Recently, Rosler and Witztum (12) administered the GnRH agonist triptorelin 3.75 mg to 30 patients with paraphilia for 8-42 months along with supportive therapy. The average age of the subjects was 32; 25 subjects displayed pedophilia and 5 subjects were other unclassified patients with paraphilia. A notable improvement was observed in the abnormal sexual fantasy and desire scale score of the patients, where it decreased from an average of 48 points before the treatment to 5 points after the treatment. In our case study, 3 months after the administration of leuprorelin, which is a GnRH agonist, an improvement of 4 points was observed in the CGI scale, and an improvement of 12 points was observed in the SAST scale. This result is consistent with the aforementioned studies (10, 11, 12). GnRH depot agents are thought to suppress abnormal sexual behavior by directly acting on the central nervous system. In an animal experiment of male rats, the direct administration of GnRH into the cerebral spinal fluid was found to decrease aggression (17). GnRH depot agents are more effective in reducing testosterone within tissues than CPA or MPA agents (18). The continuous administration of GnRH depot agents can bring about a number of side effects. By continuously reducing the secretion of androgen, GnRH agents can cause hypogonadism, especially symptoms such as impotence in aged males, and could also decrease testicular volume and body hair (12). In addition, the administration of GnRH agents could reduce normal sexual desire as well as the desire of abnormal sexual behavior. The long-term administration of GnRH agents can lead to decreased bone density (12). Long-term administration of GnRH analogues can induce a number of side effects such as hepatotoxicity, hypertension, weight gain, and calcium loss. On the other hand, depressive disorder has been reported as a side effect of GnRH agonists. Nevertheless, GnRH analogues are recommended as one of the most effective therapeutic methods of paraphilia (16). Most side effects from hypogonadism are reversibly recovered when drug administration is stopped. In this case study, 10 kg/6 months weight gain and appetite increasing were observed due to the side effect of the drug, but there was no other particular side effect complaint. In the first 2-4 days after the administration of GnRH depot agents, special attention is required because sexual drive could increase (19). This is because GnRH analogues temporarily increase progesterone and follicle-stimulating hormone in the initial stage. Therefore, during this period, some clinicians recommend the administration of cyproterone acetate (12), which is a steroidal antiandrogen agent, and flutamide, which is a nonsteroidal antiandrogen agent. In this case study, the 'flare up' phenomenon reported in the previous studies, which occurs after the administration of GnRH depot agents, was observed for 2-7 days. However, it was alleviated without the additional administration of particular drugs. It was reported that SSRI reduces abnormal sexual behavior without decreasing normal sexual desire. In this case study, paroxetine 60 mg had been continuously administered, but a significant improvement in paraphilic symptoms was not observed when it was administered alone in the drug treatment. However, it seems to have been helpful for the improvement of the secondary depression and anxiety symptoms of the patient.
According to the guidelines of the United States, hormone injection therapy (e.g., cyproterone acetate, medroxyprogesterone, and GnRH analogues) is not a preferred treatment of paraphilia (16), mostly for ethical reasons. From an ethical view, hormone therapy should be applied only when patients meet all the conditions appropriate for the treatment, and the Committee for Medicinal Products for Human Use describes the conditions as follows (20). First, the patients have been diagnosed with paraphilia after careful psychiatric evaluation by a psychiatrist. Second, for hormone therapy, the clinical symptoms and behavior of the patients should be consistent with the clinical diagnosis, and the therapy should be appropriate for the patients' health status. Third, the therapy should not cause serious risk to the patients' health, or should not do harm to others. Fourth, the hormone therapy could be implemented only when other less invasive therapeutic method does not exist. Fifth, the patients have to agree to the hormone therapy.
