Abstract
The aims of this study were to investigate whether early arterial blood gas analysis (ABGA) could define the severity of disease in infants with congenital diaphragmatic hernia (CDH). We conducted a retrospective study over a 21-yr period of infants diagnosed with CDH. Outcomes were defined as death before discharge, and extracorporeal membrane oxygenation requirements (ECMO) or death. A total 114 infants were included in this study. We investigated whether simplified prediction formula [PO2-PCO2] values at 0, 4, 8, and 12 hr after birth were associated with mortality, and ECMO or death. The area under curve (AUC) of receiver operating characteristic curve was used to determine the optimum ABGA values for predicting outcomes. The value of [PO2-PCO2] at birth was the best predictor of mortality (AUC 0.803, P < 0.001) and at 4 hr after birth was the most reliable predictor of ECMO or death (AUC 0.777, P < 0.001). The value of [PO2-PCO2] from ABGA early period after birth can reliably predict outcomes in infants with CDH.
Congenital diaphragmatic hernia (CDH) is an uncommon condition and occurs in 1 in 2,500 to 5,000 live births (1-4). Despite advances in prenatal diagnosis and neonatal intensive care, the mortality rates from CDH remains high, ranging from 20% to 75% with great variability between centers (5-8). In addition, abnormal pulmonary development results in lung hypoplasia, and several factors including persistent pulmonary hypertension (1, 2, 4) and combined anomalies are associated with high mortality and morbidity in CDH cases. The mortality risk from CDH is high when the patient is symptomatic within the first few hours after birth (9). Several parameters have been proposed to define the severity of this disease and to predict preand post-birth outcomes in affected cases. Prenatal ultrasound findings (4, 10-14), postnatal clinical findings (5, 9, 15-18), and ventilation, oxygenation parameters and arterial blood gas values (3, 5, 15-21) have been described in previous reports of CDH. However, Datin-Dorriere et al. (14) previously reported that prenatal factors alone could not predict neonatal outcomes accurately in CDH patients. Thus, the relationship between arterial blood gas analysis (ABGA) values as indicators of inadequate lung development in CDH patients has been suggested as predictors for outcomes (5, 15-17, 21-24).
We here conducted a retrospective study of CDH patients in the neonatal intensive care unit (NICU) of a single center to investigate whether early blood gas analysis could predict mortality, extracorporeal membrane oxygenation (ECMO) requirements or death in infants with CDH.
From 1990 to 2010, 141 patients with CDH were admitted to the NICU of the Asan Medical Center. Among these cases, 114 inborn infants were enrolled in the study. The remaining 27 infant patients who had been transferred from other hospitals were excluded. The medical records were reviewed retrospectively for demographic and clinical data including gender, birth weight, gestational age at birth, Apgar score, delivery mode, results of ABGA at 0, 4, 8, and 12 hr after birth, duration of mechanical ventilation, requirement for ECMO, and the day of admission and discharge. Outcomes were defined as death before discharge, requirement for ECMO therapy or death (ECMO/death), and duration of mechanical ventilation.
All infants who were prenatally diagnosed with CDH were intubated at birth and given ventilation support. These patients were sedated with continuous fentanyl infusion and/or a muscle relaxant. However, muscle relaxants were used only in selected cases at the discretion of attending physician. We applied high frequency oscillatory ventilation (HFOV) when CO2 retention or hypoxemia was persistent, despite a high conventional ventilator setting (peak inspiratory pressure > 25 cm H2O). We considered the use of inhaled nitric oxide (NO) when the oxygen index (OI) was > 25, and administering ECMO when the OI was > 40, despite the maximal support with HFOV and inotropics. An ABGA was performed at admission in all cases ( < 1 hr after birth) and at least every 4 hr up to the first 24 hr of life. ECMO treatments commenced at our institution in 2008.
A simplified prediction formula using early ABGA was developed based on our clinical experience and other prediction formulas reported in previous studies (3, 5, 25). Likely outcomes were assessed using a simplified prediction formula, [PO2-PCO2], at 0 ( < 1 hr after birth), 4, 8, and 12 hr after birth. Postductal arterial blood samples were obtained mostly via an umbilical artery catheter but infrequently via a peripheral arterial line. We used ABGA results within one hour before or after the 4, 8, 12 hr timepoints after admission. Our hypothesis was that a [PO2-PCO2] value > 0 was a predictor of a good clinical outcome in CDH patients.
