Abstract
A 62-yr-old woman with an autosomal dominant polycystic kidney disease (ADPKD) was admitted to our hospital for further evaluation of intermittent fever, nausea and left flank discomfort. The computed tomography (CT) scan revealed a gas-forming, infectious cyst of approximately 8.1 cm in size in left kidney lower pole. Escherichia coli was identified from the cyst fluid culture examination. Her symptoms improved only after the concomitant use of intravenous ciprofloxacin and an intracystic irrigation of ciprofloxacin through a percutaneous cystostomy drainage. Our case presents the successfully treated emphysematous cyst infection with combination of intravenous antibiotics and intracystic antibiotic therapy instead of surgical management.
Autosomal dominant polycystic kidney disease (ADPKD) is one of the most common hereditary disorders in humans. It affects one in every 500 to 1000 live births, accounting for 8%-10% of total dialysis patients (1). Approximately 30%-50% of ADPKD patients have a urinary tract infection (UTI) during their lifetime. In addition, the incidence of cyst infection has been estimated at approximately 0.01 episode/person/year (2). Similar to the general population, UTI in ADPKD patients is usually caused by gram-negative enteric organisms which ascend from the lower urinary tract (3) and Escherichia coli-induced UTI or cyst infection accounts for approximately 75% of total cases (2). Vesicoureteral reflux, nephrolithiasis and urinary tract instrumentation can contribute to the occurrence of cyst infection. Moreover, non-functional end-stage polycystic kidneys themselves may also be the cause of UTI (4).
Emphysematous or gas-forming cyst infection is a rare disease but is important because of its life-threatening potential and an emergent nephrectomy is often considered the best treatment option (5). However, conservative management with antiobiotic therapy without surgical management has rarely been reported before. Herein, we present the emphysematous cyst infection case successfully treated with intravenous antibiotics and intracystic antibiotics irrigation without nephrectomy.
A 62-yr-old female ADPKD patient was admitted to our hospital for further evaluation of intermittent fever, nausea and left flank discomfort on April 26, 2012. The patient had a 15-yr-history of ADPKD that was detected when the patient was diagnosed with hypertension. Her two brothers also were diagnosed as ADPKD. However, the patient had no history of diabetes. The patient had been examined for ADPKD at our outpatient clinic since 2004. Despite a history of recurrent cyst hemorrhage, the patient achieved a full recovery from the hemorrhage with conservative management. In 2009, the patient was admitted for the treatment of suspicious cyst infection versus acute pyelonephritis. She received ciprofloxacin for the infection and had E. coli detected in the urine culture. Her renal function deteriorated progressively thereafter to begin hemodialysis from April 2011. Her daily urine output remained about 200 cc.
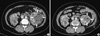
Two months before the current outpatient visit, she felt generalized weakness, anorexia, nausea and the discomfort in the left flank. She also developed intermittent fever with chilling sense one month prior to the visit. Therefore, the patient visited an emergency care center at the outside hospital to take CT scan which revealed about 8.1-cm large gas-forming cyst at the left kidney lower pole (Fig. 1A). Her initial laboratory findings showed WBC counts of 22,190/µL and CRP of 25.5 mg/dL. The urinary sediment contained numerous RBCs and WBCs per high power field. Despite a 1-week course of intravenous antibiotic therapy with ciprofloxacin, her fever and flank discomfort persisted and subsequently resulted in general weakness and anorexia. The patient was referred to our clinic for further treatment plan including left nephrectomy. On admission, the patient had the temperature 38.4℃ and the blood pressure was measured as 150/85 mmHg. On physical examination, the patient showed local tenderness in the left flank. However, there was no definite presence of the costovertebral angle tenderness.
On clinical laboratory findings, the patient had WBC counts 12,850/µL, hemoglobin 9.7 g/dL, platelet counts 348,000/µL, blood urea nitrogen 39 mg/dL, creatinine 7.76 mg/dL, albumin 3.3 mg/dL, CRP 6.79 mg/dL. The urinary sediment contained numerous RBCs and WBCs per high power field. Although her laboratory parameters partially improved after a 1-week course of intravenous antibiotic therapy, her symptoms did not improve. Therefore, she was determined to undergo percutaneous cystostomy drainage of a large gas-forming cyst. The cyst was aspirated under ultrasound guidance followed by the percutaneous cystostomy drainage on hospitalization day 2. On clinical laboratory tests, cyst aspiration had RBC counts 290,000/µL and WBC counts 180,000/µL (polymorphonuclear leukocytes 98%, lymphocytes 0% and others 2%). In addition, a gram-stain revealed many ( > 10) WBCs and many ( > 10) G(-) rods. Finally, a culture of the cyst aspirate yielded E. coli, but the blood and urine culture were negative.
