Abstract
This study was designed to evaluate whether sirolimus (SRL) conversion effectively improves renal function and histopathology in calcineurin inhibitor (CNI)-treated renal recipients with mild to moderate renal insufficiency. SRL conversion from CNI was performed in patients who underwent kidney transplantation from 6 months to 5 yr prior to screening. Forty-five patients were enrolled. The effect of SRL conversion on graft function was evaluated, and protocol biopsies were performed preconversion and 1 yr after conversion. Overall graft function after SRL conversion gradually improved, and the improvement in renal function was closely associated with the shorter duration of CNI exposure. When we divided the patients by the duration of CNI exposure, the patients with less than 1 yr of CNI exposure demonstrated significant improvement, but patients with a greater than 1 yr CNI exposure did not exhibit significant improvement. In contrast, protocol biopsies demonstrated no significant improvements in the modified "ah" score or other Banff scores after SRL conversion. Furthermore, the duration of CNI treatment prior to SRL conversion was not associated with histological findings 1 yr after SRL conversion. SRL conversion improved graft function in renal recipients with mild to moderate renal insufficiency, but this effect is not accompanied by histological improvement.
Calcineurin inhibitors (CNI) are widely used immunosuppressants that greatly decrease the incidence of acute rejection and improve both graft and patient survival rates in kidney transplantation patients. However, the long-term use of CNI produces chronic allograft dysfunction due to nephrotoxicity (1, 2). Progressive chronic nephrotoxicity is a major long-term toxic effect of CNI, and it is associated with mild-to-moderate renal dysfunction (1, 2, 3).
Sirolimus (SRL) is an effective immunosuppressive agent that improves long-term graft function and survival without nephrotoxicity (4, 5). SRL has been used for primary immunosuppression without CNI, early withdrawal or the minimization of CNI, and early or late conversion from CNI (4, 6, 7, 8, 9, 10). Some clinicians advocate the early use of SRL and CNI withdrawal because SRL has many beneficial effects, such as the reduction of malignancy risk after renal transplantation and improved long-term outcomes and associated cardiovascular risk profiles (11, 12, 13). However, the early use of SRL may increase the incidence of postoperative issues, such as impaired wound healing or lymphocele, and it may extend the duration of delayed graft function (14, 15, 16, 17).
The most efficacious regimen for long-term graft survival is not known. Additionally, no evidence of an SRL reversal of renal function or histology of renal grafts with impaired renal function has been published. The current study investigated the impact of SRL conversion therapy from CNI on graft function and histology after CNI exposure for a certain period.
This study was a 12-month, prospective, nonrandomized, two-center, open-label, noncomparative study that included a screening period, conversion of immunosuppressive agent, and a treatment period.
The current study was designed for patients who underwent kidney transplantation from 6 months to 5 yr prior to the screening point. CNI was gradually reduced by 25% of the initial dose each week enrollbeginning from the first administration of SRL (Rapamune®, Pfizer, Philadelphia, PA, USA). A loading dose of SRL was administered on the first day of conversion. The loading dose of SRL was determined based on the previous use of mycophenolate mofetil (MMF) or mycophenolic acid (MPA). MMF or MPA patients received a loading dose of 6 mg/day SRL on the first day and a maintenance dose of 2 mg/day SRL, which was adjusted to target trough levels of 7-15 ng/mL. Non-MMF or MPA patients received an SRL loading dose of 8 mg/day on the first day and a maintenance dose of 4 mg/day SRL, which was adjusted to target trough levels of 10-18 ng/mL. Prednisone or an equivalent dose of deflazacort was maintained with the preconversion dosage (5-10 mg/day). Mandatory protocol biopsies were performed during the preconversion period and 1 yr after conversion (Fig. 1).
This study evaluated whether SRL conversion therapy from CNI improved renal function in renal recipients with mild to moderate graft insufficiency. The secondary objective evaluated whether SRL conversion therapy improved histological results 12 months after conversion.
