Abstract
Genetic susceptibility is involved in the pathogenesis of vitiligo. Association studies with a whole genome-based approach instead of a single or a few candidate genes may be useful for discovering new susceptible genes. Although the etiology of non-segmental and segmental types is different, the association between gene polymorphisms and vitiligo has been reported, without defining types or in non-segmental type. Whole genome-based single nucleotide polymorphisms (SNPs) were examined in patients with non-segmental and segmental types of vitiligo using the Affymetrix GeneChip 500K mapping array, and 10 functional classes of significant SNPs were selected. Genotyping and data analysis of selected 10 SNPs was performed using real-time PCR. Genotype and allele frequencies were significantly different between both types of vitiligo and three of the target SNPs, DNAH5 (rs2277046), STRN3 (rs2273171), and KIAA1005 (rs3213758). A stronger association was suggested between the mutation in KIAA1005 (rs3213758) and the segmental type compared to the non-segmental type of vitiligo. DNAH5 (rs2277046), STRN3 (rs2273171), and KIAA1005 (rs3213758) may be new vitiligo-related SNPs in Korean patients, either non-segmental or segmental type.
Vitiligo is an acquired depigmentary disorder of the skin. Although the etiology is unclear, the melanocytes involved in vitiligo are genetically susceptible and vulnerable to extracellular insults. Identification of genes involved in susceptibility to vitiligo has been attempted by association studies of candidate genes, which related to pathogenesis of non-segmental vitiligo including autoimmunity (1-8). However, genetics of vitiligo is characterized by incomplete penetrance, multiple susceptibility loci and genetic heterogeneity. Therefore, association studies with a whole genome-based approach instead of single or a few candidate genes may be useful to discover new susceptible genes. With completion of the human genome sequencing, there is a focus on developing new sequencing methodologies considering read length, thorough-put, and cost (9). A technical improvement in whole genome amplification with small amount of genomic DNA has been adopted for single nucleotide polymorphism (SNP) analysis (10). Recently, genome-wide association analysis has been attempted in vitiligo, with identification of genes including X-box binding protein 1 (XBP1) (11), SMOC2 (12), and TYR (13). A study could be conducted with a unique isolated population with elevated prevalence of generalized vitiligo and other autoimmune disease, which may provide a condition for detection of susceptible alleles with smaller sample sizes (12). However, studies have frequently been done with independent patients and controls (11, 13).
There is a consensus that vitiligo should be classified into segmental and non-segmental vitiligo forms based on clinical manifestations (14). The etiology of each type is considered to be distinct, although the association between segmental and non-segmental vitiligo has been reported. Nevertheless, the association between gene polymorphisms and vitiligo has been reported without defining types. In cases in which the type has been clarified, the association has usually been identified in non-segmental form.
A genome-wide association study was conducted in Korean patients with vitiligo, although the whole genome SNP analysis was performed in a very small number of patients. Functional classes of significant SNPs were validated by genotyping patients and independent healthy controls. Association between SNPs and vitiligo types was examined.
Twenty patients with non-segmental vitiligo were examined for whole genome-based SNPs. In total, 163 Korean patients with vitiligo were included to validate the 10 selected target SNPs in this study. A total of 113 cases were non-segmental, and 50 were segmental. An additional 97 patients with non-segmental (71 patients) and segmental vitiligo (26 patients) were added, resulting in 184 patients with the non-segmental and 76 with the segmental type to analyze the association between the three significant gene mutations and either type of vitiligo. In the 184 non-segmental and 76 segmental types, 86 and 27 patients were male, and 98 and 49 were female, respectively. Their ages ranged from 5 to 81 yr (mean, 40.1 yr) and 4 to 70 yr (mean, 23.6 yr), respectively. The control group included 192 healthy individuals (82 males and 110 females), with ages between 30 and 80 yr (mean, 50.0 yr).
Genomic DNA was isolated from peripheral blood leukocytes using the GenEX Genomic kit (Geneall, Seoul, Korea). Whole genome-based SNPs were examined using 2 µg of the genomic DNA from 20 patients with non-segmental vitiligo. The Affymetrix GeneChip 500K mapping array, which contained 500,568 probes, was used for the genome-wide association analysis. The genotypes were determined using the BRLMM algorithm. Before applying the algorithm, whole genome-based SNPs from 44 individuals offered by the Affymetrix were put together for the genotype calling to compensate for the small number of patients. The rates of mismatch between the genotyping from 20 patients and that from 20 patients plus the 44 individuals ranged from 0.14 to 0.39%. The genotype calls from 20 patients with vitiligo were compared with SNPs from 192 Korean healthy controls. All SNPs with a call rate less than 0.5, missing genotype frequency more than 0.5, and minor allele frequency less than 0.01 were removed with any monomorphic SNP. Any SNP with a P value less than 0.0001 in Hardy-Weinberg equilibrium test was also removed to analyze valid SNPs. Risk alleles were analyzed by the chi-square test using dominant, recessive, co-dominant, and additive genetic models. Significant SNPs were chosen by the level of significance which was either α = 0.001 or α = 0.01 with multiple test correction, a Bonferroni method.
