Abstract
Compared with ST elevation myocardial infarction (STEMI), long-term outcomes are known to be worse in patients with unstable angina/non-STEMI (UA/NSTEMI), which might be related to the worse health status of patients with UA/STEMI. In patients with UA/NSTEMI and STEMI underwent percutaneous coronary intervention (PCI), angina-specific and general health-related quality-of-life (HRQOL) was investigated at baseline and at 30 days after PCI. Patients with UA/NSTEMI were older and had higher frequencies in female, diabetes and hypertension. After PCI, both angina-specific and general HRQOL scores were improved, but improvement was much more frequent in angina-related HRQOL of patients with UA/NSTEMI than those with STEMI (44.2% vs 36.8%, P < 0.001). Improvement was less common in general HRQOL. At 30-days after PCI, angina-specific HRQOL of the patients with UA/NSTEMI was comparable to those with STEMI (56.1 ± 18.6 vs 56.6 ± 18.7, P = 0.521), but general HRQOL was significantly lower (0.86 ± 0.21 vs 0.89 ± 0.17, P = 0.001) after adjusting baseline characteristics (P < 0.001). In conclusion, the general health status of those with UA/NSTEMI was not good even after optimal PCI. In addition to angina-specific therapy, comprehensive supportive care would be needed to improve the general health status of acute coronary syndrome survivors.
Compared to ST elevation myocardial infarction (STEMI), unstable angina and non-ST elevation myocardial infarction (UA/NSTEMI) show lower early mortality, but the long-term prognosis of these conditions is known to be worse (1-5). As the patients with UA/NSTEMI tend to be older and have more extensive coronary disease and more co-morbidities compared with those with STEMI (1), their health status would be so worse to be related to adverse long-term clinical outcome.
Health-related quality of life (HRQOL) scoring systems have been used as the objective measurement of performance status in various cardiovascular diseases (6-9). Although the role of percutaneous coronary intervention (PCI) in chronic stable angina is well established as it alleviates ischemic symptoms and improves quality of life (10, 11), quality-of-life has been relatively ignored in the management of acute coronary syndrome (ACS) because mortality reduction is the primary goal of treatment of ACS.
Our hypothesis is that HRQOL status would be worse in patients with UA/NSTEMI compared with STEMI. To elucidate the relationship between the change of health status and clinical factors, we investigated the HRQOL of survivors of ACS who had been treated with PCI.
We designed the Korean multicenter survey of health status outcomes after percutaneous coronary angioplasty (MUSTANG) study to invest HRQOL status for ACS patients treated with optimal PCI (12). From September 2009 to July 2010, consecutive patients were enrolled prospectively from 48 hospitals. Patients were considered eligible if they presented with UA/NSTEMI or STEMI and underwent timely PCI. Exclusion criteria were failure to achieve optimal reperfusion, delayed treatment in patients with STEMI (PCI done ≥ 12 hr after the onset of symptoms), inability to answer the questionnaires to assess health status or unwillingness to provide written informed consent.
Patients were diagnosed and managed following the current practice guidelines at the discretion of the attending physicians (13-15). Decision to refer to PCI was also at the discretion of the attending physician. A previous cardiovascular event was defined as a past history of myocardial infarction, PCI, coronary artery bypass graft surgery, or stroke. Patients were followed up for 30 days after the index PCI. Major adverse clinical events were defined as one or more of following: cardiovascular or noncardiovascular related death, non-fatal myocardial infarction, non-fatal stroke, recurrent significant angina requiring hospital admission and target vessel revascularization.
Baseline health status data were acquired directly from the patients within 24 hr after PCI through an in-depth individual interview conducted by trained personnel. The second measures were acquired at 30 days after the index PCI during the scheduled visits or by telephone interview. Two types of standardized written questionnaires were used: the Seattle Angina Questionnaire (SAQ) and the Euro Quality of Life 5-Dimensional Classification (EQ-5D) (16, 17). The original version SAQ tool is a 19-item questionnaire that is composed of five subscales of disease-specific health status for patients with coronary artery disease. We used physical limitation, angina frequency and quality-of-life (SAQ QOL) subscales. The scores of each subscale ranged from 0 to 100, where higher scores indicated better health status. The EQ-5D is a 5-item questionnaire that is composed of 5 subscales of general health status, that is, mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Scores of each subscale were converted to a summary index (EQ-5D index) that ranged from 0 (worst possible health state or death) to 1 (best possible health state).