Kidney transplant recipients who were over 18 yr of age and who received CNI for at least 3 months before screening were included in the current study. To define mild to moderate renal insufficiency, we made the inclusion criteria according to renal function including estimated glomerular filtration and proteinuria. The inclusion criteria had a lower limit of estimated glomerular filtration rate of over 40 mL/min (eGFR) as measured by the Cockcroft-Gault formula at screening and an upper limit of proteinuria of 300 mg/day using a 24-hr urine collection to exclude grafts with irreversible damage. Twenty four hour urine collection was performed only for the patients who showed eGFR over 40 mL/min to skip unnecessary evaluation. Patients who underwent kidney transplantation 6 months to 5 yr prior to screening were enrolled. Exclusion criteria included combined organ transplantation with other organs, an acute rejection episode within 3 months, generalized or localized infection, abnormal chest radiographic findings, unstable angina or arrhythmia, malignancy within 5 yr or post-transplant lymphoproliferative disease (PTLD), and the administration of drugs with pharmacokinetic effects on SRL, such as terfenadine, cisapride, astemizole, pimozide, ketoconazole, voriconazole, and fluconazole. Additionally, patients with an allergic reaction history with SRL, hepatitis B or C, HIV positivity, pregnancy, breast feeding, or a major operation history within 4 weeks were excluded. Patients with leucopenia (≤3,000/µL), thrombocytopenia (≤100,000/µL), hypertriglyceridemia (≥400 mg/dL, fasting), hypercholesterolemia (≥300 mg/dL, fasting), or other abnormal lipid profiles (fasting HDL-c ≤30 mg/dL, or fasting LDL-c≥200 mg/dL) at screening were additionally excluded. The patients were divided into three groups according to the duration of CNI exposure: 1) 6 months-1 yr, 2) 1-3 yr, and 3) 3-5 yr. The changes in renal function and histological findings were evaluated in each group.
The safety of the immunosuppressive protocol was assessed by monitoring the frequency, severity, duration and relation with the study drug of adverse events throughout the study period, including episodes of serious infection, immunosuppression-related complications and deviations from the study protocol for any reason. Laboratory tests, including hematology, biochemistry and urinalysis, were performed at preconversion and 0, 2, 4, 8, 12, 20, 28, 36, 44, and 52 weeks after conversion. Protocol biopsies were performed at the screening point and 1 yr after conversion. Proteinuria and creatinine clearance (CCr) were measured using 24-hr urine collection at preconversion and 4, 12, 28, and 52 weeks after conversion.
All biopsy slides from the two centers were collected and reviewed by one pathologist who specialized in transplant kidney pathology. Histological changes in glomerula, tubules, interstitium and blood vessels were graded using the Banff 97 classification with the 2005 modifications (18, 19). Additionally, CNI toxicity was graded according to the modified Banff classification ("ah" score) suggested by Sis et al. (20). This modified "ah" scoring system is based on the number and shape of arterial hyalinization and graded as follows: score 0=no typical lesions of CNI arteriolopathy, score 1=replacement of degenerated smooth muscle cells by hyaline deposits in only one arteriole but no circular involvement, score 2=replacement of degenerated smooth muscle cells by hyaline deposits in more than one arteriole but no circular involvement, and score 3=replacement of degenerated smooth muscle cells by hyaline deposits with circular involvement and independent of the number of arterioles involved.
Continuous data were reported as the means±SD and compared using the two-sided Student's t-test or ANOVA. Comparisons between the groups for categorical variables were analyzed using the chi-square test and the Fischer's exact test. Serial laboratory findings were compared using the Wilcoxon method for nonparametric tests or a paired t-test. Statistical analysis was performed using SPSS for Windows (version 14.0; SPSS, Chicago, IL, USA). P values less than 0.05 were regarded as significant.
Written informed consents for participation in this study were obtained from all patients before participating in this clinical trial. Severance Hospital IRB (4-2006-0241), Seoul St. Mary's Hospital IRB (KCMC06MI158) and Korean FDA (Clinical Trials Management Division-344) approved this protocol.