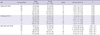
The number of significant SNPs was 114. They were divided into eight functional classes, such as non-synonymous, synonymous, mRNA UTR, intron, locus region, in-gene, intergenic, and unknown. The number of non-synonymous SNPs was eight, which were selected as the target SNPs. The SNPs within the linkage disequilibrium (LD) block, which included non-synonymous, synonymous or mRNA UTR SNPs, were also examined and seven significant SNPs were detected. Two (rs17035120 and rs2588400) of the seven SNPs were already included as target SNPs. One SNP (rs3763979) with a function class of synonymous and the other (rs1444216) with a function class of in-gene were added to the list of target SNPs, resulting in a total of 10 target SNPs (Table 1).
The real time-polymerase chain reaction (PCR) using genomic DNA from patients with vitiligo and healthy controls was performed to examine the association between non-segmental or segmental vitiligo, the 10 target SNPs, and the three significant SNPs. 10 ng of each genomic DNA was mixed with 20 µL of reaction mixture containing 1.0 µL of reaction mix, 2.0 µL of Fast-Start DNA master, and 1.6 µL of MgCl2. Real-time PCR was done automatically using specific primers and probe included in the LightSNiP kit (TIB MOLBIOL, Berlin, Germany) with a LightCycler 480 Instrument (Roche, Mannheim, Germany). The Light-SNiP kit was designed as an individual SNP base by TIB MOLBIOL.
All statistical tests were two-sided, and the level of significance was 0.05. Substitution of missing values was not performed. Data from both vitiligo and healthy control groups were compared using the chi-square test. One allele association analysis and four genotype association analyses were performed using dominant, recessive, co-dominant, and additive genetic models. Odd ratios were calculated by chi-square test from a 2 × 2 contingency table. All output was produced using SPSS version 9.1 (SPSS Inc., Chicago, IL, USA).
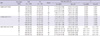
The genotype frequencies of the 10 target SNPs were compared between vitiligo patients and normal healthy controls. The genotype and allele frequencies showed a significant difference in three of the target SNPs, such as DNAH5 (rs2277046), STRN3 (rs2273171), and KIAA1005 (rs3213758) in all four different genetic models (Table 2), regardless of the vitiligo type difference (Table 3), although the STRN3 genotype was not significantly different in the dominant model. In DNAH5 (dynein axonemal heavy chain5), the genotype and allele frequencies of 12658 A > G (4220 Thr > Ala) in patients with vitiligo were significantly different from those in healthy controls. The AA genotype frequency was lower, whereas GG was higher in vitiligo patients, suggesting that G allele at the DNAH A12658G polymorphism increased susceptibility to vitiligo. The genotype and allele frequencies of STRN3 (striatin calmodulin binding protein 3) 1376 T > C (387 Asn > Ser) were also significantly different between the patients and healthy controls. The TT genotype was less frequent, whereas CC was more common in patients than controls, indicating that the C allele at the STRN3 T1376C may increase susceptibility to vitiligo. In KIAA1005, the genotype and allele frequencies of 3854 G > A (1264 Asp > Asn) in vitiligo patients were significantly different compared to healthy controls. The GG frequency was lower, whereas AA frequency was higher in vitiligo, showing an A allele at the KIAA1005 G3854A may increase susceptibility to vitiligo.
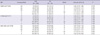
The genotype and, particularly, allele frequencies of DNAH5 12658 A > G and STRN3 1376 T > C were not significantly different between the non-segmental and segmental forms in all four models (Table 3), whereas those of KIAA1005 3854 G > A was different (Table 3). Therefore, a direct comparison between non-segmental and segmental vitiligo was performed. In fact, the frequency of allele A in the KIAA1005 gene was significantly (P = 0.025) higher in the segmental compared to that in nonsegmental vitiligo, although the genotype frequency suggested only a tendency for statistical significance in recessive (P = 0.058), co-dominant (P = 0.055), and additive (P = 0.060) models (Table 4).
