Abstract
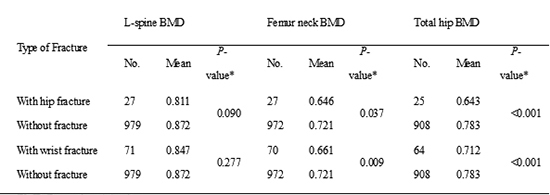
This study is to identify the characteristics of BMD and the related clinical consequences through a nationwide, consecutive, cross-sectional study. A total of 1,281 postmenopausal women was enrolled nationwide and underwent measurement for BMD using dual energy x-ray absorptiometry. Following the T-spine and L-spine plane radiography, they were evaluated for vertebral fracture by a semi-quantitative method using the Genant's method. Relationship between BMD and osteoporotic fracture and a degree of deformity in vertebral fracture, treatment history in osteoporosis and the EQ-5D was analyzed. The distribution of the normal, osteopenia and osteoporosis group was 25.9%, 37.0%, and 37.2% in lumbar spine, and 31.4%, 45.3%, and 23.3% in femur neck, respectively. BMD in subjects with symptomatic or asymptomatic vertebral fracture was significantly lower than those without fracture. The femur neck and total hip BMDs were significantly lower in hip fracture group (0.646 g/cm2 and 0.643 g/cm2, respectively) and wrist fracture group (0.661 g/cm2 and 0.712 g/cm2, respectively) than in subjects without fracture (0.721 g/cm2 and 0.712 g/cm2, respectively). The BMD was significantly lower with more severe degree of deformity in vertebral fracture and lower scores in mobility, usual activities and pain/discomfort of the EQ-5D. In Korean postmenopausal women, the prevalence of osteoporosis and vertebral, hip and wrist fracture increase and quality of life decreases with lower BMD.
As the proportion of postmenopausal women is increasing with the recent increase of aging population in Korea, it is anticipated that aging is proceeding more rapidly in the future. It is known that osteoporosis ultimately induces vertebral, hip or wrist fracture for which postmenopausal women are more vulnerable (1). Osteoporotic fracture is an important public health problem because it causes morbidity and mortality and generates not only a direct economic burden due to treatment cost for fracture but also the opportunity cost of patients and their family members. It is known that ethnicity and race are the important factors for the incidence of osteoporosis and differentiate the risk factors and treatment outcome of osteoporosis (2). Although it is known that a risk of osteoporosis and osteoporotic fracture is low in Korean population (3, 4), it is expected that the incidence of osteoporosis and osteoporotic fracture will rapidly increase when considering the speed of an increase in aging population. Because it is known generally that the mortality rate within 1 yr is approximately more or less than 20% when a hip fracture occurs (5, 6), most of the patients are receiving active treatment with surgery. In comparison, the treatment of osteoporotic vertebral fracture tends to be neglected relatively compared to hip fracture because osteoporotic fracture is very common in osteoporosis patients with many cases being asymptomatic and the short-term mortality rate is not high compared to that in hip fracture. However, it is known that vertebral fracture also increases a mortality rate (7) and increases a mortality rate as the number of fractures increases, and the mortality rate is higher in men (8, 9). For this reason, it is very important to prevent osteoporosis by active treatment through early diagnosis. Along with this, it is known that physical, psychological and social consequences from the result of osteoporotic fracture have a very important influence on the health-related quality of life (HRQOL). It is known that a decrease in BMD itself or asymptomatic fracture as well as symptomatic fracture also partly impacts on HRQOL.
BMD is the most general indicator to diagnose osteoporosis and determine for its treatment and the most important factor to predict osteoporotic fracture (10). It certainly has weakness that there may be measurement error due to two-dimensional imaging and it cannot reflect bone quality. Yet, it is the most widely used in a clinical setting because the criteria of osteoporosis and osteopenia defined by the WHO are based on BMD. BMD is also known to vary with age and sex and especially across different races. It is very important to understand BMD and the related clinical characteristics to utilize as the basic data for predicting overall public health burden related to osteoporosis. However, there has been no study reported regarding BMD and the related clinical aspects in Korean postmenopausal women.