The screening was conducted between March 2007 and December 2009. A total of 46 patients who underwent kidney transplantation 6 months to 5 yr prior to the screening time point, were screened. There were 39 living donor and 7 deceased donor kidney transplantations. One screening failure occurred due to a low eGFR under 40 mL/min. Forty-five patients were enrolled in the current study, and preconversion biopsies were performed in all enrolled patients. CNI was completely converted to SRL 4 weeks after loading SRL. Four patients dropped out during the 52-week study period because of one case of acute pancreatitis, one case of severe edema, and two cases of pneumonitis. Thirty-seven protocol biopsies (postconversion biopsy) were completed after the 52-week study period (Fig. 2).
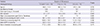
The mean age of enrolled patients was 37.1±10.9 yr. Thirty-eight male patients and 7 female patients were included. Twenty-eight patients received tacrolimus (62.2%), and 17 patients received cyclosporine (37.8%) prior to SRL conversion. The mean duration of CNI exposure after kidney transplantation was 28.6±16.8 months. Forty-three patients had used MMF or MPA, but two patients maintained their immunosuppression without antimetabolites. Ten of the 37 patients who completed the two protocol biopsies were exposed to CNI for 6 months to 1 yr, 16 patients for 1-3 yr and 11 patients for 3-5 yr after transplantation. No significant differences in preconversion clinical characteristics, such as sex, age, HLA mismatch, donor type, immunosuppressive agents, eGFR, proteinuria, and serum cholesterol level, were observed according to CNI exposure duration (Table 1).
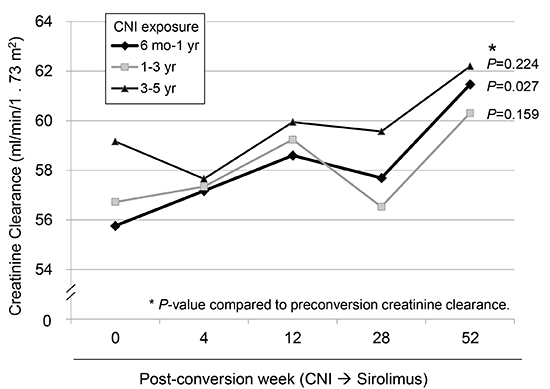
Serum creatinine at the screening point was 1.62±0.29 mg/dL, and it gradually decreased to 1.49±0.27 mg/dL 52 weeks later (P<0.001). CCr at preconversion was 57.28±10.93 mL/min/1.73 m2. CCr was mildly increased at 4, 12, 28, and 52 weeks after conversion. The CCr value 52 weeks after conversion was significantly increased to 61.21±11.51 mL/min/1.73 m2. CCr improvement was only revealed in patients who were exposed to CNI less than 1 yr (Fig. 3). Proteinuria increased at each measuring point, and it was significantly higher than at the preconversion period. The mean microprotein in the 24-hr urine collection was 101.8±51.5 mg/day (range: 12.0-221.0 mg/day) at the screening, and it gradually increased to 306.1±336.8 mg/day (range: 10.4-1,270.2 mg/day). Five patients (11.1%) exhibited proteinuria over 300 mg/day 4 weeks after conversion. Twelve patients (26.7%) exhibited proteinuria over 300 mg/day 52 weeks after conversion, and 3 of these patients had severe proteinuria over 1 g/day.
