1. Bruno MK, Raizer J. Leptomeningeal metastases from solid tumors (Meningeal carcinomatosis). Cancer Treat Res. 2005; 125:31–52.
2. Glass JP, Melamed M, Chernik NL, Posner JB. Malignant cells in cerebrospinal fluid (CSF): the meaning of a positive CSF cytology. Neurology. 1979; 29:1369–1375.
3. Chamberlain MC. Neoplastic meningitis. Oncologist. 2008; 13:967–977.
4. Park JO, Shin HJ, Kim HJ, Lee SW, Jeung HC, Kim SM, Yoo NC, Chung HC, Kim JH, Kim BS, et al. Leptomeningeal carcinomatosis in solid tumors; clinical manifestation and treatment. J Korean Cancer Assoc. 2001; 33:34–40.
5. Jaeckle KA. Neoplastic meningitis from systemic malignancies: diagnosis, prognosis and treatment. Semin Oncol. 2006; 33:312–323.
6. Herrlinger U, Weller M, Schabet M. New aspects of immunotherapy of leptomeningeal metastasis. J Neurooncol. 1998; 38:233–239.
7. Chamberlain MC. Leptomeningeal metastasis. Semin Neurol. 2010; 30:236–244.
8. Groves MD. New strategies in the management of leptomeningeal metastases. Arch Neurol. 2010; 67:305–312.
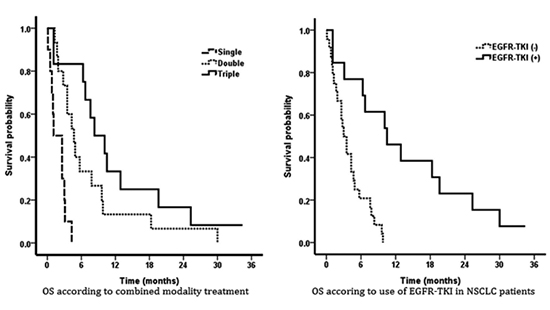
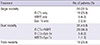
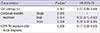
10. Park JH, Kim YJ, Lee JO, Lee KW, Kim JH, Bang SM, Chung JH, Kim JS, Lee JS. Clinical outcomes of leptomeningeal metastasis in patients with non-small cell lung cancer in the modern chemotherapy era. Lung Cancer. 2012; 76:387–392.
11. Chamberlain MC. Leptomeningeal metastasis. Curr Opin Neurol. 2009; 22:665–674.
12. Chamberlain MC. Leptomeningeal metastases: a review of evaluation and treatment. J Neurooncol. 1998; 37:271–284.
13. Rudnicka H, Niwińska A, Murawska M. Breast cancer leptomeningeal metastasis--the role of multimodality treatment. J Neurooncol. 2007; 84:57–62.
14. Hildebrand J. Prophylaxis and treatment of leptomeningeal carcinomatosis in solid tumors of adulthood. J Neurooncol. 1998; 38:193–198.
15. Boogerd W, Hart AA, van der Sande JJ, Engelsman E. Meningeal carcinomatosis in breast cancer. Prognostic factors and influence of treatment. Cancer. 1991; 67:1685–1695.
16. Gauthier H, Guilhaume MN, Bidard FC, Pierga JY, Girre V, Cottu PH, Laurence V, Livartowski A, Mignot L, Diéras V. Survival of breast cancer patients with meningeal carcinomatosis. Ann Oncol. 2010; 21:2183–2187.
17. Lee JL, Kang YK, Kim TW, Chang HM, Lee GW, Ryu MH, Kim E, Oh SJ, Lee JH, Kim SB, et al. Leptomeningeal carcinomatosis in gastric cancer. J Neurooncol. 2004; 66:167–174.
18. Balm M, Hammack J. Leptomeningeal carcinomatosis: presenting features and prognostic factors. Arch Neurol. 1996; 53:626–632.
19. Bruna J, González L, Miró J, Velasco R, Gil M, Tortosa A. Neuro-Oncology Unit of the Institute of Biomedical Investigation of Bellvitge. Leptomeningeal carcinomatosis: prognostic implications of clinical and cerebrospinal fluid features. Cancer. 2009; 115:381–389.
20. Harstad L, Hess KR, Groves MD. Prognostic factors and outcomes in patients with leptomeningeal melanomatosis. Neuro Oncol. 2008; 10:1010–1018.
21. Murray JJ, Greco FA, Wolff SN, Hainsworth JD. Neoplastic meningitis. Marked variations of cerebrospinal fluid composition in the absence of extradural block. Am J Med. 1983; 75:289–294.
22. Wasserstrom WR, Glass JP, Posner JB. Diagnosis and treatment of leptomeningeal metastases from solid tumors: experience with 90 patients. Cancer. 1982; 49:759–772.
23. Glantz MJ, Jaeckle KA, Chamberlain MC, Phuphanich S, Recht L, Swinnen LJ, Maria B, LaFollette S, Schumann GB, Cole BF, et al. A randomized controlled trial comparing intrathecal sustained-release cytarabine (DepoCyt) to intrathecal methotrexate in patients with neoplastic meningitis from solid tumors. Clin Cancer Res. 1999; 5:3394–3402.
24. Bokstein F, Lossos A, Siegal T. Leptomeningeal metastases from solid tumors: a comparison of two prospective series treated with and without intra-cerebrospinal fluid chemotherapy. Cancer. 1998; 82:1756–1763.
25. Glantz MJ, Cole BF, Recht L, Akerley W, Mills P, Saris S, Hochberg F, Calabresi P, Egorin MJ. High-dose intravenous methotrexate for patients with nonleukemic leptomeningeal cancer: is intrathecal chemotherapy necessary? J Clin Oncol. 1998; 16:1561–1567.
26. Yi HG, Kim HJ, Kim YJ, Han SW, Oh DY, Lee SH, Kim DW, Im SA, Kim TY, Kim CS, et al. Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) are effective for leptomeningeal metastasis from non-small cell lung cancer patients with sensitive EGFR mutation or other predictive factors of good response for EGFR TKI. Lung Cancer. 2009; 65:80–84.
27. Lee E, Keam B, Kim DW, Kim TM, Lee SH, Chung DH, Heo DS. Erlotinib versus gefitinib for control of leptomeningeal carcinomatosis in non-small-cell lung cancer. J Thorac Oncol. 2013; 8:1069–1074.
28. Morris PG, Reiner AS, Szenberg OR, Clarke JL, Panageas KS, Perez HR, Kris MG, Chan TA, DeAngelis LM, Omuro AM. Leptomeningeal metastasis from non-small cell lung cancer: survival and the impact of whole brain radiotherapy. J Thorac Oncol. 2012; 7:382–385.
29. Kim HJ, Im SA, Keam B, Kim YJ, Han SW, Kim TM, Oh DY, Kim JH, Lee SH, Chie EK, et al. Clinical outcome of central nervous system metastases from breast cancer: differences in survival depending on systemic treatment. J Neurooncol. 2012; 106:303–313.






 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download