Therefore, the purpose of this study is to evaluate BMD in Korean postmenopausal women based on Korean population with the national representative sample and to analyze the prevalence of osteoporosis and osteopenia, correlation between BMD and the condition of osteoporosis with the presence of symptoms and correlation between the EQ-5D and HRQOL.
This study was a nationwide, observational and cross-sectional study in Korean postmenopausal women who visited an orthopedic outpatient clinic of general hospitals and clinics from October 2010 through February 2011. The target sample size of 1,183 subjects was calculated by presuming 26% of the prevalence rate of osteoporotic vertebral compression fracture; the primary endpoint of this study, with 5% of precision and 95% of confidence interval, based on the report indicating that 18%-26% of postmenopausal white women had vertebral fracture according to the worldwide survey including Europe and the US (11). Considering a situation where it is impossible to conduct X-ray for diagnosis of vertebral fracture and collect the data, it was decided that a total of 1,479 subjects would be recruited in this study. In order to adjust the difference by region, regional distribution for women at 50 yr of age or older was confirmed by using the data in 2005 from the National Statistical Office of Korea, and the patients were to be recruited by allocating in an equal ratio by dividing into a total of four areas including the metropolitan, central, Youngnam and Honam regions.
Among the orthopedic outpatients, women at 50 yr of age or older with diagnosis of menopause confirmed by a physician were included. The menopause was defined as the last menstruation occurring 12 months before the enrollment.
Exclusion criteria included subjects whose menopause was not confirmed, women at 80 yr of age or older, subjects with high energy trauma (e.g., traffic accident and fall accident), subjects who experienced non-vertebral fracture within 6 months prior to the study enrollment (within the last 6 months). Subjects with poor cognitive ability to perform the study (to understand the contents of the survey questionnaire) at the discretion of the investigator, subjects whose normal reading was impossible were also excluded for two segments or more due to fracture or instrumentation between the first and the fourth lumbar vertebra or subjects whose BMD in the bilateral femur was non-evaluable due to femur fracture or instrumentation.
Based on a medical examination by interview, subjects were evaluated for age, height, weight, years since menopause, family history of osteoporosis in the maternal line (mother, brothers and sisters), family history of osteoporotic fracture (low energy fracture and asymptomatic fracture) in the maternal line (mother, brothers and sisters), living environment (residential area, the presence of living in facility residence, the presence of living with family, etc.), a type of insurance (medical insurance and medical care), smoking status and the amount of drinking. Concurrent diseases such as hypertension, diabetes mellitus, hypercholesterolemia, osteoporosis, rheumatoid arthritis, hyperthyroidism, hyperparathyroidism, severe osteoarthritis of knee joint, foot disease, spinal disease with claudication, and Parkinson's disease were confirmed, and untreated cataract was recorded.
In addition, history of trauma and fall-down within the last one year and the presence of back pain within the last one year were confirmed with the originated area, cause and treatment method in case of a fracture history.
BMD was measured in the lumbar spine, femur neck and total hip using dual energy x-ray absorptiometry (DXA). If the data measured within the last 3 months was available, it could be substituted for the data. The measurement for each area was performed based on the instruction by the manufacturer of a bone mineral densitometer.
Distributions of T-scores in lumbar spine, femur neck and total hip were evaluated when the T-scores were divided into normal group, osteopenia group, and osteoporosis group (T≥-1.0, -2.5<T<-1.0, and T≤-2.5). Also BMD, evaluated by age, and the correlation between BMI and BMD, was analyzed.
In order to identify the presence of vertebral fracture, standing anteroposterior and standing lateral radiographies were performed in the thoracic and lumbar spine. Vertebral fracture was assessed based on the degree of deformity by the semi-quantitative approach for each vertebra (L-spine 1-5, T-spine 1-12) (12) confirmed by an orthopedic specialist, and the presence of the symptom was confirmed. Fractured vertebrae were graded as normal (grade 0), mildly deformed (grade 1, 20%-25% height reduction), moderately deformed (grade 2, 25%-40% height reduction), and severely deformed (grade 3, over 40% height reduction) by Genant semiquantitative approach (12).