Death before hospital discharge was a primary outcome variable. The ECMO requirements or death, and duration of mechanical ventilation were secondary outcomes. We compared the accuracy of our simplified prediction formula in predicting mortality in CDH patients using The Congenital Diaphragmatic Hernia Study Group (CDHSG) prediction formula: 1-1/(1+e-x); -x = -5.024+0.9165*(birth weight in kilograms) +0.4512*5-min Apgar score (5). The Fisher's exact test and two-sample t-test were used to test the correlation between the simplified prediction formula values and the primary and secondary outcomes. The area under curve (AUC) of receiver operating characteristic curve was used to determine the optimum ABGA values for predicting outcomes. An AUC of 0.5 is completely random whereas an AUC of 1.0 indicates perfect discrimination. Values between 0.7 and 0.8 are considered acceptable, and values greater than 0.8 are considered excellent. All analyses were performed using SPSS 17.0 software (Chicago, IL, USA).
A total of 114 CDH patients were enrolled as the study population. The baseline characteristics and postnatal management of survivor and non-survivor groups within this cohort are indicated in Table 1. Thirty-five (30.7%) of these 114 patients died and 11 (9.6%) cases required ECMO therapy. Fourteen (12.3%) babies were preterm (with the lowest gestational age at 28+6 weeks). Survivors and non-survivors were similar in birth weight, gender, and delivery mode. However, survivors showed higher gestational age at birth, higher 1 min and 5 min Apgar scores, and higher pH, lower PCO2, and higher PO2 in initial ABGA, and a lower incidence of pneumothorax. In addition, a smaller proportion of surviving patients required HFOV, NO, surfactant, inotropics support, and ECMO compared with the non-survivor group.
The overall survival rate in our cohort was 69.3% during the study period. The survival rates every five years during the study period were 20% early in this period (4 deaths among 5 patients, 1990-1995), and then measured at 71.4% (4 deaths among 14 patients, 1996-2000), 60.9% (9 deaths among 23 patients, 2001-2005), and 75% (18 deaths among 72 patients, 2006-2010). Overall, 79 neonates in our retrospective cohort survived to discharge with the median length of hospital stay of 21.0 days (range, 7 to 363 days). The mean duration of assisted ventilation was 9.5 days (range, 0 to 371 days). All of our CDH patients underwent ABGA initially after birth but 13 patients did not have ABGA data at 4 hr, 15 patients did not have these data at 8 hr, and 11 patients did not have a record of these results at 12 hr post-birth.
The values of our simplified prediction formula [PO2-PCO2] at 0, 4, 8, and 12 hr after birth were found to be associated with mortality (P < 0.001 at 0 hr, P = 0.005 at 4 hr, P = 0.008 at 8 hr, and P < 0.001 at 12 hr). A [PO2-PCO2] value of less than 0 (negative value) (P < 0.001 at 0, 4, 8, and 12 hr) and the [PO2-PCO2] value itself could also predict mortality. On ROC curve analysis to predict mortality, the initial [PaO2-PaCO2] (AUC = 0.803) showed better discrimination than the CDHSG formula (AUC = 0.740) (Fig. 1). The initial [PaO2-PaCO2] had the highest AUC (0.803) compare to those of other timepoints, at 4 hr (AUC = 0.757), at 8 hr (AUC = 0.787), and at 12 hr (AUC = 0.737). We obtained the best cut-off values to predict mortality with the simplified prediction formula; initial [PO2-PCO2] from the ROC curve (Fig. 1). In addition, the simplified prediction formula showed statistical significance (P < 0.001), and a cut-off value of ≤ [-15.61] showed a 68.6% sensitivity and 88.6% specificity for predicting mortality. The mortality rate was measured at 55.3% (26 of 47) among patients in a group with an initial [PO2-PCO2] value of < 0, and 72.7% (24 of 33) for patients in a group with an initial [PO2-PCO2] value of ≤ [-15.61].
With regard to ECMO requirement or death outcomes in patients with CDH, the [PO2-PCO2] values at 0 hr (P = 0.003), 4 hr (P < 0.001), 8 hr (P = 0.003), and 12 hr (P < 0.001) after birth were found to be statistically reliable, and the CDHSG formula also showed statistical significance (P < 0.001). The [PO2-PCO2] value at 4 hr post-birth was found to be the most reliable predictor of ECMO requirement or death (Fig. 2). On ROC curve analysis, [PaO2-PaCO2] at 4 hr had the highest AUC (0.777), and AUC at initial was 0.774, at 8 hr was 0.770, and at 12 hr was 0.768. Therefore, AUC of CDHSG formula for ECMO requirement or death was 0.759.