The primary endpoint was the score on the SAQ QOL subscale or the EQ-5D index at 30 days after index PCI. Significant improvement in HRQOL was defined as an increase of ≥ 10 points on the SAQ QOL and an increase of ≥ 0.2 points on the EQ-5D index (18). The secondary endpoints were the score on each of the three subscales of SAQ and the EQ-5D index, and the interval changes of scores (ΔHRQOL) between each measurement.
Baseline clinical and demographic characteristics and HRQOL outcomes were analyzed according to the clinical diagnosis of UA/NSTEMI and STEMI. Continuous data were presented as the mean ± SD. Frequency data were presented as the number and percent. Differences between the clinical diagnosis groups were compared using Student's t-test for continuous data and the chi-square test for frequency data. Independent factors of STEMI were determined by using logistic regression analysis. Models included baseline characteristics and medications, and the results of stepwise variable selection were presented. Interval changes of each subscale of HRQOL from baseline to 30 days after PCI (ΔHRQOL) were compared using the paired t-test. Independent predictors of the 30-day HRQOL and ΔHRQOL were determined by using multiple linear regression analysis. Baseline characteristics and medications were included in multivariate model, and the results were presented as the beta coefficient (β), standard error (SE) and their 95% confidence interval (CI). To adjust for the effect of various clinical factors on the 30-day EQ-5D index scores between the patients with UA/NSTEMI and STEMI, general linear model was constructed. Clinical and demographic variables were added sequentially to the model. Every time each variable was added to the model, the mean EQ-5D index scores of both diagnosis groups were compared, and the contribution of the variable was assessed by the change in the coefficient of determination (R2). Missing values were imputed from the median. There was no substantial difference between analyses with a complete data set and those with a data set that consisted wholly of imputed values. Two-sided P values < 0.05 were considered statistically significant in all tests. All analyses were performed with the use of SPSS for Windows software, version 17.0 (SPSS Inc, Chicago, IL, USA).
The local institutional review board of each individual center approved the study protocol. All patients enrolled in the study offered written informed consent. The data were collected by the investigators at each hospital and analyzed by independent researchers. All authors had approved and vouched for the accuracy and completeness of the contents.
Among 3,577 patients recruited, data from 3,362 patients were analyzed. Incomplete data from 215 patients were excluded. Major adverse clinical events occurred in 52 patients during the observation period. The incidence of ACS reached a peak in the sixth decades in males, and the eighth decades in females. In STEMI, the proportion of males below 70 yr old was high compared with the females.
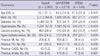
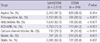
Baseline characteristics according to the clinical diagnosis are listed in Table 1. The patients with UA/NSTEMI were older and showed higher frequencies in female sex, diabetes and hypertension compared with those with STEMI. Independent variables associated with STEMI were younger age (OR, 0.992; 95% CI, 0.984-1.000, P = 0.048), male sex (OR, 1.260; 95% CI, 1.024-1.550, P = 0.029), current smoking status (OR, 1.951; 95% CI, 1.619-2.351, P < 0.001), absence of diabetes (OR, 0.800; 95% CI, 0.664-0.965, P = 0.020), hypertension (OR, 0.593; 95% CI, 0.500-0.703, P < 0.001) and previous history of major cardiovascular events (OR, 0.571; 95% CI, 0.458-0.713, P < 0.001). The medications at 30 days according to the clinical diagnostic groups are shown in Table 2. Beta blockers, and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers were administered more frequently in patients with STEMI than those with UA/NSTEMI (P < 0.001).