The percentages of vertebral compression fracture were compared in the normal, osteopenia and osteoporosis group, (T≥-1.0, -2.5<T<-1.0, and T≤-2.5). The mean BMDs in the L-spine, femur neck and total hip were compared between subjects with and without osteoporotic vertebral fracture. BMD was also compared among vertebral fracture patients with pain, asymptomatic patients with vertebral fracture and those without vertebral fracture.
The correlation between the presence of hip and wrist fracture and BMD of each site was analyzed.
The functional assessment was completed by using the EQ-5D. EQ-5D is a standardized instrument for use as a measure of health outcome. EQ-5D is applicable to a wide range of health conditions and treatments and provides a simple descriptive profile and single index value for health status. The result responded to each question of the EQ-5D was presented by calculating the utility index of each patient using the model indicated in the reference of "South Korean Time Trade-Off Values for EQ-5D Health States: Modeling with Observed Values for 101 Health States" by Lee et al. (13) The correlation between each item of the EQ-5D and BMD was analyzed, and the scale (0 means the worst health and 100 means the best health patient can imagine) to indicate the status of patient's health was measured by the visual analogue scale (VAS), followed by the analysis of correlation with the EQ-5D.
In the descriptive analysis of baseline characteristics, the numerical data are expressed as mean±standard deviations. Statistical analysis was performed using one-way analysis of variance, t-test, Cochran-Armitage trend test and chi-square test, if applicable. A probability value of less than 0.05 was accepted as the level of statistical significance.
In this study, a total of 1,281 subjects participated from 62 institutions. Among them, 1,255 subjects were evaluated excluding 25 subjects who did not meet the inclusion and exclusion criteria and one subject whose fracture was not assessed. The mean age was 63.2 (±7.7) yr, with the distribution of 36.4%, 39.5%, and 24.1% in the 50s, 60s and 70s, respectively. The mean height was 155.3 (±5.3) cm and the mean weight 57.4 (±8.3) kg with the mean BMI at 23.8 (±3.2) kg/m2. The mean age at the time of menopause was 48.8 (±5.2) yr, and the mean duration of postmenopause was 14.5 (±9.0) yr.
The dual energy x-ray absorptiometry used in this study were Lunar (GE Healthcare, USA, 666 patients), Discovery (Hologic Inc., USA, 246 patients), Dexxum (Osteosys, Korea, 293 patients), and Norland (CooperSurgical, USA, 50 patients).
The mean BMD with mean T-score was 0.86 g/cm2 with -1.91, 0.71 g/cm2 with -1.62 and 0.77 g/cm2 with -1.29 in lumbar spine, femur neck and total hip, respectively. As a result of assessing T-scores by dividing them into the normal, osteopenia and osteoporosis group (T≥-1.0, -2.5<T<-1.0, and T≤-2.5), the distribution of 25.9%, 37.0%, and 37.2% was seen in lumbar spine, respectively, the distribution of 31.4%, 45.3%, and 23.3% in femur neck, respectively, and the distribution of 40.7%, 42.5%, and 16.9% in total hip, respectively.
Regarding BMD with age, BMD and T-scores in lumbar spine, femur neck and total hip tended to decrease with increasing age (Fig. 1) (Table 1).
BMI indicated a positive correlation with the L-spine BMD (r=0.303, P<0.001) and week correlations with the femur neck (r=0.172, P<0.001) and total hip BMD (r=0.229, P<0.001).
As a result of evaluating vertebral compression fracture by dividing the T-scores into the normal group, osteopenia group and osteoporosis group (T≥-1.0, -2.5<T<-1.0, and T≤-2.5), the incidence of vertebral compression fracture tended to decrease with increasing T-score (Fig. 2). In addition, it was statistically significant that the mean BMD values in the L-spine, femur neck and total hip were lower in subjects with osteoporotic vertebral fracture than those without fracture, (P<0.001 for all three), regardless of the presence of back pain (Fig. 3). The mean T-scores in the L-spine, femur neck and total hip were lower in subjects with osteoporotic vertebral fracture than those without fracture, (P<0.001 for all three), regardless of the presence of pain (Fig. 3).