A total of 158 adverse events (AEs) were reported during the study period. The mean time of AEs was 3.5±1.9 times per person. Severe adverse events that required hospitalization occurred in 13 cases (8.2%). The most common AE was infection (39.6%) followed by digestive symptoms (18.2%) and metabolic events (15.1%), such as hyperlipidemia. The 63 events of infection included 49 (77.7%) upper respiratory infections, two (3.2%) urinary tract infections, two (3.2%) soft tissue infections, six (9.5%) viral infections, such as herpes zoster and herpes simplex, two (3.2%) fungal infections, and two (3.2%) pulmonary infections. Other AEs included skin rash, itching, oral ulcer, leg edema, myalgia, diabetes, anemia, androgenic alopecia, acute pancreatitis, heart failure, and arrhythmia. One case of acute rejection occurred during the study period, and this patient was rescued by steroid-pulse therapy. Serum total cholesterol, triglyceride and HDL cholesterol were measured on each visit (preconversion, 2, 4, 8, 12, 20, 28, 36, 44, and 52 weeks after conversion). Fig. 4 illustrates the trend of serum lipid profile changes during the study period. Total cholesterol levels rapidly increased from 189.2±45.3 mg/dL to 229.2±70.7 mg/dL in the 4 weeks after SRL conversion. Triglyceride and high-density lipoprotein levels also increased after SRL conversion. Thirty-one patients began antihypercholesterol drug (statin analogues) 122.5±78.5 days after SRL conversion. Only five patients remained statin-free 52 weeks after conversion. Serum cholesterol and triglyceride levels were controlled with the medication, and their mean levels were 193.2±35.6 mg/dL and 171.0±94.2 mg/dL, respectively, at 52 weeks.
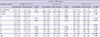
The histological changes are summarized in Table 2. Both pre- and postconversion biopsy samples were adequate for evaluation according to Banff 97 criteria (18). The proportions of global and segmental sclerosis increased from 7.6%±13.0% (range: 0%-57.0%) to 12.7%±19.0% (range: 0%-72.0%; P=0.023) and 0.9% ±4.8% (range: 0%-28.6%) to 2.1%±6.2% (range: 0%-33.3%; P=0.026), respectively, after SRL conversion. No significant differences in mean Banff scores were observed, except for the "ct" (tubular atrophy) score, which significantly increased 1 yr after conversion (P=0.012). An increase in the "ct" score was observed in the patients who were exposed to CNI for less than 3 yr.
No significant differences in modified "ah" scores between pre- and postconversion were observed in 1-yr biopsies (Fig. 5). Sixteen of the 37 patients who completed the current study (43.2%) exhibited no changes in histological CNI toxicity scores. An improved status in CNI toxicity, which was presented as a lower grade at postconversion biopsy than preconversion biopsy, was demonstrated in 10 patients (27.0%), but a worsened status was observed in 11 patients (29.8%). No significant differences in CNI toxicity between the three preconversion biopsy groups (early conversion within 1 yr after transplantation, intermediate conversion (1-3 yr after transplantation), and late conversion over 3 yr after transplantation were observed (Fig. 5B).
Early conversion is a better option than late conversion to avoid CNI toxicity or long-term graft survival (7, 8, 21). In a large multicenter study, the elimination of cyclosporine A (CsA) after 3 months from a protocol that contained SRL and CsA improved renal function, renal histology and graft survival (22, 23). However, no evidence of a time limit for the conversion of CNI to SRL or the irreversible renal change has been reported. In the current study, we extended the SRL conversion time to between 6 months and 5 yr after transplantation and included a protocol biopsy prior to and after SRL conversion.
Our study clearly demonstrated that SRL conversion improved renal function, but this effect was only observed in the patients who were exposed to CNI for less than 1 yr after transplantation. Moreover, this effect was not associated with histological improvements. These findings suggest a dissociation of function and histological improvement after SRL conversion, and histological improvement after SRL conversion cannot be expected one year after transplantation in patients with mild to moderate graft dysfunction.
The current study demonstrated improvements in renal function after SRL conversion, but no significant changes in histological findings were observed, especially in CNI toxicity. Although some patient demonstrated improved modified "ah" scores at 1 yr postconversion, other patients exhibited aggravated modified "ah" scores. Other scoring systems to evaluate CNI toxicity have replaced or modified the Banff score (20, 24). Kambham et al. (24) suggested a formula for CNI toxicity scoring using multiple histological parameters, such as glomerular sclerosis, tubular atrophy, arterial hyalinization, and tubular vacuolization. Our analysis of CNI toxicity using the scoring system suggested by Kambham et al. revealed post-conversion scores that were higher than preconversion scores (data not shown). However, the duration of CNI treatment was long enough to develop moderate to severe arteriolar changes, and the follow-up biopsies might have been performed too early for vessels to remodel their shapes. These results suggest that earlier conversion studies are required to prove the reversibility of SRL conversion.
