Abstract
Percutaneous catheter-based therapy has recently been introduced to decrease blood pressure by ablation of efferent and afferent sympathetic renal nerves. The patient described here had a seven-year history of hypertension and presented with poorly controlled blood pressure despite antihypertensive therapy with four different drugs. A 44-yr-old man underwent percutaneous renal denervation under local anesthesia using an ablation catheter. After six months of follow-up his blood pressure had dropped 49/37 mmHg with a decrease in 24-hr ambulatory BP of 20/18 mmHg. Renal Doppler ultrasound showed no significant stenosis in either renal artery. This is the first case of successful percutaneous renal denervation, which has recently become available in Korea.
The renal sympathetic nervous system has been identified as a major contributor to the complex pathophysiology of hypertension and states of volume overload such as heart failure in humans (1, 2). Recently, catheter-based renal sympathetic denervation (RDN) has been introduced as a new technique to reduce blood pressure (BP) by denervation of efferent and afferent renal sympathetic nerve fibers using radiofrequency ablation (3, 4). Here we describe the first of these procedures performed in Korea on a 44-yr old male with resistant hypertension complicated by heart failure. He successfully underwent percutaneous RDN with a significant reduction in BP after six months of follow-up.
Optimal BP could not be achieved in a 44-yr-old man with a seven-year history of hypertension despite antihypertensive therapy with four different drugs. He had a 30-pack-year smoking history with a body mass index of 33.4 kg/m2, no history of diabetes, and a family history of early coronary artery disease. The patient first visited to our hospital with chronic headache on september 1, 2008. His antihypertensive medications consisted of hydrochlorothiazide 12.5 mg and felodipine 5 mg once a day, and carvedilol 25 mg and valsartan 160 mg twice a day. His average office BP was 170/115 mmHg and his 24 hr-ambulatory BP was 167/113 mmHg with a non-dipping profile (Fig. 1A).
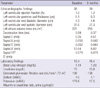
The patient underwent the established clinical and laboratory evaluation to identify essential hypertension, and he did not have any secondary causes of hypertension (5). A physical examination revealed no abnormal findings. Resting electrocardiography revealed a normal sinus rhythm with left ventricular hypertrophy diagnosed using voltage criteria. N-terminal probrain natriuretic peptide, renin activity, aldosterone were 47.8 pg/mL (normal < 88 pg/mL), 0.5 ng/mL/hr (0.15 to 3.95 ng/mL/hr) and aldosterone was 4.0 ng/dL (1.0 to 27.3 ng/dL), respectively. In addition, other laboratory and his transthoracic echocardiographic findings were shown in Table 1. Computed tomography showed bilateral renal artery length > 20 mm, lumen diameter > 4 mm, and no significant atherosclerotic plaques.
He underwent percutaneous RDN under local anesthesia with midazolam and fentanyl. First, a 6 French sheath was inserted into the right femoral artery and 5000 units of heparin were injected intravenously. Renal angiography was performed through a 5 French pigtail catheter (Cordis, Miami Lakes, FL, USA). Then, a 6 French renal double curve guide catheter (Cordis, Miami Lakes, FL, USA) was inserted to engage the left renal artery. Using an ablation catheter (Symplicity, Ardian, Medtronic), five radiofrequency ablations (Fig. 2B) were delivered to the left renal artery and six (Fig. 2E) were delivered to the right renal artery. Final angiographic findings were acceptable, and did not experience any complications such as significant stenosis, dissection, or spasm (Fig. 2C, F).
After four weeks of follow-up, his average office BP was 144/90 mmHg and his 24 hr-ambulatory BP was 145/94 mmHg. Six months post-procedure, an average office BP of 121/78 mmHg and 24-hr ambulatory BP of 147/95 mmHg were noted (Fig. 1B). Moreover, the patient did not complain of chronic headaches anymore and his microalbuminuria was decreased with an albumin to creatinine ratio of 17.5 µg/mgCr. Renal Doppler ultrasound showed no significant stenosis in either renal artery, but there was no change in his left ventricular ejection fraction, diastolic function and right ventricular systolic function (Table 1).