The L-spine and total hip BMD values were significantly lower in vertebral fracture patients with pain than in asymptomatic fracture patients (P<0.01 for all), and BMD values in the L-spine, femur and total hip were significantly lower in asymptomatic fracture patients than those without vertebral fracture (P<0.01 for all) (Fig. 4).
As a result of analyzing the correlation between the degree of deformity from vertebral fracture and BMD, the L-spine, femur neck and total hip BMD in the normal group was significantly higher than those in the Genant SQ Grade 1 and the Genant SQ Grade 2 and 3 group (P<0.01). And, the femur neck and total hip BMD in the Genant SQ Grade I group was significantly higher than those in the Genant SQ Grade 2 and 3 (P<0.01); however, there was no significant difference in the L-spine BMD between the Genant SQ Grade 1 group and the Genant SQ Grade 2 and 3 group (Fig. 5).
The L-spine BMD in the groups with hip fracture and wrist fracture was lower than that in the group without fracture, showing no statistically significant difference, but the femur neck and total hip BMD was significantly lower in the patients with hip fracture and wrist fracture than in those without fracture (P=0.037 and P<0.001 for hip fracture and P=0.009 and P<0.001 for wrist fracture, respectively) (Table 2).
BMD values for each question of the EQ-5D are indicated in Table 3. Visual analogue scale (VAS) values for all items were significantly higher in the Level 1 group compared to those in the Level 2 and 3 groups, showing a strong positive correlation between VAS and the EQ-5D (Fig. 6).
In terms of mobility, the femur neck and total hip BMD values were significantly higher in the Level 1 group than in the other groups (P=0.037 and 0.011, respectively). For the items of usual activities and pain/discomfort, the total hip BMD was significantly higher in the Level 1 group than in the other groups (P=0.028 and 0.018, respectively). For the item of anxiety/depression, the femur neck BMD was significantly higher in the Level 1 than in the other groups (P=0.020) (Table 3).
BMD levels in the L-spine, femur and hip did not have correlations with VAS.
This study is the first nationwide, observational and cross-sectional study conducted in Korea in order to evaluate BMD and the related clinical aspects in postmenopausal women. The study has the strength of reducing a bias from the region by recruiting patients divided into the four areas in the equal ratio based on the regional distribution of women at 50 yr of age or older and identifying nationwide characteristics of Korean menopausal women by recruiting 1,281 patients from 62 centers for the same period consecutively. However, it has a weakness of not reflecting all characteristics of general population properly because this study targeted patients who visited an orthopedic clinic. Another weakness of our study is that we used four different DXA in measurement of bone mineral density, which has different references to produce different T-scores between the models.
In this study, the values of BMD in the 50s, 60s, and 70s significantly diminished with increasing age, and the result was similar to the other study where the BMD significantly diminished with increasing age in postmenopausal women (1).
It is known that body fat and lean mass are correlated with BMD and postmenopausal, and some studies have indicated that obesity has a protective effect on bone loss to a certain extent (14, 15), but there are reports that obesity, especially fat mass, interrupts bone health (16, 17). Therefore, there may be different opinions regarding the correlation between BMI and BMD, but there are many reports where body weight has a protective effect on BMD and the percentage of body fat is negatively related to BMD (18). In our study, although it is a weakness not to differentiate for fat mass separately, BMI has shown a positive correlation with the L-spine BMD and very week correlations with the femur neck and total femur BMD, which is similar to the results in other studies.
It is known that osteoporotic vertebral fracture not only induces a severe symptom but also appear asymptomatic in many cases. In this study, BMD in subjects with symptomatic vertebral fracture was significantly lower than that in asymptomatic patients, and BMD in subjects with asymptomatic vertebral fracture was significantly lower than in those without fracture. Consequently, it seems that the incidences of both vertebral compression fracture and symptomatic vertebral compression fracture increase with decreasing BMD.