The rate of response for the 30-day HRQOL data was 94%. The unadjusted scores of HRQOLs acquired at the baseline, and at the 30th day after PCI, and the interval change (Δ) between the two observation periods are shown in Fig. 1. Both of the anginaspecific and general HRQOL were improved significantly at 30 days after PCI.
For angina-specific HRQOL status, the baseline scores of all three SAQ subscales were reported as significantly lower in patients with UA/NSTEMI than in those with STEMI. Mean ± SD were 75.2 ± 22.8 and 83.1 ± 22.4 (P < 0.001) for the SAQ physical-limitation subscale, 67.4 ± 26.2 and 81.0 ± 22.1 (P < 0.001) for the SAQ angina-frequency subscale, and 45.0 ± 19.0 and 50.1 ± 20.5 (P < 0.001) for the SAQ QOL subscale in the UA/NSTEMI and STEMI groups, respectively. The degree of improvement (Δ) was significantly higher in the UA/NSTEMI group: mean ± SD change were 13.0 ± 21.5 and 6.9 ± 21.3 (P < 0.001) for the ΔSAQ physical-limitation subscale, 23.0 ± 28.4 and 11.6 ± 24.1 (P < 0.001) for the ΔSAQ angina-frequency subscale, and 11.2 ± 22.7 and 6.5 ± 23.1 (P < 0.001) for the ΔSAQ QOL subscale in the UA/NSTEMI and STEMI groups, respectively. At day 30, SAQ QOL was comparable in two groups (56.1 ± 18.6 vs 56.6 ± 18.7, P = 0.521).
The number of patients in the UA/NSTEMI group who showed significant improvement (≥ 10 points) in the SAQ QOL subscale (ΔSAQ QOL) was higher (36.8% vs 44.2%, P < 0.001, Fig. 2) than the STEMI group. In addition to the diagnosis of UA/NSTEMI (β = 3.60, SE 0.98, P < 0.001), factors predicting significant improvement in the ΔSAQ QOL were current smoking status (β = 3.14, SE 0.98, P = 0.001), and the usage of beta blockers (β = -2.17, SE 0.93, P = 0.020) and calcium channel blockers (β = 3.11, SE 1.04, P = 0.003).
In the subgroup analysis for the patients with UA/NSTEMI, independent factors predicting high 30-day QOL were age (β = 0.101, SE 0.039, P = 0.010), male sex (β = 2.421, SE 0.864, P = 0.005), and no usage of beta blocker (β = -2.863, SE 0.850, P = 0.001). For the STEMI group, no specific predictor was identified.
At the baseline, there was no significant difference in the unadjusted EQ-5D index between the UA/NSTEMI and STEMI groups. The mean ± SD unadjusted EQ-5D indices were 0.77 ± 0.27 and 0.78 ± 0.29, respectively (P = 0.207, Fig. 1). The baseline EQ-5D index showed independent correlation with age (β = -0.001, SE 0.001, P = 0.002), female sex (β = -0.071, SE 0.011, P < 0.001) and the presence of hypercholesterolemia (β = 0.028, SE 0.010, P = 0.014). At 30 days after PCI, the EQ-5D index were lower in patients with UA/NSTEMI than in STEMI; the mean ± SD EQ-5D indices were 0.86 ± 0.21 and 0.89 ± 0.17, respectively (P = 0.001). In patients with UA/NSTEMI, independent predictors for the 30-day EQ-5D index were age (β = -0.002, SE 0.001, P < 0.001), male sex (β = 0.051, SE 0.010, P < 0.001), a history of cardiovascular events (β = -0.022, SE 0.010, P = 0.030) and diabetes (β = -0.022, SE 0.009, P = 0.021).
Compared with the SAQ QOL, the number of patients who showed significant improvement over 30 days in the EQ-5D index was fewer, and was not different between the two groups (Fig. 2).
Regarding the 30-day EQ-5D index between the UA/NSTEMI and STEMI groups, significant difference between the two groups was maintained in the process of sequential adjustment for each clinical factor and baseline HRQOL status (P < 0.001, Fig. 3). The addition of age in the model explained a 2.6% of the variance. The addition of the baseline SAQ QOL explained a further 7.4% of the variance.