No mechanisms of SRL conversion for the improvement of renal function have been revealed. Intrarenal hemodynamic change is one clue of this improvement. CNI use following kidney transplantation is associated with the development of vasomotor nephrotoxicity (25). The early phase of this toxicity is reversible by a reduction in CNI dosage. However, the continuous administration of CNI is associated with chronic vascular and tubulointerstitial lesions, which can cause irreversible nephropathy (26, 27). Therefore, the beneficial effect of early CNI withdrawal and SRL conversion is at least partially due to a decrease in intrarenal vascular resistance parameters (28). A functional improvement in SRL conversion patients who were exposed to CNI less than 1 yr was observed, but no histological improvement was observed. SRL can alter reversible intrarenal hemodynamicity in the early period, but it cannot reverse CNI-induced arteriopathy. A similar result was reported in another conversion study (29). The authors reported that the functional improvement in glomerular filtration rate in the conversion group was not associated with less interstitial fibrosis in protocol biopsies one year after transplantation. These results suggest that early conversion cannot prevent the progression of pathological damage.
Unfortunately, proteinuria is a well-known disadvantage of SRL conversion (30, 31, 32). The current study also demonstrated a rapid increase of proteinuria with SRL use. Proteinuria is the major concern of SRL conversion from CNI treatment. Proteinuria related to SRL is a controversial issue. Proteinuria after conversion from calcineurin inhibitors to SRL has been reported in several studies (30, 31, 32), but SRL may not be a direct factor for proteinuria (33). Proteinuria after SRL conversion could be related to the previous use of CsA but not SRL, but early SRL use with CsA elimination does not induce progressive proteinuria (33, 34). The current study demonstrated a rapid increase in proteinuria after SRL conversion. An SRL conversion study in chronic allograft dysfunction reported that intraglomerular pressure tended to increase, and renal functional reserve decreased significantly after SRL conversion form CNI, which was characteristic of hyperfiltration (35). This result may partially explain the increase in proteinuria after SRL use. Recently, Stallone et al. suggested that SRL-induced proteinuria may be a dose-dependent effect of the drug on key podocyte structures (36). The complete inhibition of mTORC1 activity with sirolimus treatment may worsen podocyte function and fail to yield a better clinical outcome because the PI3K-mTORC1 function in podocytes is essential for the maintenance of podocyte function and the integrity of the filtration barrier (37). Additionally, rapamycin treatment causes atrophy of the renal medulla in mice. The levels of rapamycin-sensitive phosphorylated S6 are higher in the tubular region under normal conditions, which suggests that renal tubular epithelial cells require relatively high mTORC1 activity for a constant turn-over and that tubular dysfunction or atrophy by prolonged mTORC1 inhibition may cause tubular proteinuria. Our data also demonstrated a significant increase in "ct" score after SRL conversion, and this increase in tubular atrophy may contribute to SRL-induced proteinuria.
Hyperlipidemia, oral ulcer, edema, anemia, and pneumonitis are related to SRL. Hyperlipidemia significantly affects long-term graft function (38). Hyperlipidemia is also closely related with SRL. However, SRL-induced hyperlipidemia generally responds to statin analogues (39). Thirty-one patients began statin analogues, and hyperlipidemia was well-controlled in the current study. A beneficial effect of SRL conversion on renal function as measured by serum creatinine and creatinine clearance was observed, especially in the patients who were converted to SRL within 1 yr after transplantation.
SRL conversion treatment can be safely applied to patients with mild to moderate renal insufficiency. However, SRL conversion should be considered within 1 yr after transplantation because the increased exposure to CNI negatively impacts histological features that may not be reversible, and it may be more difficult to improve CCr.
Figures and Tables
Fig. 1
Study design. After screening, calcineurin inhibitors were converted into sirolimus for a 4-week overlapped period (CNI dose was reduced by 25% each week). *Non-MMF and MPA patients received a loading dose of 8 mg/day and a maintenance dose of 4 mg/day. MMF, mycophenolate mofetil; MPA, mycophenolic acid; CNI, calcineurin inhibitor.