BMD usually has a correlation with vertebral compression fracture, and it is possible to form a hypothesis where higher BMD may have lower asymptomatic fracture followed by lower symptomatic fracture, inferring from the result of this study. It is associated with what BMD has a significant correlation with mortality (19) as well as fracture, and it can be interpreted that BMD reduction not only induces asymptomatic and symptomatic vertebral fractures but also increases mortality since asymptomatic vertebral fracture also increases mortality.
In addition, our result shows that a decreasing BMD causes an increasing degree of collapse in vertebral compression fracture; it is thought that the lower the BMD value is, the easier the deformity occurs by compressive force because the compressive force becomes to affect persistently on thoracic or thoracolumbar vertebra due to kyphosis of the thoracic spine and trunk weight although the same external pressure affects with vertebral fracture.
In this study, BMD in the groups with hip fracture and wrist fracture was lower than in the group without fracture, and especially the difference was significant in the femur neck and total hip BMD but not in the lumbar BMD. This result can be interpreted in two ways. One is that the lumbar BMD is less accurate than the hip BMD because the lumbar BMD might be measured higher than the actual BMD due to degenerative change or vascular calcification (20), and it is known that the total hip BMD is generally the best predictor of clinical fracture (21). The other is that it can be interpreted the femur neck or total hip BMD acts as a fracture risk more directly than the lumbar spine BMD in hip fracture.
One of the risk factors for development of osteoporosis is reduced physical activity (22). It is known that physical performances such as gait speed, step length and grip strength are better with increasing BMD (23). Physical performance has a positive correlation with general health and pain, leading to the correlation with quality of life. As an index of assessing quality of life, the EQ-5D is a useful tool. In this study, the EQ-5D scores significantly dropped in the dimensions of usual activities, mobility, pain/discomfort and anxiety/depression with decreasing BMD, and the differences were significant in the femur neck and total BMD, suggesting the close relationship between BMD and quality of life. It is known that quality of life (24) and mortality (25, 26) can be improved by increasing BMD with the treatment for osteoporosis. In addition, lower BMD is closely associated with the decreased sleep duration related to severe endocrine and metabolic dysfunction (27). In old women, lower BMD also shows positive correlations with the higher Beck Depression Inventory Score and higher levels of depressive symptoms with higher prevalence of depression (28). In women, it is known that the femur neck and total hip BMDs show positive correlations with the respiratory function represented by the FEV1 (29). In older women, lower BMD is correlated with depression of left ventricular function (30) and coronary heart disease (31, 32).
Moreover, BMD is associated with an increased mortality risk (19, 33). A Japanese study where the result is expected to be similar to that in Korean population has also reported that low BMD is significantly associated with an increased risk of mortality even with excluding the previous lifestyle-related diseases such as stroke, hypertension, heart disease and smoking (1).
Despite several limitations in this study, the nationwide cross-sectional study indicated that the prevalence of osteoporosis increased with increasing age in Korean postmenopausal women and BMD had a significant correlation with osteoporotic fracture. In addition, the BMD level was significantly low in subjects with the history of asymptomatic vertebral fracture as well as in those with symptomatic vertebral fracture, and the femur neck and total hip BMD values were significantly lower with the higher degree of vertebral fracture collapse and the history of hip fracture and wrist fracture. The femur neck and total hip BMDs were correlated with quality of life measured by the EQ-5D. Based on the result of this study, BMD and its clinical consequences were confirmed in Korean postmenopausal women, and it is expected that the result will help us establish the treatment strategy in the future.
In Korean postmenopausal women, the prevalence of osteoporosis and vertebral, hip and wrist fracture increase and quality of life decreases with lower BMD. Therefore, it is determined that active treatment is necessary for improving the clinical outcome of osteoporosis patients.
Figures and Tables
Fig. 1
T-scores by age group: Box plot. (A) T-score of L-spine. (B) T-score of femur neck. (C) T-score of total hip. With increasing age, the L-spine, femur neck and total hip BMD values significantly decrease.

Fig. 2
The incidence of osteoporotic vertebral compression fracture by T-score. With decreasing T-score, the prevalence of vertebral compression fracture increase.