HRQOL status in patients with ACS after PCI for resolving critical ischemia was was the primary concern of this study. The patients with UA/NSTEMI showed a lower general HRQOL status than those with STEMI even after optimal PCI. Unfavorable baseline clinical profiles of the patient with UA/NSTEMI are likely to be the cause, which is consistent with what was previously known (1-5). Poor general health status of patients with UA/NSTEMI might be related to their adverse long-term clinical outcomes.
Although most patients with ACS do not experience angina before index events, advanced atherosclerosis is often found. This is particularly true for patients with UA/NSTEMI, who usually have more extensive systemic atherosclerosis than those with STEMI (1). STEMI is the most severe form among ACS events, in which a gross rupture of plaque is accompanied by a storm of inflammatory and coagulative responses. Complete occlusion of a single vessel causing localized transmural infarction presents a dramatic change in the electrocardiogram, which is frequently observed in patients with STEMI. In UA/NSTEMI, which is often caused by small plaque erosion, irreversible myocardial necrosis per se tends to be less than STEMI due to several mechanisms including flow in the collateral circulation despite the much more extensive endangered. Even after optimal PCI, the improvement of performance status would be limited. Patients with UA/NSTEMI should be managed in the context of chronic heart failure as well as the ischemia-oriented acute stage care.
Advanced atherosclerosis is often associated with increased cardiovascular mortality in the setting of various non-cardiac chronic illnesses such as end-stage renal disease even in patients with considerable malnutrition (19). The heavier burden of systemic atherosclerosis is often associated with lower health status and poor long-term outcomes in such chronic diseases. Although there is controversy about the causal relationship, the poor general health status of patients with UA/NSTEMI may be attributable to the advanced atherosclerosis that is often found in chronic illnesses.
The significant improvement was evident in the angina-specific HRQOL, not in the general HRQOL. The degree of improvement in angina-related health status would be greater in patients with more extensive disease. Patients with UA/NSTEMI who have multiple coronary lesions would receive more benefit from PCI treatment than patients with an isolated lesion. As the severity of myocardial damage is less in UA/NSTEMI than in STEMI, one would expect the health status of patients with UA/NSTEMI to improve much more after optimal revascularization therapy compared with that of patients with STEMI. General health status, however, still remained significantly low in patients with UA/NSTEMI even after optimal PCI. Such findings may be the result of the limited health reserve of patients with UA/NSTEMI due to their advanced age, co-morbidities and heavier burden of atherosclerosis. Previous studies showed that the general health status as indicated by the EQ-5D score is a meaningful prognostic index (11, 20). Additional efforts such as rehabilitation and psychological support should be given to patients with UA/NSTEMI to improve their long-term outcome, particularly for those with low general health status.
Among medications, calcium channel blockers had a favorable effect on the improvement of angina-specific health status after PCI. Beta blockers, however, showed a negative impact. Although beta blockers are well-known to relieve the myocardial workload and reduce mortality in various cardiovascular diseases (21), the benefits of beta blockers might be limited in terms of the HRQOL in patients with UA/NSTEMI who underwent optimal PCI. Another explanation would be that beta blockers were intolerable because they were administrated without careful titration. Current treatment guidelines for heart failure recommend that beta blockers should be initiated with a low dose and titrated slowly over a sufficient period of time (21). The results might be different if our data had been obtained after a longer follow-up period. Further study is needed to clarify the effects of beta blockers on the QOL of patients who have received optimal revascularization.
The smoking paradox was observed in the present study. Current smoking status was an independent predictor of significant improvement in angina-related QOL in patients with UA/NSTEMI. Despite a controversy, apparent smoking paradox is now attributed to lower risk profile and more aggressive treatment (22, 23). We suppose the reason why our result is a matter of quality of life, not a matter of such "hard" outcomes. Smoking cessation after PCI could contribute to the improvement in health status.