The patient was started on intravenous ciprofloxacin at a daily dose of 400 mg for 1 week. This was followed by an intracystic irrigation of ciprofloxacin through a percutaneous cystostomy drainage for 6 days. For the intracystic irrigation, 100 mg (50 cc) of ciprofloxacin was mixed with 450 cc of normal saline.Then repeated irrigation with the antibiotics mixture was performed. Following the treatment, the symptoms such as generalized weakness, nausea and discomfort in the left flank improved. This was also accompanied with the normalization of laboratory parameters.
Following intravenous antibiotic therapy and intracystic antibiotic irrigation, the patient had the percutaneous cystostomy drainage removed. Her following CT scans showed decreased size of the infected cyst (8.1 to 4.7 cm) with internal mottled air attenuation (Fig. 1B). The patient was discharged with oral ciprofloxacin for 6 more weeks.
Emphysematous UTIs are rare, severe infections of the lower or upper urinary tract associated with gas formation and necrotizing infection. The host factors for emphysematous UTI are known to include diabetes, urinary tract obstruction, debilitated or immunocompromised status (6, 7). Most of the infections are caused by E. coli, Klebsiella, or a mixture of organisms. Gas formation is believed to require pathogenic bacterial strains that are capable of mixed acid fermentation consisting of carbon dioxide and nitrogen, a hyperglycemic milieu, local tissue ischemia, a depressed cell-mediated immune response, local tissue necrosis, and the presence of arteriosclerosis which exacerbates tissue destruction, promotes the purulent infection, and inhibits the removal of locally produced gas (1, 8). The treatment of emphysematous UTIs, especially emphysematous pyelonephritis are depends on the extent of infection and other clinical factors including percutaneous cystostomy drainage combined with antibiotic treatment and emergency nephrectomy (9, 10).
Emphysematous cyst infection is a specific entity of ADPKD patient and life threatening. Because of its scarcity, there are not definite guidelines of treatment. To date, antibiotic therapy combined with nephrectomy were conducted as a treatment (5, 11-13). As for antibiotic therapy, fluoroquinolones are usually favored because of their lipophilic properties that lead to an increased diffusion into infected cysts and their bactericidal activity against Gram-negative enteric pathogens (2). In addition, chloramphenicol, clindamycin, metronidazole, trimethoprim and vancomycin were also introduced as antibiotics showing relatively good intracystic diffusion (11-16). Meanwhile, even the single use of third-generation cephalosporins with poor cyst penetration has been reported to achieve a treatment success in non-emphysematous cyst infection in ADPKD (10). However, it is generally known that the antibiotic therapy alone may be insufficient because of the decreased antibiotic penetration into cysts. On the other hand, intracystic antibiotic irrigation may be an effective method to maintain an appropriate intracystic antibiotic concentration with relatively less complications.
Antibiotic treatment, including a fluoroquinolone, and the drainage of large (diameter > 5 cm) infected cysts is known to be the main treatment for cyst infections in ADPKD (5). Arun et al. (10) reported a successfully treated bilateral emphysematous pyelonephritis and emphysematous cystitis in ADPKD only with a medical treatment. However, there are rare data about emphysematous cyst infection with conservative management.
To date, only 4 cases of emphysematous cyst infection have been reported. All of them were developed in end stage polycystic kidneys. In addition, it has also been reported that E. coli and Clostridium perfringens are identified from the different cases. Zijl et al. (17) reported an emphysematous infection in the right renal cyst which had been a hemorrhagic cyst for seven months before infection developed. The patient underwent kidney transplantation after infection was controlled. Lanzas et al. (18) reported a hemodialysis patient with ADPKD who presented with sepsis secondary to infection of the renal cyst with gas formation. Erkoc et al. (19) also presented an emphysematous cyst infection in a ADPKD patient on hemodialysis. Sooraj et al. (5) reported an emphysematous cyst infection in a nondiabetic ADPKD patient who failed to recover and succumbed to the illness. All of them were treated with urgent nephrectomy and three of them were successfully treated. To the best of our knowledge, our patient is the fifth case of emphysematous cyst infection in ADPKD patient. More importantly, it is the first case of emphysematous cyst infection that was successfully treated by combination of intravenous antibiotic therapy and intracystic antibiotic irrigation through a percutaneous cystostomy drainage.
In summary, our case presents successfully treated emphysematous cyst infection with combination of intravenous antibiotics and intracystic antibiotic therapy instead of surgical management. The current case is meaningful because of its rarity and of a new therapeutic approach. Although many non-emphysematous cyst infections and some emphysematous UTIs were well treated with only medical treatment, intravenous antibiotic therapy alone may be insufficient to resolve emphysematous cyst infection in a short period of time considering its disease severity and poor prognosis. A percutaneous cystostomy drainage and intracystic antibiotic irrigation may be one of the alternative therapeutic options to control emphysematous cyst infection instead of surgical kidney removal in ADPKD patients. However, it needs to be carefully considered in the patients who failed to reach clinical improvement with intravenous antibiotics alone or who are not able to go through surgical nephrectomy due to general condition.