Fig. 3
Bone mineral density and fracture. (A) The mean BMD values in the L-spine, femur neck and total hip was significantly lower in subjects with osteoporotic vertebral fracture than those without fracture (P < 0.001 for all three). (B) T-scores in the L-spine, femur neck and total hip was also significantly lower in subjects with osteoporotic vertebral fracture than those without fracture (P < 0.001 for all three).

Fig. 4
Bone mineral density and osteoporotic vertebral compression fracture with or without pain. The L-spine and total hip BMD values was significantly lower in vertebral fracture patients with pain than in asymptomatic fracture patients (P < 0.01 for all), and BMD values in the L-spine, femur neck and total hip was significantly lower in asymptomatic fracture patients than those without vertebral fracture (P < 0.01 for all) by analysis of variance.

Fig. 5
Bone mineral density by vertebral deformity grade. The L-spine, femur neck and total hip BMD are significantly higher in the normal group than that in the Genant SQ Grade 1 and the Genant SQ Grade 2 and 3 group (P < 0.01). The femur neck and total hip BMD are significantly higher in Genant SQ Grade 1 than the Genant SQ Grade 2 and 3 (P < 0.01) by analysis of variance (ANOVA).

Fig. 6
Correlation between the EQ-5D index and VAS. The EQ-5D index shows a weak correlation coefficient of r = 0.445 with VAS (P < 0.001).

ACKNOWLEDGMENT
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. We deeply appreciate 62 centers which participated in our TOP study.
References
1. Suzuki T, Yoshida H. Low bone mineral density at femoral neck is a predictor of increased mortality in elderly Japanese women. Osteoporos Int. 2010; 21:71–79.
2. Cauley JA. Defining ethnic and racial differences in osteoporosis and fragility fractures. Clin Orthop Relat Res. 2011; 469:1891–1899.
3. Kanis JA, Burlet N, Cooper C, Delmas PD, Reginster JY, Borgstrom F, Rizzoli R. European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2008; 19:399–428.
4. Kanis JA, Johnell O, De Laet C, Jonsson B, Oden A, Ogelsby AK. International variations in hip fracture probabilities: implications for risk assessment. J Bone Miner Res. 2002; 17:1237–1244.
5. Yoon HK, Park C, Jang S, Jang S, Lee YK, Ha YC. Incidence and mortality following hip fracture in Korea. J Korean Med Sci. 2011; 26:1087–1092.
6. Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ. Mortality following hip fracture: trends and geographical variations over the last 40 years. Injury. 2008; 39:1157–1163.
7. Lau E, Ong K, Kurtz S, Schmier J, Edidin A. Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am. 2008; 90:1479–1486.
8. Puisto V, Rissanen H, Heliövaara M, Impivaara O, Jalanko T, Kröger H, Knekt P, Aromaa A, Helenius I. Vertebral fracture and cause-specific mortality: a prospective population study of 3,210 men and 3,730 women with 30 years of follow-up. Eur Spine J. 2011; 20:2181–2186.
9. Lee YK, Jang S, Jang S, Lee HJ, Park C, Ha YC, Kim DY. Mortality after vertebral fracture in Korea: analysis of the National Claim Registry. Osteoporos Int. 2012; 23:1859–1865.
10. Fujiwara S, Kasagi F, Masunari N, Naito K, Suzuki G, Fukunaga M. Fracture prediction from bone mineral density in Japanese men and women. J Bone Miner Res. 2003; 18:1547–1553.
11. Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J. 2006; 6:479–487.
12. Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993; 8:1137–1148.
13. Lee YK, Nam HS, Chuang LH, Kim KY, Yang HK, Kwon IS, Kind P, Kweon SS, Kim YT. South Korean time trade-off values for EQ-5D health states: modeling with observed values for 101 health states. Value Health. 2009; 12:1187–1193.
14. Albala C, Yáñez M, Devoto E, Sostin C, Zeballos L, Santos JL. Obesity as a protective factor for postmenopausal osteoporosis. Int J Obes Relat Metab Disord. 1996; 20:1027–1032.
15. Reid IR, Plank LD, Evans MC. Fat mass is an important determinant of whole body bone density in premenopausal women but not in men. J Clin Endocrinol Metab. 1992; 75:779–782.