We did not find any association in our current analyses between the duration of mechanical ventilation and the [PO2-PCO2] values at 0 hr (P = 0.232), 4 hr (P = 0.408), 8 hr (P = 0.371), and 12 hr (P = 0.279) after birth.
Various studies have previously examined the relationship between ABGA values as ventilation/oxygenation parameters and survival outcomes in CDH patients (5, 15-17, 21-25). However, pulmonary hypertension, a variable ventilator setting, an endotracheal tube position, and other lung conditions, including combined respiratory distress syndrome, can also affect arterial blood gas values as well as lung hypoplasia. Therefore, Numanoglu et al. (10) have emphasized that the inspired concentration of oxygen and PaO2 are closely associated with the VI and PaCO2. Among various parameters, postductal PaO2 has been reported to reflect the degree of pulmonary perfusion and pulmonary vascular size (22) and Bohn et al. (19, 24) have confirmed the relationship between the PaCO2 level and a diagnosis of pulmonary hypoplasia, with postmortem lung measurements. We found that the PaO2 and PaCO2 values from same blood sample reflect the degree of pulmonary hypoplasia in patients with CDH without the interfering effects of other conditions or the ventilator settings. In the case of the previously reported the Wilford Hall/Santa Rosa clinical prediction formula (WHSR[PF]) (3), the PaO2 and PaCO2 values used were from ABGA measurements of different samples during the initial 24 hr of life. Hence, the WHSR(PF) uses the highest PaO2 and PaCO2 blood gas values during the initial 24 hr post-birth and would not enable to predict survival soon after birth. The CDH study group (5) has previously reported a CDHSG prediction formula by which clinicians can assess risk in CDH infants using birth weights and 5-min Apgar scores soon after birth. However, because the CDHSG formula is quite complex to use in a bedside setting and does not reflect the clinical status of the infant after birth, including the presence of respiratory failure, we developed a simplified formula to predict mortality in infants with CDH immediately after birth.
Schultz et al. (3) have reported that a reversed arterial level of PCO2 and PO2 reflects compromised gas exchange in patients with critical pulmonary hypoplasia. They proposed a WHSR (PF) cut-off value of greater than 0 as a predictor of survival. We first identified the relationship between a negative [PO2-PCO2] value within one hour of birth and mortality outcomes (P < 0.001). Moreover, the [PO2-PCO2] value as a continuous variable also was found to be a statistically significant predictor of mortality in our current analysis (P < 0.001). Using ROC curve analysis (Fig. 1), an optimal cut-off value of initial [PO2-PCO2] value for differentiating survivor from non-survivors with CDH was (-15.61). We initially expected that a [PO2-PCO2] value greater than 0 would predict survival, but found that an initial [PO2-PCO2] after birth reading of less than [-15.61] (72.7% mortality) showed a better discriminatory ability to predict death or survival than an initial [PO2-PCO2] of less than 0 (55.3% mortality).
In comparison with the previously reported CDHSG prediction formula (AUC = 0.740, P < 0.001) with a cut-off value of 0.61, our current simple prediction formula was found to be more effective in predicting the survival of CDH infants (AUC = 0.803, P < 0.001) (Fig. 1). Both the previously reported CDHSG prediction formula and the simple prediction formula we developed in our current study can be used to predict clinical outcomes of CDH cases immediately after birth. However, the Apgar score used in the CDHSG formula is affected by operator subjectivity (3) and the degree of pulmonary hypoplasia cannot be determined with only the Apgar score and birth weight (25).
In predicting the likelihood of an ECMO requirement or death, the [PaO2-PaCO2] value at 4 hr (AUC = 0.777) was found to be the most reliable predictor (Fig. 2). Although the [PaO2-PaCO2] value at 4 hr (AUC = 0.777) was better predictor than the initial [PaO2-PaCO2] for ECMO requirement or death in CDH infants, but the initial [PaO2-PaCO2] also has high AUC (0.774). Frenckner et al. (9) and Bohn (20) have previously reported that both the onset of symptoms and the A-aDO2 levels within 6 hr of birth could help to discriminate between survivors and nonsurvivors. However, patients with CDH could have various degrees of pulmonary hypoplasia from the fetal period and ABGA measurements immediately after birth also could reflect lung hypoplasia and be used as a predictor of mortality, consistent with our current findings.