The present study has several limitations. First of all, our results of patients with STEMI showing a better HRQOL outcome after PCI were based on the premise that patients with STEMI were treated optimally including timely PCI during the acute presentation. Our results cannot be applicable to patients with STEMI who did not receive appropriate treatment. In addition, as the study population consisted of patients who could answer questionnaires about HRQOL, our results cannot be extended to all ACS patients. The lower rates of adverse clinical events could be explained by such a context. The second is about the baseline health status. As ACS is a rapidly progressive disease, it is difficult to evaluate the past health status before the index event. Our results of the baseline HRQOL particularly for STEMI should be interpreted carefully. In addition, as HRQOL outcomes even after critical treatment are inherently dependent on baseline health status, most of the patients with a high HRQOL score at 30 days also had a higher baseline HRQOL. The 30-day health status would be even more greatly dependent on the baseline health status and clinical characteristics rather than on revascularization therapy, therefore the HRQOL results should be interpreted as a complex of results of treatments and clinical factors. Thirdly, 30 days might be short for patients with ACS to attain full recovery of their general health. Re-evaluation after a sufficient period of time would provide more valuable information. Lastly, the missing of some important clinical information such as angiographic data is a critical limitation. As the primary goal of this study is to investigate HRQOL status, we wholly focused to HRQOL data. That is why the minimum number of variables other than HRQOL was included at the stage of the study planning.
In conclusion, compared with the patients with STEMI, the general health status of those with UA/NSTEMI was not good even after optimal PCI. Although PCI is an effective treatment for acute myocardial ischemia, its benefit in general health status would not be sufficient. In addition to angina-specific therapy, comprehensive supportive care would be needed to improve the general health status of ACS survivors, which might improve long-term clinical outcome especially in patients with UA/NSTEMI.
Figures and Tables
 | Fig. 1Changes of HRQOL in each group of UA/NSTEMI and STEMI. In EQ-5D index, scores increased significantly after PCI. The degree of improvement (Δ) is not different in both groups (P = 0.337). In all three SAQ subscales, scores at 30 days after PCI are significantly higher compared with the baseline in both groups. The degree of improvement is higher in patients with UA/NSTEMI than with STEMI. |
 | Fig. 2The frequency of significant improvement in general and angina-specific HRQOL (ΔHRQOL). Compared with general HRQOL, significant improvement is more frequently observed in angina-specific HRQOL after PCI. Patients with UA/NSTEMI show much more improvement in angina-specific HRQOL than those with STEMI. |
 | Fig. 3Sequentially adjusted 30-day EQ-5D index. Mean EQ-5D indices of UA/NSTEMI and STEMI groups are sequentially adjusted by demographic and clinical variables, medications and baseline SAQ QOL. P value for final adjusted scores was < 0.01. CCB, calcium channel blocker; CV history, previous history of significant cardiovascular events. |
Notes
References
1. Cannon CP, Braunwald E. Unstable angina and non-ST elevation myocardial infarction. In : Bonow RO, Mann DL, Zipes DP, Libby P, editors. Braunwald's heart disease: a textbook of cardiovascular medicine. 9th ed. Philadelphia: Saunders Elsevier;2012. p. 1178–1209.
2. Bode C, Zirlik A. STEMI and NSTEMI: the dangerous brothers. Eur Heart J. 2007; 28:1403–1404.
3. Montalescot G, Dallongeville J, Van Belle E, Rouanet S, Baulac C, Degrandsart A, Vicaut E. OPERA Investigators. STEMI and NSTEMI: are they so different? 1 year outcomes in acute myocardial infarction as defined by the ESC/ACC definition (the OPERA registry). Eur Heart J. 2007; 28:1409–1417.
4. Chan MY, Sun JL, Newby LK, Shaw LK, Lin M, Peterson ED, Califf RM, Kong DF, Roe MT. Long-term mortality of patients undergoing cardiac catheterization for ST-elevation and non-ST-elevation myocardial infarction. Circulation. 2009; 119:3110–3117.
5. García-García C, Subirana I, Sala J, Bruguera J, Sanz G, Valle V, Arós F, Fiol M, Molina L, Serra J, et al. Long-term prognosis of first myocardial infarction according to the electrocardiographic pattern (ST elevation myocardial infarction, non-ST elevation myocardial infarction and nonclassified myocardial infarction) and revascularization procedures. Am J Cardiol. 2011; 108:1061–1067.