Fig. 2
Study population. Forty-six patients were screened, and 45 preconversion biopsies were performed. After the 52-week study period, 37 post-conversion biopsies were completed.
Fig. 3
Creatinine clearance before and after SRL conversion according to the CNI exposure period. *P value compared to preconversion creatinine clearance.

Fig. 5
Calcineurin inhibitor (CNI) toxicity in the biopsy. (A) Change of modified "ah" score. (B) Proportion of modified "ah" score according to exposure duration to CNI; preconversion versus postconversion 1 yr.

Notes
Funding: This investigator-initiated study was supported by Wyeth Korea, which was acquired by Pfizer Pharmaceuticals in 2010 (#102299[WS1234412], 2006).
The authors of this manuscript have conflicts of interest to disclose. DJJ, HJJ, BJL, IJ, KHH, BHC, YJC, and SWK have declared no conflicts of interest. YSK and CWY have participated in clinical trials sponsored by Astellas, Novartis, Roche, CKD, and Wyeth, and they have received research grants from Astellas, Novartis, Roche, and CKD. No one have stocks of the respective pharmaceutical companies.
References
1. Nankivell BJ, Borrows RJ, Fung CL, O'Connell PJ, Allen RD, Chapman JR. The natural history of chronic allograft nephropathy. N Engl J Med. 2003; 349:2326–2333.
2. Chapman JR, Nankivell BJ. Nephrotoxicity of ciclosporin A: short-term gain, long-term pain? Nephrol Dial Transplant. 2006; 21:2060–2063.
3. Bennett WM, DeMattos A, Meyer MM, Andoh T, Barry JM. Chronic cyclosporine nephropathy: the Achilles' heel of immunosuppressive therapy. Kidney Int. 1996; 50:1089–1100.
4. Lebranchu Y, Thierry A, Toupance O, Westeel PF, Etienne I, Thervet E, Moulin B, Frouget T, Le Meur Y, Glotz D, et al. Efficacy on renal function of early conversion from cyclosporine to sirolimus 3 months after renal transplantation: concept study. Am J Transplant. 2009; 9:1115–1123.
5. Meier-Kriesche HU, Steffen BJ, Chu AH, Loveland JJ, Gordon RD, Morris JA, Kaplan B. Sirolimus with neoral versus mycophenolate mofetil with neoral is associated with decreased renal allograft survival. Am J Transplant. 2004; 4:2058–2066.
6. Carvalho C, Coentrão L, Bustorff M, Patrício E, Sampaio S, Santos J, Oliveira G, Pestana M. Conversion from sirolimus to everolimus in kidney transplant recipients receiving a calcineurin-free regimen. Clin Transplant. 2011; 25:E401–E405.
7. Flechner SM. Sirolimus in kidney transplantation indications and practical guidelines: de novo sirolimus-based therapy without calcineurin inhibitors. Transplantation. 2009; 87:S1–S6.
8. Guba M, Pratschke J, Hugo C, Krämer BK, Nohr-Westphal C, Brockmann J, Andrassy J, Reinke P, Pressmar K, Hakenberg O, et al. Renal function, efficacy, and safety of sirolimus and mycophenolate mofetil after short-term calcineurin inhibitor-based quadruple therapy in de novo renal transplant patients: one-year analysis of a randomized multicenter trial. Transplantation. 2010; 90:175–183.
9. Han F, Wu J, Huang H, Zhang X, He Q, Wang Y, Wang S, Wang H, Chen J. Conversion from cyclosporine to sirolimus in chronic renal allograft dysfunction: a 4-year prospective study. Exp Clin Transplant. 2011; 9:42–49.
10. Höcker B, Tönshoff B. Calcineurin inhibitor-free immunosuppression in pediatric renal transplantation: a viable option? Paediatr Drugs. 2011; 13:49–69.