In this case study, the improvement of paraphilic symptoms was observed after the administration of the GnRH analogue. However, the results cannot be generalized, since this is only one case report and, above all, the result was obtained in a short period of time. Therefore, it will be necessary to investigate the result of the clinical effect and side effect observed after a long period of treatment. Also, the therapeutic effect of GnRH analogues needs to be reexamined in a long-term study for a large-scale paraphilic patient group that is elaborately designed and accurately diagnosed and evaluated. Especially, the safety of GnRH analogue administration needs to be sufficiently investigated besides the clinical effect. If the clinical effect of GnRH analogues is sufficiently proved in the future studies despite a number of limitations on the clinical effect and safety, the GnRH analogues are expected to be used as an alternative or supplementary therapeutic method in addition to the diverse therapeutic methods currently used for the treatment of sexual offenders.
Figures and Tables
References
1. Garcia FD, Thibaut F. Current concepts in the pharmacotherapy of paraphilias. Drugs. 2011; 71:771–790.
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed. Washington, D.C.: American Psychiatric Association;2000.
3. Home Office. Home Office statistical bulletin: statistics of mentally disordered offenders in England and Wales. London: Home Office;1998-2001.
4. Ward T, Gannon TA, Birgden A. Human rights and the treatment of sex offenders. Sex Abuse. 2007; 19:195–216.
5. Conn PM, Crowley WF Jr. Gonadotropin-releasing hormone and its analogues. N Engl J Med. 1991; 324:93–103.
6. Wheeler MD, Styne DM. Drug treatment in precocious puberty. Drugs. 1991; 41:717–728.
7. Paterson WF, McNeill E, Reid S, Hollman AS, Donaldson MD. Efficacy of Zoladex LA (goserelin) in the treatment of girls with central precocious or early puberty. Arch Dis Child. 1998; 79:323–327.
8. Sifton DW. Physicians desk reference. Montvale: Medical Economics Company, Inc.;2001.
9. Isaac H, Patel L, Meyer S, Hall CM, Cusick C, Price DA, Clayton PE. Efficacy of a monthly compared to 3-monthly depot GnRH analogue (goserelin) in the treatment of children with central precocious puberty. Horm Res. 2007; 68:157–163.
10. Thibaut F, Cordier B, Kuhn JM. Effect of a long-lasting gonadotrophin hormone-releasing hormone agonist in six cases of severe male paraphilia. Acta Psychiatr Scand. 1993; 87:445–450.
11. Thibaut F, Cordier B, Kuhn JM. Gonadotrophin hormone releasing hormone agonist in cases of severe paraphilia: a lifetime treatment? Psychoneuroendocrinology. 1996; 21:411–419.
12. Rösler A, Witztum E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 1998; 338:416–422.
13. Kim HS, Park WS, Lee JW, Lim MH. A case of an adolescent with paraphilia with depot GnRH analogue (Goserelin). Korean J Psychopharmacol. 2011; 22:230–236.
14. Guy W. ECDU asessment manual for psychopharmacology, revised. Bethesda: US Department of Health, Education, and Welfare;1976.
15. Schroeder SR, Rojahn J, Reese RM. Brief report: reliability and validity of instruments for assessing psychotropic medication effects on self-injurious behavior in mental retardation. J Autism Dev Disord. 1997; 27:89–102.
16. Thibaut F, De La Barra F, Gordon H, Cosyns P, Bradford JM. WFSBP Task Force on Sexual Disorders. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of paraphilias. World J Biol Psychiatry. 2010; 11:604–655.
17. Kádár T, Telegdy G, Schally AV. Behavioral effects of centrally administered LH-RH agonist in rats. Physiol Behav. 1992; 51:601–605.
18. Barron JL, Millar RP, Searle D. Metabolic clearance and plasma half-disappearance time of D-TRP6 and exogenous luteinizing hormone-releasing hormone. J Clin Endocrinol Metab. 1982; 54:1169–1173.
19. Reilly DR, Delva NJ, Hudson RW. Protocols for the use of cyproterone, medroxyprogesterone, and leuprolide in the treatment of paraphilia. Can J Psychiatry. 2000; 45:559–563.
20. Recommendation Rec (2004) 10 of the Committee of Ministers to member states concerning the protection of the human rights and dignity of persons with mental disorder. Council of Europe. 2004.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download