This study has some limitations. First, this study was conducted retrospectively, thus some of the results of ABGA at certain timepoint were not collected. Second, the number of study population and the patients who were dead or underwent ECMO were small. Although this study has some limitations, this study was the single institution report of the largest population with CDH in Korea (26, 27). We assume that the physician could predict the outcomes or requirement of ECMO with this formula in patients with CDH soon after birth. Our simplified prediction formula requires further validation but might prove to be a useful tool and an easily applicable predictor of outcomes in patients with CDH.
In conclusion, we propose a simple mathematical equation, [PaO2-PaCO2], using initial ABGA values to reliably predict mortality, and the risk of ECMO or death in CDH patients.
Figures and Tables
Fig. 1
Comparison of receiver operating characteristic (ROC) curves the simplified prediction formula at birth with the CDHSG formula in the prediction of mortality outcomes in congenital diaphragmatic hernia. The simplified prediction formula at birth (initial [PaO2-PaCO2], AUC 0.803) showed better discrimination than the CDHSG formula (AUC 0.740) in the prediction of mortality outcomes with higher area under curve (AUC) value of ROC curve.
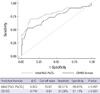
Fig. 2
Comparison of receiver operating characteristic (ROC) curves for the CDHSG formula with those for the simplified prediction formula at 4, 8, and 12 hr post-birth in predicting extracorporeal membrane oxygenation (ECMO) or death outcome in congenital diaphragmatic hernia. Based on ROC curve, the [PaO2-PaCO2] at 4 hr had the highest area under curve (AUC) (0.777) and Congenital Diaphragmatic Hernia Study Group (CDHSG) prediction formula had the lowest AUC (0.759) in predicting ECMO or death outcome.

References
1. Van Loenhout RB, Tibboel D, Post M, Keijzer R. Congenital diaphragmatic hernia: comparison of animal models and relevance to the human situation. Neonatology. 2009. 96:137–149.
2. De Buys Roessingh AS, Dinh-Xuan AT. Congenital diaphragmatic hernia: current status and review of the literature. Eur J Pediatr. 2009. 168:393–406.
3. Schultz CM, DiGeronimo RJ, Yoder BA. Congenital Diaphragmatic Hernia Study Group. Congenital diaphragmatic hernia: a simplified postnatal predictor of outcome. J Pediatr Surg. 2007. 42:510–516.
4. Thébaud B, Azancot A, de Lagausie P, Vuillard E, Ferkadji L, Benali K, Beaufils F. Congenital diaphragmatic hernia: antenatal prognostic factors: does cardiac ventricular disproportion in utero predict outcome and pulmonary hypoplasia? Intensive Care Med. 1997. 23:10062–10069.
5. Estimating disease severity of congenital diaphragmatic hernia in the first 5 minutes of life: the Congenital Diaphragmatic Hernia Study Group. J Pediatr Surg. 2001. 36:141–145.
6. Downard CD, Jaksic T, Garza JJ, Dzakovic A, Nemes L, Jennings RW, Wilson JM. Analysis of an improved survival rate for congenital diaphragmatic hernia. J Pediatr Surg. 2003. 38:729–732.
7. Javid PJ, Jaksic T, Skarsgard ED, Lee S. Canadian Neonatal Network. Survival rate in congenital diaphragmatic hernia: the experience of the Canadian Neonatal Network. J Pediatr Surg. 2004. 39:657–660.
8. Migliazza L, Bellan C, Alberti D, Auriemma A, Burgio G, Locatelli G, Colombo A. Retrospective study of 111 cases of congenital diaphragmatic hernia treated with early high-frequency oscillatory ventilation and presurgical stabilization. J Pediatr Surg. 2007. 42:1526–1532.
9. Frenckner B, Ehrén H, Granholm T, Lindén V, Palmér K. Improved results in patients who have congenital diaphragmatic hernia using preoperative stabilization, extracorporeal membrane oxygenation, and delayed surgery. J Pediatr Surg. 1997. 32:1185–1189.
10. Numanoglu A, Morrison C, Rode H. Prediction of outcome in congenital diaphragmatic hernia. Pediatr Surg Int. 1998. 13:564–568.