This genome-wide association study in Korean patients with vitiligo identified that three new SNPs, such as DNAH5 (rs2277046), STRN3 (rs2273171), and KIAA1005 (rs3213758), were associated with increased susceptibility to both non-segmental and segmental types of vitiligo (Table 2, 3), although the number of patients was too small to identify the actual number of significant SNPs.
Although an association with other variants in DNAH5, STRN3, and KIAA1005 with particular diseases has been reported (15-21), a clinical association of the SNPs, such as DNAH5 rs2277046, STRN3 rs2273171, and KIAA1005 rs3213758, has not been revealed. The DNAH5 gene is located in the coding axon of chromosome 5p15.2. The A12658G (rs2277046) variant had an amino acid threonine residue (Thr4220) changed to an alanine residue (Ala4220). Mutation in the DNAH5 is found in patients with primary ciliary dyskinesia (PCD) (15), a rare disease transmitted as an autosomal recessive trait and characterized by recurrent airway infections due to abnormal ciliary structure and function. Primary defects in the structure and function of sensory and motile cilia result in multiple ciliopathies (16). Multiple variants of the KIAA1005 gene, which is located in coding exon of chromosome 16q12.2 and called as a retinitis pigmentosa GTPase regulator-interacting protein 1-like (RPGRIP1L) gene, have also been associated with certain clinical manifestations, particularly ciliopathies as in DNAH5 with neurological, renal and ocular manifestations (17). The D1264N (rs3213758) mutation had the amino acid aspartic acid residue (Asp1264) changed to asparagine (Asn1264). Since cilia may be a sensitive and easily damaged organelle (18), performing diverse biological functions as hair-like structures extending from the cell membrane, certain defects of the cilia in either melanocytes or keratinocytes may relate to vitiligo development, although further studies are required. STRN3 gene locates in the coding exon of chromosome 14q12. The STRN3 rs2273171 variant induces the amino acid asparagine residue (Asn387) to change to a serine residue (Ser387). Striatin is an intracellular protein characterized by four protein-protein interaction domains, a caveolin-binding domain, a coiled-coil structure, a Ca2+-calmodulin (CaM)-binding domain, and a WD repeat domain (19). Results including the defective calcium uptake in both keratinocytes and melanocytes (20) and the activated nitric oxide synthases by increased levels of intracellular Ca2+ via calmodulin (21), suggest an association of striatin with vitiligo development.
In general, segmental vitiligo has been classified separately from other forms of vitiligo including non-segmental vitiligo. An association between gene polymorphisms and vitiligo has been reported for non-segmental vitiligo (1-4). In this study, the association was separately analyzed both in non-segmental and in segmental forms. The association did not differ in either type of vitiligo (Table 3), although a stronger association between KIAA1005 (rs3213758) and segmental vitiligo was suggested (Tables 3 and 4). Neural dysfunction in the pathogenesis of segmental vitiligo and KIAA genes for organization and function in the brain (22) may support this association. However, increasing clinical and etiological evidence suggests an association between segmental vitiligo and non-segmental vitiligo.
Collectively, our genome-wide association study in Korean patients with vitiligo resulted in three new vitiligo-related SNPs, such as DNAH5 (rs2277046), STRN3 (rs2273171), and KIAA1005 (rs3213758), although a stronger association between KIAA1005 (rs3213758) and segmental compared to the non-segmental type of vitiligo was suggested. Future functional studies of these SNPs may contribute to the understanding of vitiligo pathogenesis.
Figures and Tables
Table 2
Genotype and allele frequencies of each gene polymorphism in the vitiligo patients and the healthy controls
Notes
References
1. Nath SK, Kelly JA, Namjou B, Lam T, Bruner GR, Scofield RH, Aston CE, Harley JB. Evidence for a susceptibility gene, SLEV1, on chromosome 17p13 in families with vitiligo-related systemic lupus erythematosus. Am J Hum Genet. 2001. 69:1401–1406.
2. Cantón I, Akhtar S, Gavalas NG, Gawkrodger DJ, Blomhoff A, Watson PF, Weetman AP, Kemp EH. A single-nucleotide polymorphism in the gene encoding lymphoid protein tyrosine phosphatase (PTPN22) confers susceptibility to generalised vitiligo. Genes Immun. 2005. 6:584–587.
3. LaBerge GS, Bennett DC, Fain PR, Spritz RA. PTPN22 is genetically associated with risk of generalized vitiligo, but CTLA4 is not. J Invest Dermatol. 2008. 128:1757–1762.
4. Jin Y, Birlea SA, Fain PR, Spritz RA. Genetic variations in NALP1 are associated with generalized vitiligo in a Romanian population. J Invest Dermatol. 2007. 127:2558–2562.