16. Zhao LJ, Jiang H, Papasian CJ, Maulik D, Drees B, Hamilton J, Deng HW. Correlation of obesity and osteoporosis: effect of fat mass on the determination of osteoporosis. J Bone Miner Res. 2008; 23:17–29.
17. Greco EA, Fornari R, Rossi F, Santiemma V, Prossomariti G, Annoscia C, Aversa A, Brama M, Marini M, Donini LM, et al. Is obesity protective for osteoporosis? Evaluation of bone mineral density in individuals with high body mass index. Int J Clin Pract. 2010; 64:817–820.
18. Kim KC, Shin DH, Lee SY, Im JA, Lee DC. Relation between obesity and bone mineral density and vertebral fractures in Korean postmenopausal women. Yonsei Med J. 2010; 51:857–863.
19. Mussolino ME, Madans JH, Gillum RF. Bone mineral density and mortality in women and men: the NHANES I epidemiologic follow-up study. Ann Epidemiol. 2003; 13:692–697.
20. Yu W, Glüer CC, Fuerst T, Grampp S, Li J, Lu Y, Genant HK. Influence of degenerative joint disease on spinal bone mineral measurements in postmenopausal women. Calcif Tissue Int. 1995; 57:169–174.
21. Black DM, Cummings SR, Stone K, Hudes E, Palermo L, Steiger P. A new approach to defining normal vertebral dimensions. J Bone Miner Res. 1991; 6:883–892.
22. Kanis JA. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report: WHO Study Group. Osteoporos Int. 1994; 4:368–381.
23. Lindsey C, Brownbill RA, Bohannon RA, Ilich JZ. Association of physical performance measures with bone mineral density in postmenopausal women. Arch Phys Med Rehabil. 2005; 86:1102–1107.
24. Yoh K, Tanaka K, Ishikawa A, Ishibashi T, Uchino Y, Sato Y, Tobinaga M, Hasegawa N, Kamae S, Yoshizawa M. Health-related quality of life (HRQOL) in Japanese osteoporotic patients and its improvement by elcatonin treatment. J Bone Miner Metab. 2005; 23:167–173.
25. Sim IW, Ebeling PR. Treatment of osteoporosis in men with bisphosphonates: rationale and latest evidence. Ther Adv Musculoskelet Dis. 2013; 5:259–267.
26. Lee JH, Lee YH, Moon SH, Lee YS. Prevalence of Osteoporotic Vertebral Compression Fractures in Korean Post Menopausal Women Study Group. Influence of insurance benefit criteria on the administration rate of osteoporosis drugs in postmenopausal females. Clin Orthop Surg. 2014; 6:56–61.
27. Fu X, Zhao X, Lu H, Jiang F, Ma X, Zhu S. Association between sleep duration and bone mineral density in Chinese women. Bone. 2011; 49:1062–1066.
28. Coelho R, Silva C, Maia A, Prata J, Barros H. Bone mineral density and depression: a community study in women. J Psychosom Res. 1999; 46:29–35.
29. Lekamwasam S, Trivedi DP, Khaw KT. An association between respiratory function and bone mineral density in women from the general community: a cross sectional study. Osteoporos Int. 2002; 13:710–715.
30. Laudisio A, Marzetti E, Antonica L, Cocchi A, Bernabei R, Zuccalà G. Association of left ventricular function with bone mineral density in older women: a population-based study. Calcif Tissue Int. 2008; 82:27–33.
31. Tankó LB, Christiansen C, Cox DA, Geiger MJ, McNabb MA, Cummings SR. Relationship between osteoporosis and cardiovascular disease in postmenopausal women. J Bone Miner Res. 2005; 20:1912–1920.
32. Van Der Klift M, Pols HA, Geleijnse JM, Van Der Kuip DA, Hofman A, De Laet CE. Bone mineral density and mortality in elderly men and women: the Rotterdam Study. Bone. 2002; 30:643–648.
33. Browner WS, Seeley DG, Vogt TM, Cummings SR. Non-trauma mortality in elderly women with low bone mineral density: Study of Osteoporotic Fractures Research Group. Lancet. 1991; 338:355–358.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download