Figures and Tables
Fig. 1
Comparison of intravenous contrast-enhanced CT scans between at diagnosis and on day 6 following the treatment. (A) A 8.1-cm sized complicated cyst is displayed in left kidney lower pole with air-mottled soft tissue density. (B) The cyst decreased of its size to 4.7 cm with internal mottled air attenuation after 6-days antibiotics irrigation through percutaneous cystostomy drainage.
References
1. Gabow PA. Autosomal dominant polycystic kidney disease. N Engl J Med. 1993; 329:332–342.
2. Sallée M, Rafat C, Zahar JR, Paulmier B, Grünfeld JP, Knebelmann B, Fakhouri F. Cyst infections in patients with autosomal dominant polycystic kidney disease. Clin J Am Soc Nephrol. 2009; 4:1183–1189.
3. Ubara Y, Takei R, Hoshino J, Tagami T, Sawa N, Yokota M, Katori H, Takemoto F, Hara S, Takaichi K. Intravascular embolization therapy in a patient with an enlarged polycystic liver. Am J Kidney Dis. 2004; 43:733–738.
4. Stiasny B, Ziebell D, Graf S, Hauser IA, Schulze BD. Clinical aspects of renal transplantation in polycystic kidney disease. Clin Nephrol. 2002; 58:16–24.
5. Sooraj YS, Nainan GK, Joseph F, Thara P. Emphysematous polycystic renal infection. Indian J Nephrol. 2010; 20:205–206.
6. Cosentini V, Cosaro A, Gammaro L, Lidestri V, Oldrizzi L, Maschio G. Escherichia coli-induced emphysematous pyelonephritis in a diabetic patient with polycystic kidney disease. G Ital Nefrol. 2011; 28:85–88.
7. Tseng CC, Wu JJ, Wang MC, Hor LI, Ko YH, Huang JJ. Host and bacterial virulence factors predisposing to emphysematous pyelonephritis. Am J Kidney Dis. 2005; 46:432–439.
8. Turney JH. Renal conservation for gas-forming infections. Lancet. 2000; 355:770–771.
9. Huang JJ, Tseng CC. Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med. 2000; 160:797–805.
10. Arun N, Hussain A, Kapoor MM, Abul F. Bilateral emphysematous pyelonephritis and emphysematous cystitis with autosomal-dominant polycystic kidney disease: is conservative management justified? Med Princ Pract. 2007; 16:155–157.
11. Bennett WM, Elzinga L, Pulliam JP, Rashad AL, Barry JM. Cyst fluid antibiotic concentrations in autosomal-dominant polycystic kidney disease. Am J Kidney Dis. 1985; 6:400–404.
12. Elzinga LW, Golper TA, Rashad AL, Carr ME, Bennett WM. Ciprofloxacin activity in cyst fluid from polycystic kidneys. Antimicrob Agents Chemother. 1988; 32:844–847.
13. Elzinga LW, Golper TA, Rashad AL, Carr ME, Bennett WM. Trimethoprim-sulfamethoxazole in cyst fluid from autosomal dominant polycystic kidneys. Kidney Int. 1987; 32:884–888.
14. Hiyama L, Tang A, Miller LG. Levofloxacin penetration into a renal cyst in a patient with autosomal dominant polycystic kidney disease. Am J Kidney Dis. 2006; 47:e9–e13.
15. Suwabe T, Ubara Y, Sumida K, Hayami N, Hiramatsu R, Yamanouchi M, Hasegawa E, Hoshino J, Sawa N, Saitoh S, et al. Clinical features of cyst infection and hemorrhage in ADPKD: new diagnostic criteria. Clin Exp Nephrol. 2012; 16:892–902.
16. Schwab SJ, Weaver ME. Penetration of trimethoprim and sulfamethoxazole into cysts in a patient with autosomal-dominant polycystic kidney disease. Am J Kidney Dis. 1986; 7:434–438.
17. Van Zijl PS, Chai TC. Gas-forming infection from Clostridium perfringens in a renal cyst of a patient with autosomal dominant polycystic kidney disease. Urology. 2004; 63:1178–1179.
18. Lanzas Prieto JM, Alonso De La Campa JM, Pérez García FJ, Gutiérrez García R, González Tuero J, Guate Ortiz JL. Pneumopyocystitis in a patient with adult polycystic kidney disease. Arch Esp Urol. 2003; 56:536–538.
19. Erkoc R, Sayarlioglu H, Ceylan K, Dogan E, Kara PS. Gas-forming infection in a renal cyst of a patient with autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 2006; 21:555–556.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download