11. Oberbauer R, Kreis H, Johnson RW, Mota A, Claesson K, Ruiz JC, Wilczek H, Jamieson N, Henriques AC, Paczek L, et al. Long-term improvement in renal function with sirolimus after early cyclosporine withdrawal in renal transplant recipients: 2-year results of the Rapamune Maintenance Regimen Study. Transplantation. 2003; 76:364–370.
12. Campistol JM, Cockwell P, Diekmann F, Donati D, Guirado L, Herlenius G, Mousa D, Pratschke J, San Millán JC. Practical recommendations for the early use of m-TOR inhibitors (sirolimus) in renal transplantation. Transpl Int. 2009; 22:681–687.
13. Morales JM. Cardiovascular risk profile in patients treated with sirolimus after renal transplantation. Kidney Int Suppl. 2005; (93):S69–S73.
14. Schäffer M, Schier R, Napirei M, Michalski S, Traska T, Viebahn R. Sirolimus impairs wound healing. Langenbecks Arch Surg. 2007; 392:297–303.
15. Srivastava A, Muruganandham K, Vinodh PB, Singh P, Dubey D, Kapoor R, Kumar A, Sharma RK, Prasad N. Post-renal transplant surgical complications with newer immunosuppressive drugs: mycophenolate mofetil vs. m-TOR inhibitors. Int Urol Nephrol. 2010; 42:279–284.
16. Langer RM, Kahan BD. Incidence, therapy, and consequences of lymphocele after sirolimus-cyclosporine-prednisone immunosuppression in renal transplant recipients. Transplantation. 2002; 74:804–808.
17. Boratyńska M, Banasik M, Patrzalek D, Szyber P, Klinger M. Sirolimus delays recovery from posttransplant renal failure in kidney graft recipients. Transplant Proc. 2005; 37:839–842.
18. Racusen LC, Solez K, Colvin RB, Bonsib SM, Castro MC, Cavallo T, Croker BP, Demetris AJ, Drachenberg CB, Fogo AB, et al. The Banff 97 working classification of renal allograft pathology. Kidney Int. 1999; 55:713–723.
19. Solez K, Colvin RB, Racusen LC, Sis B, Halloran PF, Birk PE, Campbell PM, Cascalho M, Collins AB, Demetris AJ, et al. Banff '05 Meeting Report: differential diagnosis of chronic allograft injury and elimination of chronic allograft nephropathy ('CAN'). Am J Transplant. 2007; 7:518–526.
20. Sis B, Dadras F, Khoshjou F, Cockfield S, Mihatsch MJ, Solez K. Reproducibility studies on arteriolar hyaline thickening scoring in calcineurin inhibitor-treated renal allograft recipients. Am J Transplant. 2006; 6:1444–1450.
21. Weir MR, Mulgaonkar S, Chan L, Shidban H, Waid TH, Preston D, Kalil RN, Pearson TC. Mycophenolate mofetil-based immunosuppression with sirolimus in renal transplantation: a randomized, controlled Spare-the-Nephron trial. Kidney Int. 2011; 79:897–907.
22. Mota A, Arias M, Taskinen EI, Paavonen T, Brault Y, Legendre C, Claesson K, Castagneto M, Campistol JM, Hutchison B, et al. Sirolimus-based therapy following early cyclosporine withdrawal provides significantly improved renal histology and function at 3 years. Am J Transplant. 2004; 4:953–961.
23. Oberbauer R, Segoloni G, Campistol JM, Kreis H, Mota A, Lawen J, Russ G, Grinyó JM, Stallone G, Hartmann A, et al. Early cyclosporine withdrawal from a sirolimus-based regimen results in better renal allograft survival and renal function at 48 months after transplantation. Transpl Int. 2005; 18:22–28.
24. Kambham N, Nagarajan S, Shah S, Li L, Salvatierra O, Sarwal MM. A novel, semiquantitative, clinically correlated calcineurin inhibitor toxicity score for renal allograft biopsies. Clin J Am Soc Nephrol. 2007; 2:135–142.
25. Lanese DM, Conger JD. Effects of endothelin receptor antagonist on cyclosporine-induced vasoconstriction in isolated rat renal arterioles. J Clin Invest. 1993; 91:2144–2149.