This case is the first successful percutaneous RDN performed for the treatment of a hypertensive patient with congestive heart failure in Korea. Hyperactivation of the sympathetic nerve system plays a major role in initiating and maintaining hypertension, and enhanced nerve activity in hypertensive patients may contribute to subsequent target organ damage such as left ventricular hypertrophy, congestive heart failure, and progressive renal damage (1, 2, 6-8). Surgical renal denervation has been performed to lower blood pressure in patients with hypertension, but the invasive nature of this approach is associated with a high incidence of complications (3). However, a percutaneous catheter-based device using radiofrequency ablation has recently been introduced to interrupt both efferent and afferent renal nerves located in the adventitia of the renal artery (9). The key clinical study supporting this technique, Symplicity HTN-2, was a multicenter, prospective, randomized controlled trial in patients aged 18-85 yr with a systolic blood pressure of 160 mm Hg or more ( ≥ 150 mm Hg in patients with type 2 diabetes), despite compliance with three or more antihypertensive drugs, showing a significant decrease in office BP of 32/12 mmHg after six months of follow-up in 49 patients who underwent RDN. Measurements of 24-hr ambulatory BP recordings were available for 20 patients in the RDN group in that study, showing a mean decrease of 11/7 mmHg at six months (10). In our case, the drop in office BP was 49/37 mmHg with a decrease in 24-hr ambulatory BP of 20/18 mmHg after six months of follow-up.
Considering data obtained from Western populations (3, 10, 11), our results suggest that percutaneous RDN could also be an effective and safe strategy for the treatment of resistant hypertension in Asian populations. Furthermore, in hypertensive patients with heart failure and left ventricular systolic dysfunction like our patient, the beneficial effects of this procedure might extend beyond a decrease in BP and involve the repair of end organ damage because conditions such as hypertension, heart failure, and kidney injury are commonly associated with sodium retention or systemic sympathetic hyperactivity albeit by different mechanisms (3). Our patient's microalbuminuria was improved although there was no change in his left ventricular systolic function. Further research is needed to investigate the benefit of this procedure for the treatment of various conditions such as heart failure and hypertension.
In summary, we reported the first successful experience with percutaneous RDN as a new technique for the treatment of hypertension. Our findings indicate that percutaneous RDN might be an effective and safe therapeutic tool in Asian populations with resistant hypertension.
Figures and Tables
 | Fig. 1Monitoring of 24-hr ambulatory blood pressure (BP). (A) At baseline showing poorly controlled BP (average systolic/diastolic BP = 167/113 mm Hg). (B) After 6 months of follow-up showing suboptimally-controlled BP (average systolic/diastolic BP = 147/95 mmHg). |
 | Fig. 2Renal angiographies baseline image showing no significant stenosis in the left (A) or right renal artery (D). While the catheter was withdrawn proximally, five radiofrequency ablations were delivered to the left renal artery (B) while six were delivered to the right renal artery (E). Final angiographic findings were acceptable and did not show any complications in the left (C) or right renal artery (F). |
References
1. Schlaich MP, Sobotka PA, Krum H, Whitbourn R, Walton A, Esler MD. Renal denervation as a therapeutic approach for hypertension: novel implications for an old concept. Hypertension. 2009; 54:1195–1201.
2. DiBona GF. The sympathetic nervous system and hypertension: recent developments. Hypertension. 2004; 43:147–150.
3. Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus K, Kapelak B, Walton A, Sievert H, Thambar S, et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet. 2009; 373:1275–1281.
4. Mahfoud F, Cremers B, Janker J, Link B, Vonend O, Ukena C, Linz D, Schmieder R, Rump LC, Kindermann I, et al. Renal hemodynamics and renal function after catheter-based renal sympathetic denervation in patients with resistant hypertension. Hypertension. 2012; 60:419–424.
5. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, et al. 2007 ESH-ESC practice guidelines for the management of arterial hypertension: ESH-ESC task force on the management of arterial hypertension. J Hypertens. 2007; 25:1751–1762.
6. Thomas G, Shishehbor MH, Bravo EL, Nally JV. Renal denervation to treat resistant hypertension: guarded optimism. Cleve Clin J Med. 2012; 79:501–510.
7. Mancia G, Grassi G, Giannattasio C, Seravalle G. Sympathetic activation in the pathogenesis of hypertension and progression of organ damage. Hypertension. 1999; 34:724–728.
8. Davies JE, Manisty CH, Petraco R, Barron AJ, Unsworth B, Mayet J, Hamady M, Hughes AD, Sever PS, Sobotka PA, et al. First-in-man safety evaluation of renal denervation for chronic systolic heart failure: primary outcome from REACH-Pilot Study. Int J Cardiol. 2013; 162:189–192.
9. Sobotka PA, Krum H, Böhm M, Francis DP, Schlaich MP. The role of renal denervation in the treatment of heart failure. Curr Cardiol Rep. 2012; 14:285–292.
10. Symplicity HTN-2 Investigators. Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Böhm M. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet. 2010; 376:1903–1909.
11. Voskuil M, Verloop WL, Blankestijn PJ, Agostoni P, Stella PR, Doevendans PA. Percutaneous renal denervation for the treatment of resistant essential hypertension; the first Dutch experience. Neth Heart J. 2011; 19:319–323.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download