5. Casp CB, She JX, McCormack WT. Genetic association of the catalase gene (CAT) with vitiligo susceptibility. Pigment Cell Res. 2002. 15:62–66.
6. Gavalas NG, Akhtar S, Gawkrodger DJ, Watson PF, Weetman AP, Kemp EH. Analysis of allelic variants in the catalase gene in patients with the skin depigmenting disorder vitiligo. Biochem Biophys Res Commun. 2006. 345:1586–1591.
7. Li M, Sun D, Li C, Zhang Z, Gao L, Li K, Li H, Gao T. Functional polymorphisms of the FAS gene associated with risk of vitiligo in Chinese populations: a case-control analysis. J Invest Dermatol. 2008. 128:2820–2824.
8. Namian AM, Shahbaz S, Salmanpoor R, Namazi MR, Dehghani F, Kamali-Sarvestani E. Association of interferon-gamma and tumor necrosis factor alpha polymorphisms with susceptibility to vitiligo in Iranian patients. Arch Dermatol Res. 2009. 301:21–25.
9. Chan EY. Advances in sequencing technology. Mutat Res. 2005. 573:13–40.
10. Bannai M, Higuchi K, Akesaka T, Furukawa M, Yamaoka M, Sato K, Tokunaga K. Single-nucleotide-polymorphism genotyping for whole-genome-amplified samples using automated fluorescence correlation spectroscopy. Anal Biochem. 2004. 327:215–221.
11. Ren Y, Yang S, Xu S, Gao M, Huang W, Gao T, Fang Q, Quan C, Zhang C, Sun L, et al. Genetic variation of promoter sequence modulates XBP1 expression and genetic risk for vitiligo. PLoS Genet. 2009. 5:e1000523.
12. Birlea SA, Gowan K, Fain PR, Spritz RA. Genome-wide association study of generalized vitiligo in an isolated European founder population identifies SMOC2, in close proximity to IDDM8. J Invest Dermatol. 2010. 130:798–803.
13. Jin Y, Birlea SA, Fain PR, Gowan K, Riccardi SL, Holland PJ, Mailloux CM, Sufit AJ, Hutton SM, Amadi-Myers A, et al. Variant of TYR and autoimmunity susceptibility loci in generalized vitiligo. N Engl J Med. 2010. 362:1686–1697.
14. Ezzedine K, Lim HW, Suzuki T, Katayama I, Hamzavi I, Lan CC, Goh BK, Anbar T, Silva de Castro C, Lee AY, et al. Revised classification/nomenclature of vitiligo and related issues: the Vitiligo Global Issues Consensus Conference. Pigment Cell Melanoma Res. 2012. 25:E1–E13.
15. Omran H, Häffner K, Völkel A, Kuehr J, Ketelsen UP, Ross UH, Konietzko N, Wienker T, Brandis M, Hildebrandt F. Homozygosity mapping of a gene locus for primary ciliary dyskinesia on chromosome 5p and identification of the heavy dynein chain DNAH5 as a candidate gene. Am J Respir Cell Mol Biol. 2000. 23:696–702.
16. Zariwala MA, Knowles MR, Omran H. Genetic defects in ciliary structure and function. Annu Rev Physiol. 2007. 69:423–450.
17. Delous M, Baala L, Salomon R, Laclef C, Vierkotten J, Tory K, Golzio C, Lacoste T, Besse L, Ozilou C, et al. The ciliary gene RPGRIP1L is mutated in cerebello-oculo-renal syndrome (Joubert syndrome type B) and Meckel syndrome. Nat Genet. 2007. 39:875–881.
18. Warfvinge K. Single cilia in human epidermis are susceptible to challenge. Acta Derm Venereol. 1995. 75:446–448.
19. Castets F, Rakitina T, Gaillard S, Moqrich A, Mattei MG, Monneron A. Zinedin, SG2NA, and striatin are calmodulin-binding, WD repeat proteins principally expressed in the brain. J Biol Chem. 2000. 275:19970–19977.
20. Schallreuter KU. Epidermal adrenergic signal transduction as part of the neuronal network in the human epidermis. J Investig Dermatol Symp Proc. 1997. 2:37–40.
21. Bruch-Gerharz D, Ruzicka T, Kolb-Bachofen V. Nitric oxide in human skin: current status and future prospects. J Invest Dermatol. 1998. 110:1–7.
22. Imai K, Kawai M, Tada M, Nagase T, Ohara O, Koga H. Temporal change in mKIAA gene expression during the early stage of retinoic acid-induced neurite outgrowth. Gene. 2005. 364:114–122.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download