26. Naesens M, Kuypers DR, Sarwal M. Calcineurin inhibitor nephrotoxicity. Clin J Am Soc Nephrol. 2009; 4:481–508.
27. Ojo AO, Held PJ, Port FK, Wolfe RA, Leichtman AB, Young EW, Arndorfer J, Christensen L, Merion RM. Chronic renal failure after transplantation of a nonrenal organ. N Engl J Med. 2003; 349:931–940.
28. Lee PC, Lee CY, Hu RH, Lo C, Tsai MK, Lee PH. Intrarenal vascular resistance parameters in kidney transplant patients receiving calcineurin inhibitor-based or sirolimus-based regimens. Nephrol Dial Transplant. 2010; 25:1675–1680.
29. Servais A, Meas-Yedid V, Toupance O, Lebranchu Y, Thierry A, Moulin B, Etienne I, Presne C, Hurault de LB, Le Pogamp P, et al. Interstitial fibrosis quantification in renal transplant recipients randomized to continue cyclosporine or convert to sirolimus. Am J Transplant. 2009; 9:2552–2560.
30. Franco AF, Martini D, Abensur H, Noronha IL. Proteinuria in transplant patients associated with sirolimus. Transplant Proc. 2007; 39:449–452.
31. Morelon E, Kreis H. Sirolimus therapy without calcineurin inhibitors: Necker Hospital 8-year experience. Transplant Proc. 2003; 35:52S–57S.
32. Bumbea V, Kamar N, Ribes D, Esposito L, Modesto A, Guitard J, Nasou G, Durand D, Rostaing L. Long-term results in renal transplant patients with allograft dysfunction after switching from calcineurin inhibitors to sirolimus. Nephrol Dial Transplant. 2005; 20:2517–2523.
33. Ruiz JC, Campistol JM, Sanchez-Fructuoso A, Mota A, Grinyo JM, Paul J, Castro-Henriques A, Reimao-Pinto J, Garcia J, Morales JM, et al. Early sirolimus use with cyclosporine elimination does not induce progressive proteinuria. Transplant Proc. 2007; 39:2151–2152.
34. Watson CJ, Gimson AE, Alexander GJ, Allison ME, Gibbs P, Smith JC, Palmer CR, Bradley JA. A randomized controlled trial of late conversion from calcineurin inhibitor (CNI)-based to sirolimus-based immunosuppression in liver transplant recipients with impaired renal function. Liver Transpl. 2007; 13:1694–1702.
35. Saurina A, Campistol JM, Piera C, Diekmann F, Campos B, Campos N, de las Cuevas X, Oppenheimer F. Conversion from calcineurin inhibitors to sirolimus in chronic allograft dysfunction: changes in glomerular haemodynamics and proteinuria. Nephrol Dial Transplant. 2006; 21:488–493.
36. Stallone G, Infante B, Pontrelli P, Gigante M, Montemurno E, Loverre A, Rossini M, Schena FP, Grandaliano G, Gesualdo L. Sirolimus and proteinuria in renal transplant patients: evidence for a dose-dependent effect on slit diaphragm-associated proteins. Transplantation. 2011; 91:997–1004.
37. Inoki K, Mori H, Wang J, Suzuki T, Hong S, Yoshida S, Blattner SM, Ikenoue T, Rüegg MA, Hall MN, et al. mTORC1 activation in podocytes is a critical step in the development of diabetic nephropathy in mice. J Clin Invest. 2011; 121:2181–2196.
38. Hernández D, Martínez D, Gutiérrez E, López V, Gutiérrez C, García P, Cobelo C, Cabello M, Burgos D, Sola E, et al. Clinical evidence on the use of anti-mTOR drugs in renal transplantation. Nefrologia. 2011; 31:27–34.
39. Sayin B, Karakayali H, Colak T, Sevmis S, Pehlivan S, Demirhan B, Haberal M. Conversion to sirolimus for chronic allograft nephropathy and calcineurin inhibitor toxicity and the adverse effects of sirolimus after conversion. Transplant Proc. 2009; 41:2789–2793.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download