6. Spertus JA, Jones P, McDonell M, Fan V, Fihn SD. Health status predicts long-term outcome in outpatients with coronary disease. Circulation. 2002; 106:43–49.
7. Heidenreich PA, Spertus JA, Jones PG, Weintraub WS, Rumsfeld JS, Rathore SS, Peterson ED, Masoudi FA, Krumholz HM, Havranek EP, et al. Health status identifies heart failure outpatients at risk for hospitalization or death. J Am Coll Cardiol. 2006; 47:752–756.
8. Issa SM, Hoeks SE, Scholte op Reimer WJ, Van Gestel YR, Lenzen MJ, Verhagen HJ, Pedersen SS, Poldermans D. Health-related quality of life predicts long-term survival in patients with peripheral artery disease. Vasc Med. 2010; 15:163–169.
9. Guyatt GH. Measurement of health-related quality of life in heart failure. J Am Coll Cardiol. 1993; 22:185A–191A.
10. Weintraub WS, Spertus JA, Kolm P, Maron DJ, Zhang Z, Jurkovitz C, Zhang W, Hartigan PM, Lewis C, Veledar E, et al. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med. 2008; 359:677–687.
11. Dyer MT, Goldsmith KA, Sharples LS, Buxton MJ. A review of health utilities using the EQ-5D in studies of cardiovascular disease. Health Qual Life Outcomes. 2010; 8:13.
12. Kim MJ, Jeon DS, Gwon HC, Kim SJ, Chang K, Kim HS, Tahk SJ. Korean MUSTANG Investigators. Current statin usage for patients with acute coronary syndrome undergoing percutaneous coronary intervention: multicenter survey in Korea. Clin Cardiol. 2012; 35:700–706.
13. Wright RS, Anderson JL, Adams CD, Bridges CR, Casey DE Jr, Ettinger SM, Fesmire FM, Ganiats TG, Jneid H, Lincoff AM, et al. 2011 ACCF/AHA focused update of the guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction (updating the 2007 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011; 123:2022–2060.
14. Kushner FG, Hand M, Smith SC Jr, King SB 3rd, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE Jr, et al. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2009; 54:2205–2241.
15. King SB 3rd, Smith SC Jr, Hirshfeld JW Jr, Jacobs AK, Morrison DA, Williams DO, Feldman TE, Kern MJ, O'Neill WW, Schaff HV, et al. 2007 focused update of the ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: 2007 writing group to review new evidence and update the ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention, writing on behalf of the 2005 writing committee. Circulation. 2008; 117:261–295.
16. Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonell M, Fihn SD. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995; 25:333–341.
17. EuroQol: a new facility for the measurement of health-related quality of life: the EuroQol Group. Health Policy. 1990; 16:199–208.
18. Wyrwich KW, Spertus JA, Kroenke K, Tierney WM, Babu AN, Wolinsky FD. Heart Disease Expert Panel. Clinically important differences in health status for patients with heart disease: an expert consensus panel report. Am Heart J. 2004; 147:615–622.
19. Pecoits-Filho R, Lindholm B, Stenvinkel P. The malnutrition, inflammation, and atherosclerosis (MIA) syndrome: the heart of the matter. Nephrol Dial Transplant. 2002; 17:28–31.
20. Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001; 33:337–343.
21. Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, et al. 2009 focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009; 119:e391–e479.
22. Aune E, Røislien J, Mathisen M, Thelle DS, Otterstad JE. The "smoker's paradox" in patients with acute coronary syndrome: a systematic review. BMC Med. 2011; 9:97.
23. Wakabayashi K, Romaguera R, Laynez-Carnicero A, Maluenda G, Ben-Dor I, Sardi G, Gaglia MA Jr, Mahmoudi M, Gonzalez MA, Delhaye C, et al. Impact of smoking on acute phase outcomes of myocardial infarction. Coron Artery Dis. 2011; 22:217–222.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download