11. Deprest J, Jani J, Van Schoubroeck D, Cannie M, Gallot D, Dymarkowski S, Fryns JP, Naulaers G, Gratacos E, Nicolaides K. Current consequences of prenatal diagnosis of congenital diaphragmatic hernia. J Pediatr Surg. 2006. 41:423–430.
12. Okuyama H, Kubota A, Oue T, Kuroda S, Ikegami R, Kamiyama M, Kitayama Y, Yagi M. Inhaled nitric oxide with early surgery improves the outcome of antenatally diagnosed congenital diaphragmatic hernia. J Pediatr Surg. 2002. 37:1188–1190.
13. Beck C, Alkasi O, Nikischin W, Engler S, Caliebe A, Leuschner I, von Kaisenberg CS. Congenital diaphragmatic hernia, etiology and management, a 10-year analysis of a single center. Arch Gynecol Obstet. 2008. 277:55–63.
14. Datin-Dorriere V, Rouzies S, Taupin P, Walter-Nicolet E, Benachi A, Sonigo P, Mitanchez D. Prenatal prognosis in isolated congenital diaphragmatic hernia. Am J Obstet Gynecol. 2008. 198:80.e1–80.e5.
15. Skari H, Bjornland K, Frenckner B, Friberg LG, Heikkinen M, Hurme T, Loe B, Mollerlokken G, Nielsen OH, Qvist N, et al. Congenital diaphragmatic hernia in Scandinavia from 1995 to 1998: predictors of mortality. J Pediatr Surg. 2002. 37:1269–1275.
16. Datin-Dorriere V, Walter-Nicolet E, Rousseau V, Taupin P, Benachi A, Parat S, Hubert P, Revillon Y, Mitanchez D. Experience in the management of eighty-two newborns with congenital diaphragmatic hernia treated with high-frequency oscillatory ventilation and delayed surgery without the use of extracorporeal membrane oxygenation. J Intensive Care Med. 2008. 23:128–135.
17. Shanbhogue LK, Tam PK, Ninan G, Lloyd DA. Preoperative stabilisation in congenital diaphragmatic hernia. Arch Dis Child. 1990. 65:1043–1044.
18. Fumino S, Shimotake T, Kume Y, Tsuda T, Aoi S, Kimura O, Deguchi E, Iwai N. A clinical analysis of prognostic parameters of survival in children with congenital diaphragmatic hernia. Eur J Pediatr Surg. 2005. 15:399–403.
19. Bohn D, Tamura M, Perrin D, Barker G, Rabinovitch M. Ventilatory predictors of pulmonary hypoplasia in congenital diaphragmatic hernia, confirmed by morphologic assessment. J Pediatr. 1987. 111:423–431.
20. Bohn D. Blood gas and ventilatory parameters in predicting survival in congenital diaphragmatic hernia. Pediatr Surg Int. 1987. 2:336–340.
21. Norden MA, Butt W, McDougall P. Predictors of survival for infants with congenital diaphragmatic hernia. J Pediatr Surg. 1994. 29:1442–1446.
22. O'Rourke PP, Vacanti JP, Crone RK, Fellows K, Lillehei C, Hougen TJ. Use of the postductal PaO2 as a predictor of pulmonary vascular hypoplasia in infants with congenital diaphragmatic hernia. J Pediatr Surg. 1988. 23:904–907.
23. Casaccia G, Ravà L, Bagolan P, di Ciommo VM. Predictors and statistical models in congenital diaphragmatic hernia. Pediatr Surg Int. 2008. 24:411–414.
24. Bohn DJ, James I, Filler RM, Ein SH, Wesson DE, Shandling B, Stephens C, Barker GA. The relationship between PaCO2 and ventilation parameters in predicting survival in congenital diaphragmatic hernia. J Pediatr Surg. 1984. 19:666–671.
25. Hoffman SB, Massaro AN, Gingalewski C, Short BL. Survival in congenital diaphragmatic hernia: use of predictive equations in the ECMO population. Neonatology. 2011. 99:258–265.
26. Kim DH, Park JD, Kim HS, Shim SY, Kim EK, Kim BI, Choi JH, Park GW. Survival rate changes in neonates with congenital diaphragmatic hernia and its contributing factors. J Korean Med Sci. 2007. 22:687–692.
27. Kim SH, Cho YH, Ryu JH. Clinical study of congenital diaphragmatic diseases in neonates and infants. J Korean Assoc Pediatr Surg. 2010. 16:143–153.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download